Impaction Bone Grafting for Large Bone Defects
Paul A. Lotke
Jess H. Lonner
INDICATIONS
Large bone defects are frequently encountered during revision surgery for total knee arthroplasty. These are usually caused by osteolysis secondary to polyethylene wear or particulate debris. Large bone defects are also noted after removal of a prior prosthesis, however, especially if large femoral and tibial stems were present or after staged procedures for sepsis. The defects are frequently irregular in contour. This irregularity makes it difficult to use preformed spacers or augments without sacrificing additional bone (1). The impacted bone-grafting technique offers the ability to fill the irregular defects, as well as the opportunity to reconstitute bone. It has had long-term success in total hip arthroplasty and more recently for revision total knee surgery.
The combination of a long stem, cemented and imbedded within impacted bone graft creates a rigid, structurally sound support for large defects in the femoral or tibial metaphyses. Uncontained defects, in either of these metaphyseal areas, can be enclosed with wire mesh (2). Therefore, impacted bone grafting is clinically versatile and can be used in a wide variety of clinical situations.
CONTRAINDICATIONS
There are few absolute contraindications for use of impacted bone graft other than the presence of sepsis. It is time consuming, especially with uncontained defects requiring wire mesh enclosure. However, the ability to reconstruct bone and fill irregular defects can balance the time expended in using this technique.
ALTERNATIVES
Alternative methods of biological reconstruction include bulk allografts, however, they are technically difficult to fit and never incorporated into the host. Non-biologic materials, such as metallic augments and metaphyseal cones are also available, especially with the porous ingrowth metals. The ability to ultimately reconstruct bone makes impaction grafting a particularly advantageous alternative, however, especially in younger patients.
The alternative treatments include re-enforcing cement, metallic augments, metaphyseal porous metal cones, and structural allografts.
PREOPERATIVE PREPARATION
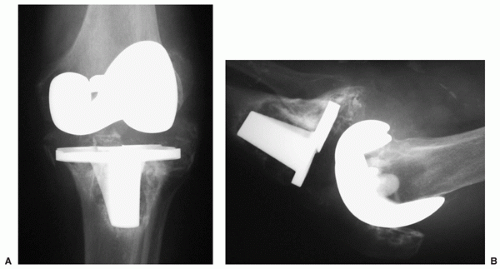
Standard anterior, posterior, lateral, and patellar radiographs should be used to evaluate all painful total knee arthroplasties (Fig. 21-1A,B). It is well recognized, however, that the standard
radiographs routinely underestimate the extent of osteolysis that occurs in metaphyseal bone and behind the prostheses. Special sequence magnetic resonance imaging scans and computed tomography can be helpful for determining bone defects but depend on the imaging techniques and can be misleading as well. As with all preoperative preparations for revision total knee surgery, care should be taken to rule out the possibility of infection. If infection is suspected, multiple aspirations of the knee should be done, sedimentation rate and C-reactive protein laboratory studies obtained before surgery, and frozen pathology sections should be requested at the time of surgery.
radiographs routinely underestimate the extent of osteolysis that occurs in metaphyseal bone and behind the prostheses. Special sequence magnetic resonance imaging scans and computed tomography can be helpful for determining bone defects but depend on the imaging techniques and can be misleading as well. As with all preoperative preparations for revision total knee surgery, care should be taken to rule out the possibility of infection. If infection is suspected, multiple aspirations of the knee should be done, sedimentation rate and C-reactive protein laboratory studies obtained before surgery, and frozen pathology sections should be requested at the time of surgery.
SURGICAL TECHNIQUE
The patient is positioned, prepped, and draped in the usual manner. A cross-table foot post may be used to help stabilize the knee in the fully flexed position.
The exposure should generally utilize the prior skin incision and excise the widened stretched scar. Given the complexity of many revision total knee arthroplasties, in the presence of massive bone loss, a medial parapatellar arthrotomy is extensile and recommended. When extending the incision proximally, care should be taken to remain within the quadriceps tendon, so that a quadriceps snip across the tendon to obtain better exposure can be readily repaired. Care should be taken to avoid crossing the quadriceps tendon too distally or entering into the medialis muscle, as it makes repairing the quadriceps snip more problematic. Care should also be taken to protect the patella tendon attachment from peeling off the tibial tubercle. The patella should be subluxed, and rarely if ever, everted. In many of the knees with massive osteolysis, the tibial tubercle bone or the bones under the femoral condyles may be so thin that fracture is possible. Special care should be taken to avoid losing the integrity of these structures.
After reasonable exposure has been carefully obtained, we recommend a complete synovectomy to obtain full exposure and relaxation of the remaining soft tissue sleeve. As noted in Figures 21-2, 21-3 and 21-4, the synovium can be removed sharply with its surrounding capsule. First, we remove the synovium from the suprapatellar pouch and then the medial and lateral extensions. When the synovium has been removed, it relaxes the medial and lateral soft tissue sleeves, making the knee more mobile and exposes the prosthetic interfaces. The remainder of the posterior synovium can be resected after the prosthesis has been removed.
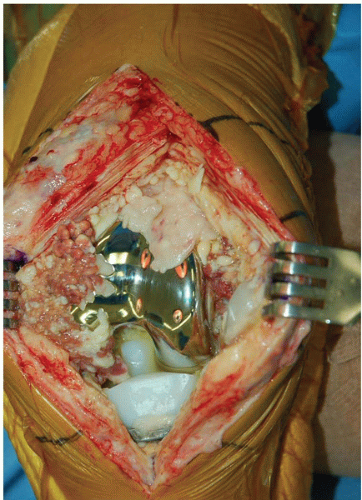 FIGURE 21-2 Exposure of the knee demonstrating marked synovial proliferation surrounding the prosthetic component and obscuring vision. |
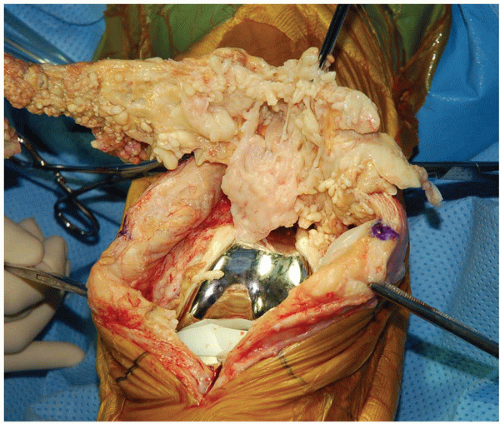 FIGURE 21-3 Removal of synovium by sharp dissection. The combined synovium and capsule are first removed from the suprapatellar pouch and medial-lateral extensions. |
The prosthesis can be removed by standard techniques depending on its fixation, remaining bone stock, and style of prosthesis. Flexible osteotomes, thin saw blades, and osteotomes are standard requirements for removing the prothesis with the least amount of additional bone loss. It is best to remember not to insert a primary prosthesis that cannot be readily removed. Porous stems, notches imbedded within cement mantles, and rough textured surfaces make it extremely difficult to remove prostheses from the femur and tibia and should be avoided if possible.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree