Minimally Invasive Total Knee Arthroplasty
David Watson
Steven Haas
INDICATIONS
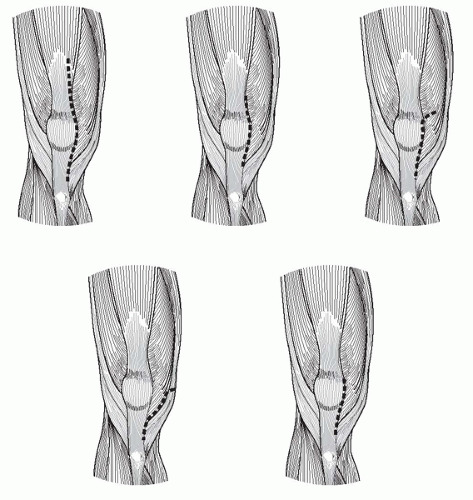
Innovative techniques and alteration in instrument design have facilitated the safe and accurate placement of a total knee arthroplasty (TKA) while utilizing smaller incisions and less dissection/disruption of the extensor mechanism and joint capsule. Several techniques have been popularized, including the mini-medial parapatellar, mini-subvastus, quadriceps-sparing, and mini-midvastus approaches with a unifying theme of minimal disruption of the extensor mechanism. These techniques were developed to minimize the surgical insult and allow for an earlier return to function and in no way alter the indications for TKA. Regardless of which particular minimally invasive surgical approach is used, the general philosophy and approaches to the knee are similar, and outcomes similar, despite only subtle variations in the arthrotomies and capsular incisions (Fig. 3-1).
The advantages of minimally invasive knee arthroplasty are as follows:
Earlier return of quadriceps function
Earlier return of motion
Improved flexion
Decreased postoperative narcotic usage
Improved cosmesis
Equal complication rate to standard techniques
TKA is a highly successful operation, rewarding for both the surgeon and patient when performed well, in well-selected individuals. It is indicated in the situation of significant disability arising from an underlying arthritic condition of the knee that has been refractory to nonoperative measures. Before surgical consideration, a patient should have an appropriate diagnosis and participated in a trial of conservative measures including activity modification, nonnarcotic analgesics/anti-inflammatory medication, physical therapy, and weight reduction when appropriate.
The decision to proceed with a minimally invasive technique depends on the surgeon, instrumentation, and patient factors.
Surgeon
Although the underlying principles of appropriate bony cuts and soft tissue balancing are unchanged, the techniques used in minimally invasive (MIS) TKA are different, and the execution of a well-placed and balanced knee is more technically demanding than the more traditional extensile arthrotomy. Specialized training sessions, in addition to a thorough understanding and technical mastery of standard knee arthroplasty techniques are recommended before attempting these techniques.
Instrumentation
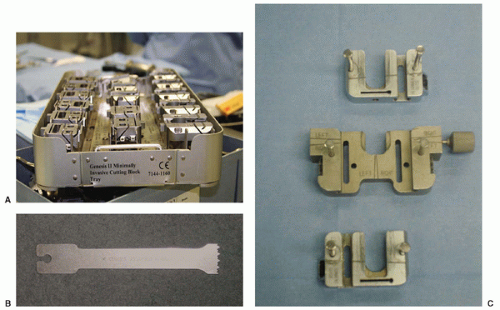
In the development of minimally invasive techniques, instrumentation was adapted to facilitate use through smaller operative windows. A minimally invasive set with significantly smaller, side-specific guides, and cutting blocks is very advantageous and certainly recommended if MIS TKA is to be undertaken. Specialized saw blades are also recommended (Fig. 3-2).
Patient
In the day of direct-to-consumer advertising and Internet access, patients often request MIS techniques. If the surgical expertise and appropriate instrumentation are available, I believe it is reasonable to proceed if the patient is an appropriate candidate. Although there are no absolute contraindications to MIS TKA, the relative contraindications are patient related. Patients, particularly those requesting the techniques, are advised that incisions are increased in size, and dissections are made more extensile at any time during the reconstruction should safety, visualization, or quality be felt to be compromised. Early in a surgeon’s experience, MIS approaches to the knee are typically reserved for the simplest of cases; as the surgeon’s experience and comfort level improve, the indications for MIS approaches expand.
Relative contraindications to MIS TKA are as follows:
Men with substantial quadriceps muscle mass
Men with very large bone dimensions
Significant obesity (body mass index [BMI] >40)
Severe coronal plane deformity
Flexion contracture >25 degrees
Passive flexion <80 degrees
Severe patella baja
Significant scarring of the quadriceps mechanism
Thin female patients tend to be the easiest candidates for MIS TKA, particularly those with a “loose knee” and an underdeveloped vastus medialis obliquus (VMO) inserting high on the patella. Patients with a well-developed VMO (muscular men) and those in whom the VMO inserts lower on the patella at a more oblique angle are more challenging and may warrant standard technique until considerable experience is gained.
Preoperative Planning
Planning proceeds as per standard knee arthroplasty. The author obtains standing anteroposterior (AP), lateral, flexed PA, and merchant views. Full-length views are not obtained unless otherwise indicated by history or physical examination. In cases of deformity, anticipating an appropriate valgus cut angle and height of tibial resection can be helpful.
TECHNIQUE
Positioning
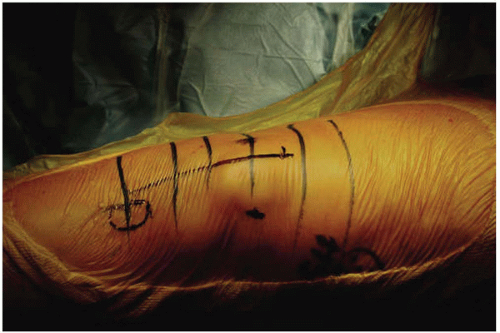
Appropriate leg positioning is crucial when performing minimally invasive TKA. I prefer to use a tourniquet if there is no contraindication, although it may be done without one. A sandbag is placed
under the drapes at the level of the opposite ankle so that the knee can sit flexed at approximately 70 to 90 degrees. The majority of the procedure is done in this position. Hyperflexion is sometimes required to prepare the proximal tibia and insert the definitive tibial tray. A lateral support is used so that the leg sits without being held by an assistant (Fig. 3-3).
under the drapes at the level of the opposite ankle so that the knee can sit flexed at approximately 70 to 90 degrees. The majority of the procedure is done in this position. Hyperflexion is sometimes required to prepare the proximal tibia and insert the definitive tibial tray. A lateral support is used so that the leg sits without being held by an assistant (Fig. 3-3).
Exposure
Landmarks for the skin incision are the borders of the patella and the tibial tubercle. These are marked, and a longitudinal incision line is drawn at the junction of the middle and medial thirds of the patella. The incision extends from 1 cm above the superior pole of the patella to the proximal half of the tibial tubercle on its medial side. A typical skin incision length is between 8.5 and 12 cm; however, the technique is not defined by incision length, and there should be no hesitation to extend this at any stage if there appears to be undue tension, especially at the distal apex of the incision (Fig. 3-4).
A medial arthrotomy is performed. This extends from the superior pole of the patella to the level of the tibial tubercle. We leave a 5-mm cuff of tissue adjacent to the tubercle to aid in closure later on. The VMO is identified, and an oblique split is made in the muscle in the line of its fibers at the level of the superior pole of the patella (Fig. 3-5).
The first centimeter of the muscle split is started sharply, but the remainder is performed bluntly with a finger, gently separating the muscle fibers. Performing the split completely by sharp dissection risks damaging the distal innervation of the vastus musculature. The muscle split is generally between 2 and 4 cm in length. We have found from experience that this usually does not propagate any further with this technique. The suprapatellar pouch is preserved except in cases of severe inflammatory disease.
With the knee extended, a subperiosteal dissection is carried around the medial pretibial border, releasing the meniscotibial attachments. The patella is then retracted laterally, and a partial excision of the infrapatellar fat pad is performed. We also excise the medial fat pad at this stage. Excision of the fat pad is a crucial maneuver at this point, as it releases a distal tether of the patella allowing for lateral subluxation. The tibial attachments of the anterior cruciate ligament and the anterior horn of the lateral meniscus are released. This allows placement of a thin bent Homan retractor laterally to sublux the patella. A small synovial window is made over the antero-lateral femoral cortex to aid in our initial anterior femoral resection.
In patients with tight extensor mechanisms, large patellae, or an abundance of patellar osteophytes, the patella can be cut first. Initial patellar resection is usually not required, however.
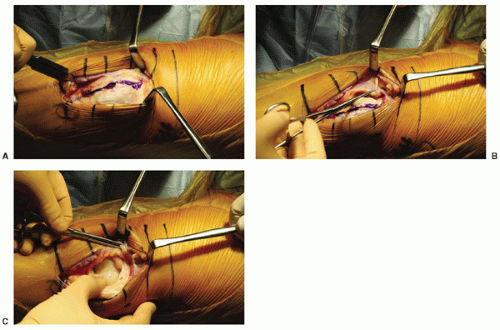 FIGURE 3-5 (A) The intended arthrotomy is depicted. A 5-mm cuff of tissue is left along the medial border of the patella for ease of repair. At the superior pole of the patella, the dissection turns medial and enters the VMO at a 45-degree angle. (B) The initial 1-cm split of the VMO is performed sharply. (C)
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|