Varus and Valgus Deformities
William J. Long
Giles R. Scuderi
INDICATIONS/CONTRAINDICATIONS
Fixed angular deformity about the knee necessitates special consideration to restore normal alignment during a total knee arthroplasty (TKA). With fixed angular deformity, one ligament is shortened or contracted while the opposite ligament is usually elongated. Particularly with varus deformity, there is often an associated flexion contracture with involvement of the posterior capsule. The cruciate ligaments, being in the center of the knee, usually retain their normal length; however, it may be difficult to elongate the contracted side without releasing the cruciate ligaments. The ideal postoperative alignment is independent of the original anatomy and should not be compared to that of the opposite, “normal knee,” because it most likely has a similar angular deformity. This ideal alignment, which is achieved by balancing the soft tissues and placing the prosthetic components in proper position, is 5 to 9 degrees of anatomic valgus. The tibial component should be placed at 90 degrees (perpendicular) to the mechanical axis of the tibia in the coronal plane, while the posterior slope in the sagittal plane is dictated by the implant design. The ideal placement of the femoral component is 5 to 7 degrees of valgus angulation in the coronal plane and 0 to 5 degrees of flexion in the sagittal plane (1). When the alignment is not sufficiently corrected, the components will be unequally loaded and subjected to excessive stress, resulting in eventual loosening of the prosthesis (2). Intraoperatively, it is imperative to reassess each step of the soft tissue release as it is performed so as not to overcorrect the deformity and create an unwanted instability. When using cruciate-retaining or posterior stabilized knee prostheses, the intact collateral ligaments and not the prosthesis alone give stability to the knee (3).
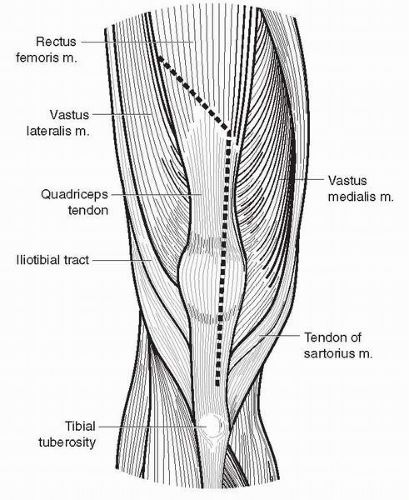
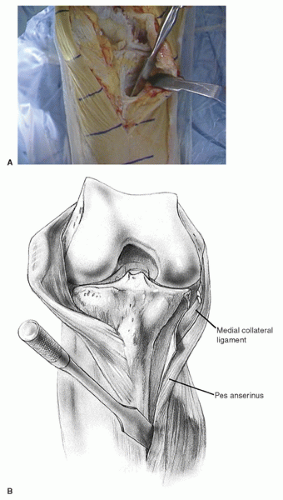
Varus deformity is usually caused by medial tibial bone loss with contracture of the medial collateral ligament, posterior medial capsule, pes anserinus, and semimembranosus muscle (Fig. 9-1). Medial femoral bone loss, which may be present, is usually minimal. Elongation of the lateral collateral ligament is a late event, and rupture of the ligament is rare.
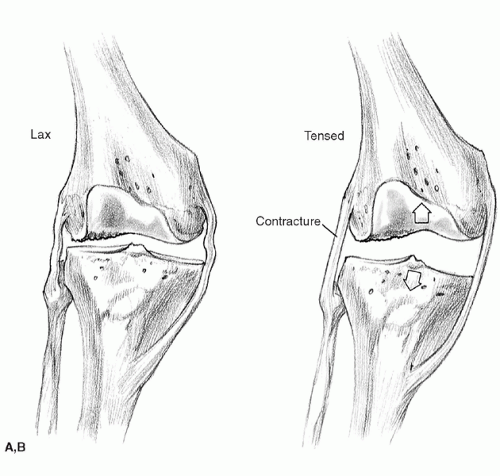
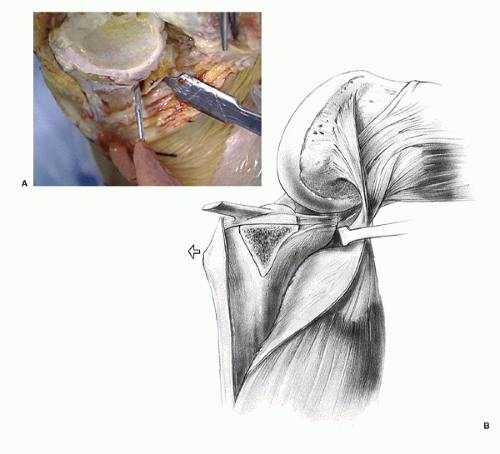
A fixed valgus deformity is caused by contracture of the iliotibial band and biceps femoris, lateral collateral ligament (LCL), popliteus, and posterolateral capsule (Fig. 9-2A,B). Elongation of the medial collateral ligament (MCL) is a late secondary event. Knees with rheumatoid arthritis and valgus deformity usually have an external rotation deformity of the tibia caused by contracture of the iliotibial band. Because of the articulation of the lateral femoral condyle with the posterior aspect of the tibia, valgus deformity usually includes a posterior lateral tibial defect with sparing of the anterior tibial margin. The lateral femoral condyle, which is often hypoplastic, is eroded in a valgus deformity because of its articulation with the tibia and wear from a laterally tracking patella.
PREOPERATIVE PLANNING
A careful physical examination should determine the degree of deformity, whether or not it is correctable, range of motion, muscle strength, and condition of the soft tissue envelope surrounding the knee. Ligamentous instability is rarely a problem in the degenerative knee with a fixed angular deformity. The anterior cruciate ligament is usually deficient or degenerative, particularly in younger patients with osteoarthritis, but this is not a problem in TKA (4). The integrity of the posterior cruciate ligament (PCL), however, will determine the choice of prosthesis. If the PCL is deficient or needs to be released or resected to correct the fixed deformity, then a PCL-substituting prosthesis should be implanted. For cases with severe contracture requiring extensive ligamentous release and difficulty in balancing the soft tissues, a constrained condylar prosthesis should be available.
Although limited weight-bearing knee views may provide sufficient templating ability for mild deformities (<15 degrees) (5), we continue to use a full-length standing anteroposterior radiograph, including the hip, knee, and ankle for more severe or complex deformities. The objective in correcting fixed angular deformities is to restore the mechanical axis of the leg to 0 degrees. This mechanical axis consists of a straight line from the center of the femoral head through the center of the knee and to the center of the ankle. Preoperative radiographs should also demonstrate any bony defects that may need augmentation, while the tangential (merchant) view allows for an assessment of patellar alignment and wear.
TECHNIQUE
Surgical Exposure
The anterior midline approach allows full exposure of the distal femur and proximal tibia (6). It is an extensile approach and can be extended proximally or distally as needed. This anterior incision also allows exposure of the medial and lateral supporting structures.
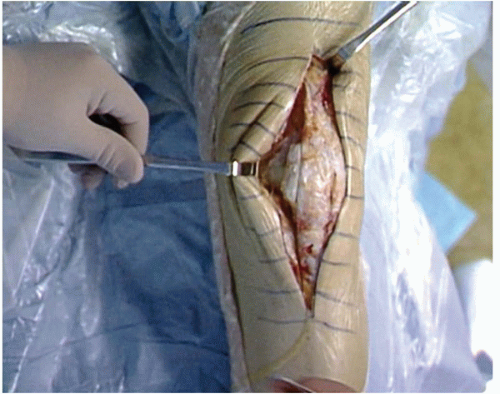
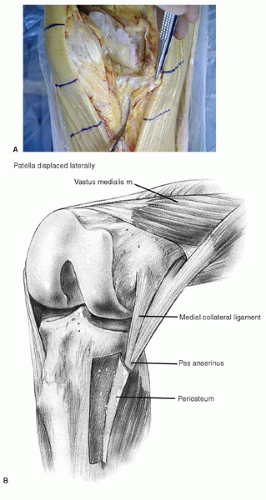
Following the skin incision, a limited medial parapatellar arthrotomy is performed through a straight incision extending over the medial one third of the patella and continuing along the medial border of the tibial tubercle (Fig. 9-3). The quadriceps expansion is peeled from the anterior surface of the patella by sharp dissection until the medial border of the patella is exposed (Fig. 9-4). The synovium is divided, and the fat pad is split in line with the capsular incision. The patella is then subluxed
laterally. To avoid avulsion of the patellar tendon, it can be subperiosteally dissected to the crest of the tibial tubercle, releasing tension while the knee is flexed (6). This approach is the most versatile, allows the broadest exposure to the knee joint, and can be extended proximally into a quadriceps snip, or distally with a tibial tubercle osteotomy.
laterally. To avoid avulsion of the patellar tendon, it can be subperiosteally dissected to the crest of the tibial tubercle, releasing tension while the knee is flexed (6). This approach is the most versatile, allows the broadest exposure to the knee joint, and can be extended proximally into a quadriceps snip, or distally with a tibial tubercle osteotomy.
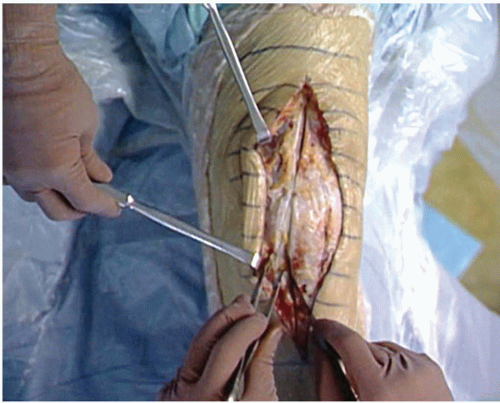 FIGURE 9-3 The medial parapatellar arthrotomy extends from the quadriceps tendon over the medial one third of the patella and continues along the medial border of the tibial tubercle. |
Varus Deformity
To correct a fixed varus deformity, progressive release of the tight medial structures is performed until they reach the length of the lateral supporting structures (7). With the knee in extension, soft tissues are dissected from the anteromedial tibia, as a continuous subperiosteal sleeve progressing medially (Fig. 9-5A,B). A periosteal elevator can be used to develop this plane approximately 3 to 4 cm distal to the medial joint line (Fig. 9-6). Retraction for better exposure during the release is performed with a sharp bent Homan retractor (Fig. 9-7). Placement of this retractor also allows traction on the medial soft tissues, facilitating the subperiosteal release around to the posteromedial corner distal to the joint line.
The cruciate ligaments may inhibit the correction and should be resected if they do (8). Attempts to retain the PCL in cases of severe varus deformity usually result in an inability to correct the deformity. Although conceptually it would be appealing to progressively release the PCL or perform a recession from the tibial spine, we prefer to resect it and insert a PCL-substituting prosthesis. In addition to preventing the correction of a fixed varus deformity, a tight PCL will limit motion and cause the knee to open like a book, preventing the more normal gliding and rolling motion that occurs with knee flexion (8).
The knee can now be flexed and the tibia externally rotated. The insertion of the semimembranosus muscle is released from the posterior medial corner (Fig. 9-8A,B), and the posterior and medial osteophytes are removed at this time. Excising osteophytes from the medial femur and tibia facilitates the release as they tent the medial capsule and ligamentous structures, and their removal can produce a minimal amount of correction by relaxing tension on the superficial MCL, before the soft tissue release is begun. Further trimming of posteromedial osteophytes may need to be performed after the proximal tibia is resected and the trial tibia is applied.
At this point, and following each further step in the release, gap and alignment balance can be assessed by removing retractors and applying a valgus movement across the knee in extension or inserting lamina spreaders within the medial and lateral joint space and judging alignment with respect to the mechanical axis.
A medial release is performed with the knee in extension and a Homan retractor in place. A ¾-inch osteotome is used to progressively release medial soft tissues including the superficial MCL and pes insertion from proximal to distal along the tibia. Palpation of tight structures facilitates a focused release. Complete release extends up to 15 cm distal to the medial joint line.
In marked fixed varus deformities, the medial subperiosteal dissection is continued posteriorly and distally, including the deep fascia of the soleus, while maintaining continuity of the medial soft tissue sleeve (Fig. 9-9A,B). When a flexion contracture is present, it may be necessary to resect posterior tibial osteophytes and further release the posterior capsule, which can be stripped subperiosteally from the femur and/or the tibia, after the bone cuts are made. In severe cases with extensive subperiosteal dissection, the proximal medial tibia appears skeletonized (Fig. 9-10).
 FIGURE 9-6 The subperiosteal sleeve is continued posteriorly, using a periosteal elevator for further release. |
When the medial release is complete and normal alignment has been achieved, the standard bone cuts are made (9). The level of the tibial cut is constant, conservative, and perpendicular to the long axis of the tibia. In a knee with a varus deformity, more bone is resected from the lateral than from the medial tibial plateau. Once the tibia is cut, resection of the femur is undertaken. The flexion gap produced should be rectangular rather than trapezoidal in shape (Fig. 9-11A,B), and to achieve this, the femoral component is rotationally set along the epicondylar axis. This results
in more bone resection from the posterior medial femoral condyle than from the posterolateral femoral condyle.
in more bone resection from the posterior medial femoral condyle than from the posterolateral femoral condyle.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree