CHAPTER 58 Minimally Invasive Posterior Lumbar Fusion Techniques
Despite these advances, the morbidity of spinal fusion surgery remains significant. The standard posterior midline exposure is notorious for paraspinal muscle stripping and denervation leading to significant postoperative scar formation. The limitations of this approach for spinal fusion have been well documented, especially regarding a prolonged recovery period and muscle damage that may affect a patient following surgery.1–5
In recent years, less invasive surgical approaches have been developed to minimize damage to the paraspinal soft tissues during surgical exposure. These “minimally invasive” surgical approaches are becoming more popular because they offer the surgeon a method to achieve the goals of spinal surgery while minimizing some of the perioperative morbidity inherent to the classic posterior approach.6,7
Principles of Minimally Invasive Spinal Surgery
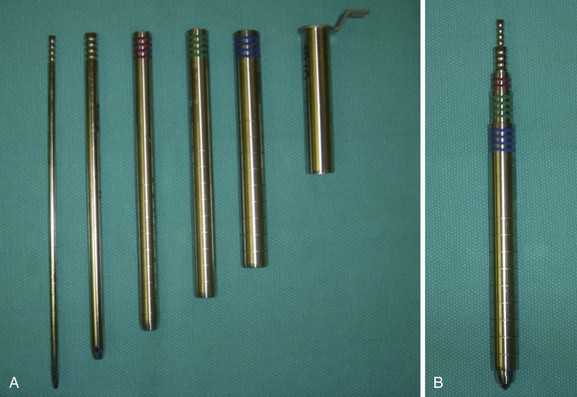
All minimally invasive spinal procedures, despite the type and the location, have the common goal of correcting the underlying spinal pathology while avoiding excessive damage to the paraspinal soft tissue envelope. As with other spine procedures, an MISS procedure begins with the careful analysis of the preoperative imaging studies to precisely localize the spinal pathology. Before making a surgical incision, preoperative fluoroscopy is used to localize the involved spinal segments and plan the skin incision. During the surgical approach, the paraspinal muscles are split rather than cut or resected using serial tubular dilators to create a surgical corridor between the skin incision and the spine (Fig. 58–1). Only necessary portions of the vertebral columns are exposed, and excessive use of electrocautery or vigorous retractor pressures should be avoided.
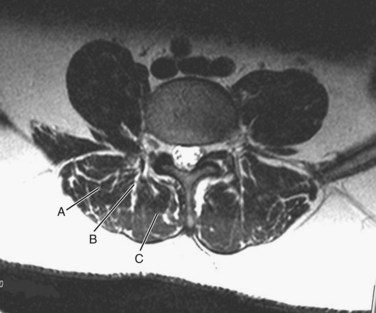
The surgeon must understand the muscular anatomy of the paraspinal region to design the optimal approach for an MISS procedure. There are two distinct muscular compartments: the multifidus compartment, which overlies the midline spinal structures, and the lateral compartment, which overlies the transverse processes (Fig. 58–2). The multifidus muscle surrounds the spinous processes, lamina, and facet joints. The multifidus muscles receive its nerve and blood supply from the medial branches of the dorsal rami and segmental vessels, respectively, which course from the intervertebral foramen along the base of the transverse process and enter the lateral margin of the muscle in the region of the pars intra-articularis. Care should be taken to avoid rupturing the lateral attachments of the multifidus muscle, which would disrupt the nerve and blood supply to the multifidus muscle, leading to atrophy and scar formation in the substance of the muscle. The lateral muscle compartment contains the longitudinally oriented muscles of the erector spinae group. The lateral compartment overlies the transverse processes and includes the entry site for pedicle screw insertion at the base of the transverse process. The lateral compartment is traversed whenever a posterolateral onlay fusion is performed.
Surgical Setup for a Posterior Fusion Procedure
Setup and Imaging
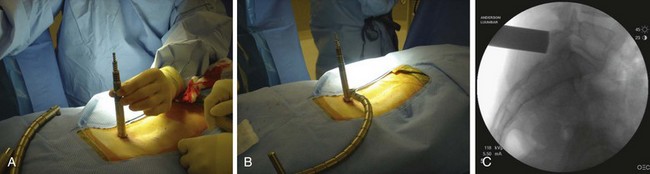
Following placement of surgical monitoring equipment and the induction of general anesthesia, the patient should be positioned prone on a radiolucent spinal frame (Fig. 58–3). The abdomen should be free of compression, and free access to the lumbar region for fluoroscopy should be confirmed. The preoperative imaging studies should be available in the room with the operative plan clearly marked. The surgeon should ensure the availability of the proper implants and instruments prior to commencing with the operative procedure.
Surgical Incisions and Approach
When operating through a tubular retractor, the smallest dilator is then docked at the appropriate bony site and serial dilation is used to expand the operative corridor. Care should be taken into bringing each subsequent dilator in contact with the bony elements. The correct length of the tubular retractor can then be selected, inserted, and secured using an operating table–mounted retractor holder. Once the tubular retractor is in place, the position of the retractor should be verified using fluoroscopy (Fig. 58–4).
Posterior Interbody and Transforaminal Interbody Fusion
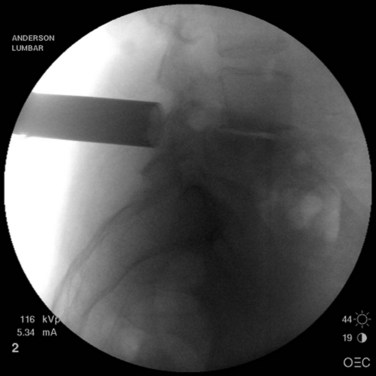
When performing a posterior or transforaminal lumbar interbody fusion (PLIF and TLIF) via a minimally invasive approach, it is important to align the tubular retractor collinear with the disc space on the lateral view (Fig. 58–5). When performing a TLIF procedure, the tubular retractor must be aligned with enough lateral to medial angulation to allow the surgeon to reach the contralateral side of the disc space for preparation of an adequate fusion bed (Fig. 58–6). During the exposure, adequate facet joint must be removed to minimize retraction of the neural elements and provide working access to the disc space.8
The detrimental effects of over-retraction of the neural elements with the PLIF procedure have been well documented in the literature.9 Facet removals for a PLIF or TLIF can be achieved with either osteotomes or a high-speed burr. It is helpful to skeletonize the upper and medial portions of the caudal pedicle (e.g., L5 pedicle for a L4-5 TLIF) to gain adequate access to the disc space and allow safe retraction/protection of the dural/neural elements.
After disc space preparation, the interspace should be packed with autogenous bone graft or an adequate fusion substrate. An interbody fusion cage, of appropriate size, is selected and packed with the graft material, before impacting the cage into the disc space. The optimal position of the cage is toward the anterior portion of the disc space.10,11 This produces better reconstruction of the sagittal contour of the spine and allows ample bone graft material to be packed around and behind the cage.
Posterolateral Fusion (Intertransverse Onlay Fusion)
From the traditional midline approach, access to the intertransverse region for onlay fusion requires complete stripping of the paraspinal muscles to the tips of the transverse processes, an act that causes destruction, or at least disruption, of the multifidus muscle and significant postoperative scarring.5 Using the paraspinal muscle-splitting approach (Wiltse approach), exposure of the intertransverse region is simple to achieve without major muscle stripping. This provides direct access to the intertransverse region for fusion.
The skin incision for a paraspinal approach for intertransverse fusion is made at least 3.5 to 4 cm lateral to the midline. The fascia is divided in line with the skin incision, and the paraspinal muscles are split in line with their fibers to expose the transverse processes. For fusion purposes, the entire transverse process at both levels should be exposed. Either a tubular retractor (preferably an expandable tubular retractor) or side-to-side (e.g., McCullough retractor) retractor can be used to visualize the intertransverse interval. The authors prefer to use an expandable tubular retractor, which allows both transverse processes to be simultaneously exposed (Fig. 58–7).

FIGURE 58–7 The use of an expandable tubular retractor allows simultaneous exposure of both transverse processes.
Facet Fusion
To perform a facet fusion, the retractor should be docked on the facet, which resides in the lateral portion of the multifidus compartment (see Fig. 58–2). If decompression of the spinal canal is required, facet fusion can easily be performed during the exposure through the multifidus compartment. Once the facet is exposed, the capsule is removed with electrocautery and the articular surfaces of the inferior and superior articular processes are identified. A high-speed burr is used to decorticate the facet joint along its entire length, and the joint space is packed with fragments of autogenous bone or a suitable bone substitute.