19 Meniscus Repair: Outside-In Technique
Patient Presentation and Symptoms
Patients with meniscus tears frequently present with pain and mechanical symptoms such as “clicking” or “popping.” There may be a history of joint swelling. The pain typically is located at the joint line and worsens with activity. Occasionally, the knee is “locked” and range of motion is limited. The most common differential diagnosis is patellofemoral pain.
Indications
- Morphology: vertical longitudinal tears
- Location: red—red zone or red—white zone
- Patient compliance: ability to comply with postoperative protection and rehabilitation
- Associated injuries: better results with concurrent anterior cruciate ligament reconstruction
- This technique may also be used for meniscal allograft placement.
Contraindications
- Unstable knee in which future stabilization is not planned, since reinjury is likely
- Degenerative tears that prevent adequate coaptation of tear edges
- Partial-thickness tears
Physical Examination
- May be unable to bear full weight on the extremity
- Knee effusion is common.
- Joint line tenderness
- Range of motion may be restricted.
- Positive Steinmann test
- Check knee stability.
- Examine the hip to rule out referred pain.
Diagnostic Tests
- Radiographs are normal with an isolated meniscal tear but are usually obtained prior to surgery to evaluate for osteochondral lesions, joint space narrowing, and patellofemoral abnormalities. Stress fractures and capsular avulsion fractures can also be detected occasionally with plain radiographs.
- Magnetic resonance imaging (MRI) is 64 to 95% accurate for diagnosing a meniscal tear.1 It is not reliable for predicting reparability.2 Because false-positive readings for meniscus tears are not uncommon, the MRI interpretation is done in conjunction with the clinical findings.
Special Considerations
Most meniscus tears are best repaired through an “allinside” technique using bioabsorbable devices, but tears in the anterior third of the meniscus are more easily managed with the outside-in technique due to the difficulty in placing bioabsorbable devices across anterior tears through standard portals. The inside-out technique is still the gold standard for meniscus repair, but due to longer operative times and a larger incision this technique has become less popular compared with all-inside and outside-in techniques.
The current consensus is that the age of the tear and the age of the patient are very minor factors affecting meniscus repair healing.3 Certainly, for tears that have borderline indication for repair, the age of the patient becomes a larger factor in the decision.
Preoperative Planning and Timing of Surgery
The surgery should be performed as soon as convenient for the patient and surgeon. A long time period between injury and repair may contribute to tear propagation or chondromalacia.
Special Instruments
- No. 0 PDS suture: rigid enough for passing through spinal needles
- Meniscus Mender II (Instrument Makar, Inc.): This disposable kit contains an assortment of straight and curved spinal needles and suture retrievers to facilitate the procedure.
- Alternatively, regular 18-gauge spinal needles and arthroscopic graspers may be used.
Anesthesia
General or regional anesthesia is recommended to allow for tourniquet use and joint distraction. Local anesthesia is an alternative.
Patient and Equipment Positions
The patient may be positioned supine in an arthroscopic leg holder or with the extremity draped free, with or without a lateral post attached to the table.
Surgical Procedure4
- Place the arthroscope in the ipsilateral portal.
- Flex the patient’s knee 10 degrees for medial tears, 90 degrees for lateral tears.
- Rasp or shave the tear edges.
- Hold the tear reduced with a probe.
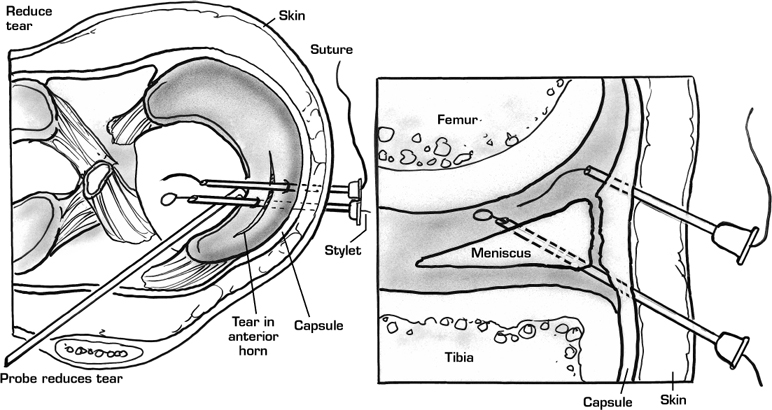
- Under arthroscopic guidance, place an 18-gauge spinal needle percutaneously until it crosses the tear site. Transillumination may assist in locating neurovascular structures (Fig. 19–1).
- Make a small skin incision around the needle and spread down to the capsule.
- Pass a second needle through the same incision until it emerges through the meniscus on the opposite side of the tear from the first needle (Fig. 19–2).
- With the Meniscus Mender II kit, place a wire-loop suture retriever through one needle and 0 PDS suture through the other needle (Fig. 19–3).
- Use an arthroscopic grasper to guide the intraarticular portion of the suture through the wire loop.
- Using the wire loop, pull the suture out through the needle.
- Tie extraarticular knot directly against capsule without entrapping cutaneous nerves.
- Place sutures 4 mm apart until the tear is stable to probing.
Alternative Technique5
- Place the arthroscope in the ipsilateral portal.
- Flex the patient’s knee 10 degrees for medial tears, 90 degrees for lateral tears.
- Rasp or shave the tear edges.
- Hold the tear reduced with a probe.
- Under arthroscopic guidance, place an 18-gauge spinal needle percutaneously until it crosses the tear site. Transillumination may assist in locating neurovascular structures.
- Make a small skin incision around the needle and spread down to the capsule.
- Pass a second needle through the same incision until it emerges through the meniscus on the opposite side of the tear from the first needle.
- Pass a 0 PDS suture through one spinal needle. Retrieve it with an arthroscopic grasper and pull it out through the contralateral portal. Remove the spinal needle and clamp each end of suture outside the knee.
- Pass a second 0 PDS suture through the second spinal needle. Retrieve it with an arthroscopic grasper and pull it out through the contralateral portal. Remove the spinal needle and clamp each end of suture outside the knee.
- Tie a large knot with multiple throws (Mulberry knot) in the two ends of suture on the femoral side of the meniscus.
- Pull the opposite ends of the sutures until the knots reduce and hold the meniscus.
- Tie extraarticular knot directly against capsule without entrapping cutaneous nerves.
- Place sutures 4 mm apart until the tear is stable to probing.
Dressings, Braces, Splints, and Casts
Use a standard knee arthroscopy dressing such as gauze, light cotton padding, and Ace bandage. Braces are usually not necessary. Splints and casts are generally discouraged because their use may lead to knee arthrofibrosis.
Tips and Pearls
It is important to hold the meniscus reduced during passage of the spinal needles, so that the reduction will be easy to maintain when the sutures are tensioned. Placing both spinal needles prior to passing any sutures aids in guiding the second needle and also prevents cutting the first suture with the second needle.
Pitfalls and Complications
The unique concern with the outside-in technique is entrapment of cutaneous nerves, which can lead to postoperative paresthesia. For posterior meniscus tears, needle entry must be posterior, further increasing the risk of neurovascular injury. Injury can be avoided by using curved spinal needles or by, alternatively, using the allinside or inside-out techniques.
Postoperative Care
If ACL reconstruction has been performed simultaneously with meniscus repair, the rehabilitation is focused toward the ACL reconstruction. For isolated meniscus repairs range of motion is immediately encouraged from 0 to 90 exercises are initiated 8 weeks postoperatively. Sport-degrees of flexion. No brace is prescribed. Weight bearing specific training begins at 3 months. The patient is is allowed to tolerance with crutches as needed. Patellar allowed to return to full activity including pivoting sports mobilization, icing, and isometric quadriceps strengthen- after 4 months when the quadriceps and hamstring ing are begun right away. Resistance strengthening strength are at least 90% of the contralateral side.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








