Correction of Flexion Contractures in Total Knee Arthroplasty
Adolph V. Lombardi
Keith R. Berend
Bradley S. Ellison
INDICATIONS
The success of total knee arthroplasty (TKA) has been well established. The clinical success, however, depends on the surgical correction of the deformity, attainment of optimal mechanical alignment, and meticulous soft tissue balancing. Flexion contractures are inherent in the pathophysiology of severe articular degeneration of the knee, either as a consequence of previous traumatic injury, advanced osteoarthritis, or inflammatory arthritis. Commonly, flexion contractures are related to an inability to maintain full knee extension secondary to the presence of painful synovitis, large joint effusion, prominent osteophytes at the posterior aspect of the femoral condyles, posterior adhesive capsulitis, as well as contractures of the posterior capsule, cruciate ligaments, and hamstrings (1). Fixed flexion contractures affect the gait cycle at initial contact, midstance, and the terminal stance phases. To compensate for the flexed posture of the knee during gait, this disorder necessitates recruitment of the quadriceps, leading to additional energy expenditure (2,3). The pathologic gait pattern associated with a knee flexion contracture results in inefficient locomotion, accelerated fatigue, and compromises the clinical outcome of TKA.
To ensure optimal postoperative range of motion (ROM) and functional outcome, we believe that full correction of any flexion contracture should be performed at the time of surgical intervention. The specific approach depends on the degree of flexion contracture present, which is classified according to severity. A mild contracture is considered to be 15 degrees or less and is classified as grade I (Fig. 10-1). A moderate contracture is considered to be between 15 and 30 degrees and is classified as grade II. A severe contracture is considered to be greater than 30 degrees and is classified as grade III. Each grade requires a slightly different surgical approach, and accurately assessing the degree of flexion contracture will guide the surgeon as the contracture is addressed with a combination of soft tissue releases and bony resection.
CONTRAINDICATIONS
Although the surgical management of fixed flexion contracture in TKA is technically challenging and associated with a higher rate of complications, the technique can be performed reliably and is successful in providing improved postoperative function, ROM, and pain relief. One of the potential complications in correcting severe flexion contractures, especially in the setting of an associated valgus deformity, is peroneal nerve palsy. Fixed flexion contracture, however, regardless of severity, is not a contraindication to TKA, insofar as the patient meets all other criteria for surgery and does not have another identifiable contraindication for the operation.
PREOPERATIVE PREPARATION
Once the patient is determined to be a suitable candidate for TKA, a detailed assessment of coronal and sagittal deformity, flexion contracture, extensor lag, and preoperative ROM should be obtained. Accurate measurement of these patient-specific variables allows the surgeon to enter into an individualized discussion with each patient regarding surgical technique, clinical expectations, and associated risks and complications. When present, a flexion contracture can be classified according to severity as measured during clinical examination using a goniometer. A grade I contracture is considered mild and 15 degrees or less. A grade II contracture is considered moderate and between 15 and 30 degrees. A grade III contracture is considered severe and is greater than 30 degrees. With each increasing grade, there is a concomitant increase in the complexity of deformity.
Once the flexion contracture has been appropriately classified, the next step is to identify the structures contributing to the deformity, as determined by clinical examination and standard preoperative radiographic studies. Typically, standard radiographic views will reveal abnormalities in the bony anatomy, including prominent posterior osteophytes, condylar deficiency, and significant coronal or sagittal malalignment. Attention should be directed toward the bony deficiency of the posterior condyles that may affect rotation of the femoral component when using a measured resection technique or posterior referencing system. Occasionally, large bone deficits may require the use of augmentation with allograft or modular inserts. Additionally, various soft tissue structures commonly contribute to a flexion contracture, including an adherent or taut posterior capsule, as well as a contracted posterior cruciate ligament (PCL), collateral ligaments, and/or hamstrings. The authors believe that full correction of flexion contractures should be attempted at the time of surgical intervention and further suggest that the best chance of correction may only be obtained at the time of surgery. All components of the deformity must be addressed intraoperatively, and each grade of flexion contracture requires a slightly different surgical approach to soft tissue release, bony resection, and degree of prosthetic constraint.
As the severity of the flexion contracture increases, a corresponding amount of bony resection and soft tissue releases will be needed. To compensate for bone deficits and attenuated soft tissue structures, the surgeon may employ various options in prosthetic constraint for the chosen implant design. Thus, it is expected that with increased severity of flexion contracture, an increased level of
constraint in prosthetic design will be needed. Depending on the grade of flexion contracture, the authors have developed an algorithm based on pathologic criteria to assist in the decision to implant a posterior cruciate-retaining (PCR), posterior stabilized (PS), posterior stabilized constrained (PSC), or linked hinge component. Based on the preoperative evaluation, measures should be taken to ensure the necessary implants and accessories are available at the time of surgery.
constraint in prosthetic design will be needed. Depending on the grade of flexion contracture, the authors have developed an algorithm based on pathologic criteria to assist in the decision to implant a posterior cruciate-retaining (PCR), posterior stabilized (PS), posterior stabilized constrained (PSC), or linked hinge component. Based on the preoperative evaluation, measures should be taken to ensure the necessary implants and accessories are available at the time of surgery.
TECHNIQUE
Management of Flexion Contractures—An Algorithmic Approach
Once the decision to move forward with surgery has been made, and all the necessary preoperative plans have been developed and surgical implants and materials assembled, the patient will be escorted to the operative suite. A pneumatic tourniquet is applied to the proximal thigh and will be activated prior to incision. Following the use of regional anesthesia supplemented with mild sedation, the operative leg is prepared and draped in standard fashion. An anterior longitudinal midline skin incision is used beginning 4 to 6 cm proximal to the suprapatellar pole and extended distally to the medial border of the tibial tubercle. A medial parapatellar arthrotomy is performed allowing sufficient exposure of the medial and lateral condyles while everting the patella. Once adequate visualization is obtained, elementary correction of the coronal deformity with appropriate osteophyte removal and soft tissue release is performed.
The key to successful management of flexion contracture is addressing the contracture by a combination of soft tissue releases and bony resection to restore coronal and sagittal stability. Every effort should be undertaken to completely correct the flexion deformity during the operation while maintaining adequate stability and motion through meticulous soft tissue balancing. There are several different approaches to soft tissue balancing in TKA. The first approach is referred to as the classic Insall technique (1,4, 5, 6) and involves creating a balanced flexion gap by resecting the posterior condyles about a rotational axis that changes based on soft tissue balance. The corresponding extension gap is matched to the flexion gap via tensioning devices or spacer blocks. The second approach to soft tissue balancing is referred to as the measured resection technique (7,8) and involves replacing the exact thickness of resected bone from the distal femur and proximal tibia with a prosthetic implant of matched thickness. Assuming correct alignment of the resections, the knee is then balanced by ligamentous release. A third approach is a hybrid technique, which balances the knee with ligamentous releases first, and then the surgeon performs measured resections of the distal femur and proximal tibia. The flexion gap is then balanced with a tensioner device to establish femoral rotation (1).
Regardless which technique is used as the method of soft tissue balancing, the posterior recess of the knee should be the focus of attention. The posterior capsule should be released in all cases of flexion contracture and possibly in all primary TKAs, as this maneuver positively enhances final postoperative ROM (9). If the tightened capsule is not released and posterior osteophytes are not removed, then an erroneous distal femoral resection will be performed in an effort to obtain full extension and balanced flexion/extension gaps. An error of this kind can result in elevation of the joint line and midflexion instability, negatively affecting the function of an intact PCL and further altering patellofemoral kinematics.
Newer prosthetic designs allow for increased flexion, which is obtained by increasing the distance that the tibial insert travels behind the femur before impinging on the posterior femur. These designs often require an increased posterior condyle resection, which should facilitate debridement of the posterior aspect of the knee, indirectly increasing correction of the fixed flexion deformity. Additionally, the posterior condyles of the femoral prosthesis do not edge load at higher angles. The propensity for a PS design to dislocate at higher flexion angles is reduced by these prosthetic design modifications. It may be possible to conceive that “high-flexion” prosthetic designs may allow for improved motion and facilitate the correction of fixed flexion contractures. Even when using a “high-flexion” prosthesis, meticulous soft tissue balancing and bony resection must still be performed (10). More importantly, if these designs are to be successful in allowing increased ROM, the posterior recess must be devoid of osteophytes, and the posterior capsule should be subperiosteally released from the femur.
Grade I Flexion Contracture
For contractures of 15 degrees or less, the decision between the implantation of either a PCR or PS device depends on the correctability of the deformity, surgeon preference, and competency of the PCL. Using the principles of measured resection, the distal femur and proximal tibia are cut with the
goal of obtaining appropriate alignment in the coronal and sagittal planes. The rotational alignment for the femur and tibia is determined by using the appropriate landmarks. For femoral landmarks, the anteroposterior axis, epicondylar axis, and posterior condylar axis are used. For tibial landmarks, the insertions of the PCL and patella tendon are used, along with a trial ROM.
goal of obtaining appropriate alignment in the coronal and sagittal planes. The rotational alignment for the femur and tibia is determined by using the appropriate landmarks. For femoral landmarks, the anteroposterior axis, epicondylar axis, and posterior condylar axis are used. For tibial landmarks, the insertions of the PCL and patella tendon are used, along with a trial ROM.
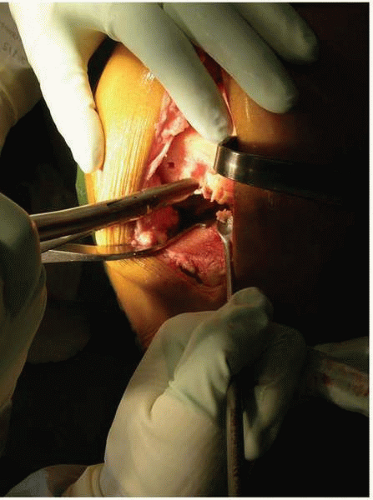
Removal of overhanging bone at the posterior femoral condyle and osteophytes at the posterior femoral condyle is mandatory to obtain full correction of flexion contracture (Fig. 10-2). An intramedullary rod may be used to elevate the femur and tense the posterior capsule while a Cobb elevator or dull curved 0.5-inch osteotome is used to establish a posterior recess. Alternatively, a specialized laminar spreader may be utilized to separate the condyles from the tibia and tense the posterior capsule, thereby facilitating a thorough debridement of the posterior capsule (Fig. 10-3). A trial reduction with PCR implants is performed to identify perceivable tension imbalances in the medial collateral ligament, lateral collateral ligament, and PCL, as well as symmetry of the flexion and extension gaps. If the extension gap is less than the flexion gap, further release of the




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree