Soft Tissue Balancing Technique for Posterior Stabilized Total Knee Arthroplasty
Hari P. Bezwada
Robert E. Booth Jr.
INDICATIONS
Total knee arthroplasty (TKA) is indicated for end-stage arthritis involving the knee. It is often tricompartmental in nature and may be the result of a variety of arthritides. The majority of knee arthroplasties are performed for “garden-variety” osteoarthritis; however, inflammatory arthritis, avascular necrosis, and posttraumatic arthritis are other conditions that can be treated with TKA. Knee arthroplasty is currently being performed in younger and higher-demand patients than in previous decades, with a decline in the average patient age. Obesity is commonplace. The majority of patients in our practice have a body mass index ≥30, with an evolving group of patients with a body mass index ≥50. Advanced tricompartmental arthritis is often associated with substantial deformity and reduced range of motion, both of which need to be addressed at the time of surgery. Many of these patients have also typically failed an attempt at nonoperative treatment, such as viscosupplementation, physical therapy, nonsteroidal anti-inflammatory medications, weight loss, and steroid injections.
CONTRAINDICATIONS
Medically infirm patients with severe comorbidities may not be candidates for TKA because of a substantial risk of medical complications. Active knee sepsis, osteomyelitis, severe peripheral vascular disease, severe and profound neuropathy or neurologic disease (Parkinson’s disease, cerebrovascular accident), deficient extensor mechanism, and severely traumatized soft tissues may be contraindications to knee arthroplasty.
PREOPERATIVE PREPARATION
With this technique of knee replacement surgery, the soft tissue balancing is done early and progressively because bone preparation based on poorly balanced and improperly tensioned soft tissues can be flawed. This is different than the measured resection technique, in which the bone cuts are made independent of the soft tissues. After the trial components are inserted, the tissues are then balanced.
Evaluation
If the coronal alignment of the knee is “passively correctable” to neutral in 5 degrees of flexion, a smaller incision and no initial soft tissue release other than osteophyte removal should be necessary to balance the knee. If it is not, the surgeon should anticipate a longer incision and more extensive soft tissue balancing.
X-ray assessment may or may not show osteophyte formation. If there are substantial osteophytes on the concavity of the deformity, minimal dissection other than the osteophyte excision is necessary. If there is minimal correction passively and little arthrosis (such as in the mesomorphic middle-aged male), a soft tissue release is probably necessary (Figs. 7-1 and 7-2). Assess limb alignment and pattern of arthritis on preoperative x-rays to help determine roughly what may be needed in terms of osteophyte removal and ligament balancing. Regarding special situations, mild valgus knees may be passively correctable and need no early soft tissue release, whereas those with a developmental valgus and a hypoplastic lateral femoral condyle need soft tissue releases early to facilitate alignment. Laterally subluxated patellae in valgus knees—and even in some varus knees—require preoperative awareness such that femoral and tibial components can be lateralized or rotated to their maximal safe limit during the procedure and thus avoid patellar problems at the end of the case. Pure patellofemoral arthritis, without maltracking, often requires little soft tissue correction but may require strategies to avoid overstuffing the patellofemoral compartment, such as slight posterior displacement of the femoral component (which would cause a small notch in the anterior cortex) and overresecting the patella (which could result in fracture or avascular necrosis).
TECHNIQUE
Skin Incision
The patient is placed in the supine position, and a bump is placed to hold the knee at 90 degrees. The leg is marked, prepped, and draped. Typically, a midline incision is used. The length of the skin incision should be proportional to the difficulty of the case. A well-padded pneumatic tourniquet is applied and insufflated to 350 mm Hg following Esmarch exsanguination. The midline skin incision should be proportionate to the body habitus, with knee in flexion for obese patients. Create minimal skin flaps, yet enough to fully identify the quadriceps mechanism.
 FIGURE 7-1 Anteroposterior radiograph of the right knee in a 63-year-old man with severe osteoarthritis. |
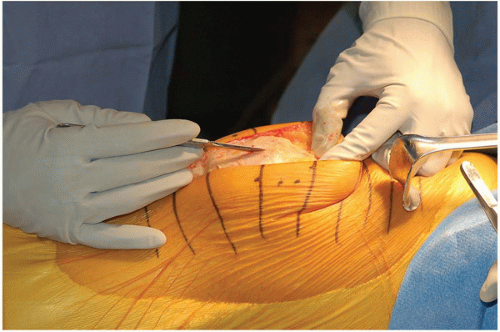
 FIGURE 7-3 Bilateral knees are marked for skin incisions with crosshatches. The tibial tubercle, patella, and quadriceps tendon are outlined. |
Surgical Approach
The initial arthrotomy should include the medial patellar capsule distally, extending subperiosteally down to the pes anserinus tendons. After osteophyte removal, subperiosteal dissection should extend posteriorly to but not through the semimembranosus tendons. Proximal to the patella, multiple arthrotomy options can be used, including a traditional quadriceps tendon incision (medial parapatellar), subvastus, midvastus (see Chapter 1). All osteophytes that are accessible (excluding those in the posterior part of the femur and tibia) should be excised early on to avoid oversizing the prosthetic components and to facilitate earlier soft tissue balancing.
An initial evaluation, perhaps with a central lamina spreader in extension, will help determine whether the soft tissue balance is approximately correct at this point, although it need not be precise. When releases are necessary, the surgeon needs to determine whether the tightness is in flexion or extension, or both. Static stabilizers such as ligaments may require release, whereas dynamic stabilizers such as tendons should generally be left to stretch after the arthroplasty. The primary issue is to avoid overreleasing in an attempt to gain full correction at this time, although approximate correction allows the soft tissues to contribute to the alignment of the parts. At this point, moving the knee between flexion and extension creates an opportunity for assessment regarding the need for future soft tissue releases.
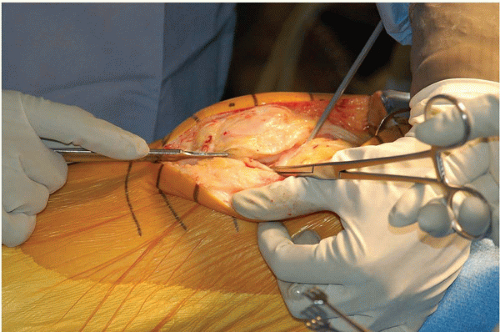
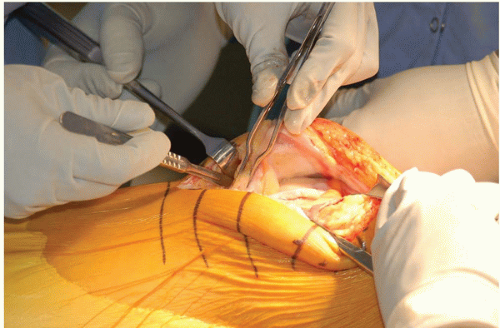
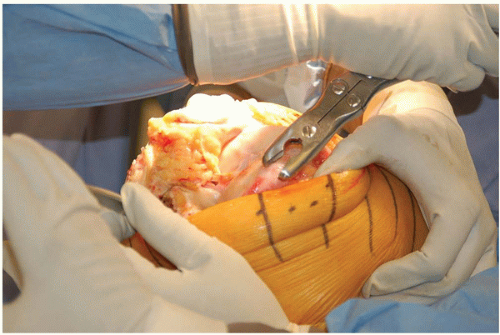
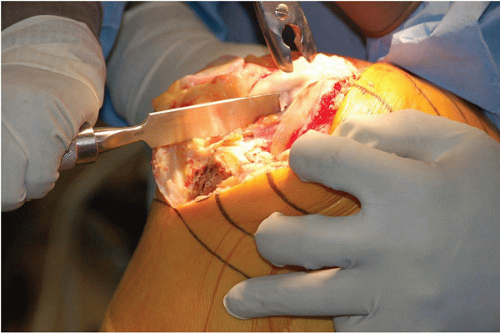
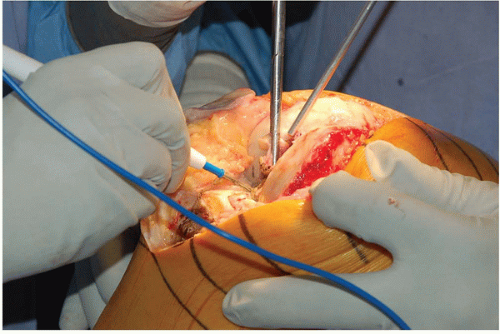
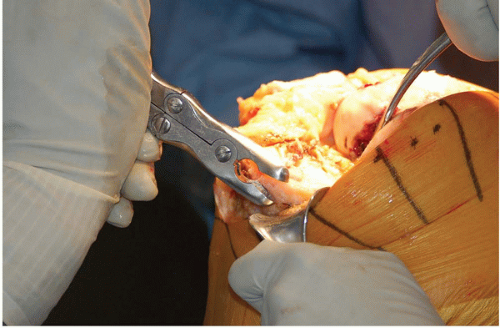
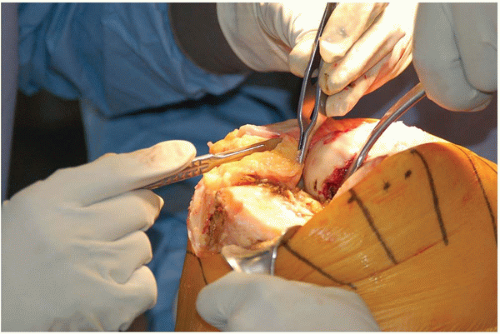
The surgical steps are as follows (Figs. 7-5, 7-6, 7-7, 7-8, 7-9, 7-10, 7-11, 7-12, 7-13, 7-14 and 7-15).
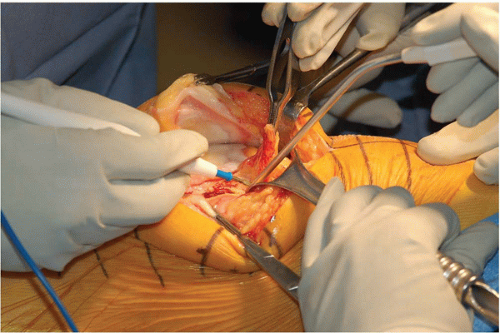 FIGURE 7-7 Minimal anterior femoral synovectomy defines the anterior femur, which is important in an anterior referencing system. |
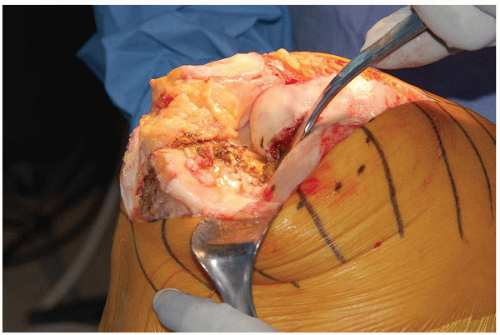 FIGURE 7-12 A Homan retractor is placed along the posterior border of the tibia forcing the tibia to sublux anteriorly. |
We prefer to perform a medial parapatellar arthrotomy, leaving a 2-mm tendon cuff to repair on the medial border of the patella. The surgeon must take care with fat pad excision to protect the patellar tendon.
An anterior femoral synovectomy is performed to identify the anterior margin of the femur. Medial soft tissue release is initiated with electrocautery or a scalpel and then continued with a Cobb elevator with the knee in a figure-four position.
The patient’s knee is flexed, the patella is everted, and the foot is placed on the bump.
Osteophytes from the anteromedial tibia and femur are excised, and overhanging femoral notch osteophytes are removed with a curved osteotome. Next, the anterior and posterior cruciate ligaments are removed with a Kocher and electrocautery.
The surgeon places a Homan retractor along the midline posterior border of the tibia, and the tibia is externally rotated and subluxed anteriorly. A Richardson retractor is placed along the medial soft tissue sleeve, and the medial meniscus is removed. Additional medial releases may be performed in a tight varus knee after the remaining medial tibial osteophytes are removed. Sequential release of the semimembranosus is typically all that is necessary, followed by subperiosteal slide of the superficial medial collateral ligament. Release of the pes anserinus tendons is almost never necessary. An additional fat pad may be removed to visualize lateral tibia, and a lateral Homan retractor is placed. The lateral meniscus excised, and the lateral inferior geniculate vessels are identified and cauterized.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree