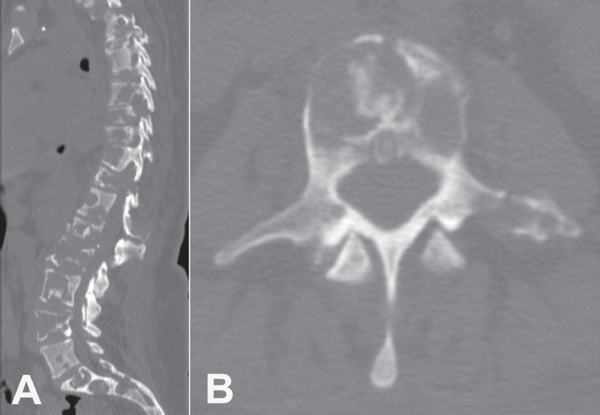
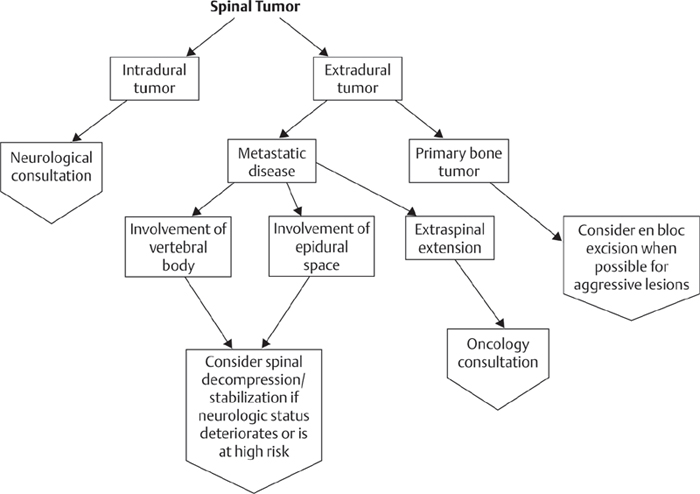
47 The spine is the most common site of skeletal metastatic disease. Spinal metastases account for the majority of spinal tumors encountered by spine surgeons. Breast carcinoma is the most common primary in women (Fig. 47.1A,B), while lung and prostate carcinoma are the most common primary sources in men. Renal, thyroid, and gastrointestinal tumors are also commonly seen, but in lesser frequency then the former mentioned tumors. Breast, prostate, and renal metastases are more likely to be seen by spine surgeons because of the longer relative survival compared with lung and gastrointestinal carcinoma. The most common first symptom of spinal metastasis is mechanical pain, often well localized, insidious in onset, positional, and severe enough to disturb sleep. Patients may also present with various neurologic symptoms ranging from mild sensory or motor radiculopathy to complete paralysis due to neurologic compression, either directly from excessive tumor load or through instability of a pathologic fracture. Spinal metastasis may be the presenting complaint in a patient previously unaware of having a malignancy. The history should also address constitutional symptoms, such as fever, chills, malaise, and weight loss, as well as malignancy in the patient history and family history. Radiographic evaluation begins with plain films looking for tumor location, bony destruction, soft-tissue extension, and pathologic fracture. Classic radiographic signs such as the “winking owl” (missing pedicle) or vertebra plana are present only after significant bony destruction. Magnetic resonance imaging (MRI) allows excellent evaluation of the neurologic elements and soft-tissue tumor involvement. Key tumor characteristics, such as density and vascularity, are also readily seen on MRI. Computerized tomography (CT) scans are helpful in evaluating bony lesions, determining stability, and preoperative planning. Pathologic diagnosis should be obtained by biopsy, either CT-guided or open. Bone scans may be used as screening tools to identify other sites of metastasis, both in the spine and in the apical skeleton. Areas of metastasis identified outside of the spine, especially if they occur around the hips, should be imaged to evaluate for potential impending pathologic fracture. Fig. 47.1 CT of metastatic breast carcinoma of the vertebral column. (A) Sagittal. (B) Axial. For patients who present with metastatic lesions in the spine and who have not previously been diagnosed with cancer, a thorough examination should be performed. This often includes blood work, including complete blood count (CBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), ionized calcium level, and serum and urine electrophoresis (SPEP and UPEP). Prostate-specific antigen (PSA) levels should be checked in men. CT scans of the chest, abdomen and pelvis should be obtained. Biopsy of either the spinal lesion or another lesion identified on imaging studies is necessary to make a definitive diagnosis. Goals of any intervention are improved quality of life via palliation of pain and prevention of neurologic worsening. The patient’s overall health and prognosis must be taken into account when considering surgery or radiation, and close consultation with the medical oncologist, patient, and family should be the first step. Surgery should not be considered in patients who are hopelessly bedridden with an expected survival of less than six weeks. Vertebroplasty or kyphoplasty is useful for palliative treatment of select tumors wholly contained within a vertebral body. Indications for use are refractory pain without neurologic deficit. The posterior vertebral body wall must be intact to prevent extravasation of cement into the spinal canal. Radiation therapy may be extremely useful for pain and tumor control in select pathologies, particularly germ cell and hematopoietic lines. Close coordination with the radiation oncologist is mandatory, as protocols change often, and variability in the direction of external beam may avoid irradiating a potential surgical approach. Indications for surgical management include an isolated spinal lesion, pathologic fracture or deformity causing a neurologic deficit, or refractory pain and radioresistant tumors. The mainstay of treatment is intralesional excision and spinal reconstruction. Strong consideration should be given to “overfixing” with instrumentation, as immediate unbraced activity is necessary to maintain constitutional fitness, and solid osseous union may never be achieved in the face of an immunocompromised cancer patient. Anterior, posterior, and combined approaches all have a place in reconstructive efforts, largely depending on level, degree of instability, and surgeon preference. Multiple noncontiguous lesions may create a very difficult situation. Patchels et al. in 2005 presented the only level I evidence comparing radiation to surgery. Exquisitely radiosensitive tumors were not studied and should be treated with radiation. Patients randomized to surgery had statistically better return of neurologic function, preservation of bowel and bladder function, relief of lower pain, and improved ambulation. Those who crossed over from radiation to surgery did not improve as much as those who were randomized to surgery, and the complication rate was higher. The study was stopped early by the review board because the results so heavily favored surgery over radiation. Though these results strongly favor surgical treatment of carcinoma and adenocarcinomas, a thorough discussion of the risks and benefits of all options must be undertaken. Outcomes and prognosis for spinal metastasis vary based on several interrelated factors: primary tumor site, general health of the patient, number of extraspinal metastases, number of spinal metastases, metastatic involvement of internal organs, and severity of neurologic deficit on presentation. Wound healing in cancer patients is often challenging. If radiotherapy is used as an adjunct to definite surgical stabilization, serious consideration should be given to deferring radiotherapy until after surgery to minimize complications of operating in an irradiated bed. Discussing the approach and incision with the radiation oncologist may help avoid unnecessary radiation to the incision. Patients with diffuse metastatic disease may be systemically ill, cachectic, and malnourished. Aggressive nutritional support should be considered mandatory preoperatively as well as postoperatively and can help avoid or limit wound healing problems. Abe E, Kobayashi T, Murai H, Suzuki T, Chiba M, Okuyama K. Total spondylectomy for primary malignant, aggressive benign, and solitary metastatic bone tumors of the thoracolumbar spine. J Spinal Disord 2001;14(3):237–246 PubMed Total spondylectomy was used to treat 14 patients with malignant or aggressive benign vertebral tumors. All patients had good pain relief and there were no serious complications. There were three local recurrences at 3.2 years. Dudeney S, Lieberman IH, Reinhardt MK, Hussein M. Kyphoplasty in the treatment of osteolytic vertebral compression fractures as a result of multiple myeloma. J Clin Oncol 2002;20(9): 2382–2387 PubMed This article reports prospective evaluation of 55 kyphoplasties in 18 patients. Mean follow-up was 7.4 months. SF36 scores for bodily pain, physical function, vitality, and social function all significantly improved. Fourney DR, Schomer DF, Nader R, et al. Percutaneous vertebroplasty and kyphoplasty for painful vertebral body fractures in cancer patients. J Neurosurg 2003;98(1, Suppl):21–30 PubMed Sixty-five vertebroplasties and 32 kyphoplasties were done in 56 patients with myeloma and primary malignant tumors. Median follow-up was 4.5 months with 84% complete pain relief. Patchell RA, Tibbs PA, Regine WF, et al. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet 2005; 366(9486):643–648 PubMed This landmark randomized controlled trial compared surgery to radiotherapy for metastatic lesions to the spine; it was ended early because significant benefits were seen for surgical patients. Ryu S, Fang Yin F, Rock J, et al. Image-guided and intensity-modulated radiosurgery for patients with spinal metastasis. Cancer 2003;97(8):2013–2018 PubMed In this evaluation of 10 patients, most had significant pain relief within 2 to 4 weeks after treatment. Sundaresan N, Rothman A, Manhart K, Kelliher K. Surgery for solitary metastases of the spine: rationale and results of treatment. Spine 2002;27(16):1802–1806 PubMed This is a retrospective review of 80 patients with solitary spinal metastasis from solid tumors. Median survival after surgery was 30 months. Surgical excision is recommended before radiotherapy to increase the chances of palliation and cure. Wai EK, Finkelstein JA, Tangente RP, et al. Quality of life in surgical treatment of metastatic spine disease. Spine 2003;28(5):508–512 PubMed In this prospective evaluation of 25 patients undergoing surgery for spinal metastasis, the greatest improvement was with pain; however, improvements in constitutional symptoms were also seen. Whyne CM, Hu SS, Lotz JC. Burst fracture in the metastatically involved spine: development, validation, and parametric analysis of a three-dimensional poroelastic finite-element model. Spine 2003;28(7):652–660 PubMed A finite-element study was undertaken to investigate features that contribute to burst fracture risk. The primary factors affecting fracture initiation were tumor size, magnitude of spinal loading, and bone density.
Metastatic Spinal Tumors
![]() Workup
Workup
![]() Treatment
Treatment
![]() Outcome
Outcome
![]() Complications
Complications
Suggested Readings
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






