4
Meniscus Allograft Transplantation
There has been an emerging emphasis on meniscal preservation following meniscal injuries primarily due to an increasing understanding of the importance of meniscal function for load sharing, joint stability, and articular cartilage protection. Several studies have demonstrated poor long-term outcomes following even partial meniscectomy, with an increased incidence of osteoarthritis. Because meniscal preservation is not always possible, there remains an existing population of patients who have undergone subtotal or total meniscectomy. A subset of these patients will become symptomatic due to progressive degenerative change in the affected hemijoint, and meniscal allograft transplantation is an option to replace the native meniscus in these select individuals. With rigid adherence to surgical indications and technique, excellent pain relief and improved function can be achieved.
The technique for both medial and lateral meniscal transplantation is described. The preferred technique for medial meniscal transplantation is the use of free bone plugs at the horn attachments. The preferred technique for lateral meniscal transplantation is a slot technique. A “keyhole” technique can also be used for lateral meniscus transplantation. Because more normal tibiofemoral biomechanics is achieved with soft tissue fixation to bone, both techniques emphasize retention of bony attachments as opposed to relying on soft tissue fixation alone.
Indications
Meniscal allograft transplantation is indicated in patients with a history of one or more previous meniscectomies with complaints of persistent pain in the involved compartment. Typically, there is good resolution of pain following the initial meniscectomy, but over time, there is an increase in ipsilateral joint line pain, activity-related swelling, and generalized aching of the knee. Degenerative changes should ideally be less than grade 3, and axial malalignment and ligament insufficiency must be normalized prior to or simultaneously with allograft meniscus transplantation.
Contraindications
Meniscal allograft transplantation is contraindicated in the presence of significant articular cartilage damage (i.e., late grade 3 or 4 chondral disease) in the ipsilateral compartment. In cases of localized chondral defects, however, simultaneous cartilage restoration can be performed. Ligament insufficiency and malalignment are not strict contraindications, but they must be addressed simultaneously or in a staged fashion prior to meniscus transplantation.
Diagnostic Testss
To rule out significant osteoarthritis that would contraindicate the procedure, standard weight-bearing anteroposterior (AP) radiograph of both knees in full extension, a non-weight-bearing 45-degree flexion lateral view, and an axial view of the patellofemoral joint should be obtained. Additionally, a 45-degree flexion weight-bearing posteroanterior (PA) radiograph is recommended to help identify subtle joint space narrowing that traditional extension views may fail to identify. Special studies such as a long-cassette mechanical axis view or magnetic resonance imaging (MRI) should be ordered with any degree of clinical malalignment or suspicion for chondral injury, respectively. In cases where questions remain as to the source of a patient’s symptoms, a three-phase technetium bone scan is potentially useful. Both MRI and bone scan may demonstrate increased signals in the affected compartment related to stress overload there due to the meniscal deficiency.
Differential Diagnoses and Other Options
Patients with significant articular cartilage disease or osteoarthritis can have similar complaints as those with meniscal deficiency. In patients with ligamentous deficiency or malalignment, procedures to restore ligament stability, such as anterior cruciate ligament (ACL) reconstruction, or correct alignment, such as high tibial osteotomy, may provide significant pain relief alone, alleviating the need for meniscal transplantation. This may be especially true in older or lower-demand patients. Thus, staging these procedures is a reasonable algorithm in select individuals.
Preoperative Planning
Preoperative planning for meniscal transplantation is essential, because meniscus allografts are size and compartment specific. Meniscal sizing measurements are obtained from an AP and lateral radiograph with magnification markers placed on the skin at the level of the joint line. The meniscus width is determined on the AP radiograph (from the edge of the ipsilateral tibial spine to the edge of the tibial plateau), and the meniscus length is determined on the lateral radiograph (the AP dimension of the ipsilateral tibial plateau) (Fig. 4–1). Following correction for magnification, meniscus width is a 1:1 relationship with the calculated measure from the AP radiograph, and meniscus length is determined by multiplying by 0.8 for the medial and 0.7 for the lateral meniscus using the corrected measure from the lateral radiograph. Most commonly, meniscal allografts are either fresh-frozen or cryopreserved. The risk for disease transmission is minimized through rigid donor screening, sterile processing, graft culturing, and polymerase chain reaction testing for HIV.

Figure 4-1 (A) Anteroposterior (AP)and (B) lateral radiograph used to determine meniscus allograft size based on correcting for magnification and obtaining bone measures based on the distance between the tibial eminence and border of the tibial plateau on the AP view (meniscus width) and anterior and posterior border of the tibia on the lateral view (meniscus length) (see text for details).
Surgical Procedure
Examination Under Anesthesia
An examination under anesthesia should be performed to confirm full range of motion and to assess ligament status.
Positioning
Depending on surgeon preference, the patient’s limb may be placed in a standard leg holder or maintained in the unsupported supine position. The posteromedial and/or posterolateral corners of the joint must be freely accessible to perform inside-out meniscus repair. A tourniquet is applied to the proximal thigh and inflated according to surgeon preference. Anesthesia options include general, spinal, and epidural. Most transplants are performed in an outpatient setting.
Diagnostic Arthroscopy
At the time of surgery, meniscal deficiency and the integrity of the articular surface should be performed, to confirm that the patient is a candidate for meniscal transplantation (Fig. 4–2). This must be performed prior to thawing the allograft.
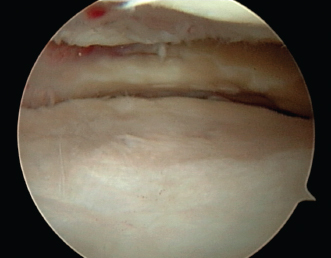
Figure 4-2 Arthroscopic view of same patient imaged in Fig. 4–1 with focal chondral defect of medial femoral condyle and prior subtotal meniscectomy indicated for simultaneous autologous chondrocyte implantation and medial meniscus allograft reconstruction.
Arthroscopic Preparation for Transplantation
The initial steps for medial and lateral meniscus transplantation are similar. First, the remaining meniscus is arthroscopically debrided, leaving a 1 to 2 mm peripheral rim. This is performed using an arthroscopic shaver and hand instruments to achieve punctate bleeding in an effort to promote allograft healing to the knee capsule. Any portion of the anterior horn that is difficult to remove arthroscopically can be removed when the miniarthrotomy is made for allograft implantation. To provide a footprint for a subsequent allograft placement, the remnants of the anterior and posterior horn can be preserved. Debriding the interval between the posterior cruciate ligament (PCL) and bony portion of the medial femoral condyle will facilitate later passage of the meniscus allograft posterior bone plug (Fig. 4–3).
Surgical Technique: Medial Meniscus Transplantation
Arthroscopic Preparation
For medial meniscus transplantation, the authors prefer the double bone plug technique, where a tunnel is used to seat the anterior and posterior horn bone plugs. Following host meniscal preparation, a 9 mm posterior horn tunnel is reamed using an ACL guide (passed through the inferomedial portal) set at 60 degrees with its tip centered on the footprint of the host posterior horn insertion site (Fig. 4–4). The origin of the tunnel is on the anteromedial aspect of the tibia, between the tibial crest and posterior border of the tibia. To ensure anatomic placement of the anterior horn, it is crucial to drill a blind 9 to 10 mm anterior horn tunnel directly through the miniarthrotomy after the posterior horn and plug are secured.
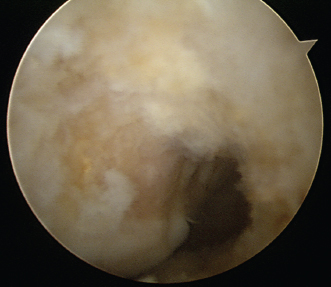
Figure 4-3 Increasing the window between the posterior cruciate ligament (PCL) and medial femoral condyle by debriding the soft tissue and performing a minimal low posterior notchplasty improves visualization of the posterior horn and facilitates posterior horn bone.
Preparation for Meniscal Repair
A standard meniscus repair exposure should be performed on the posterior medial joint line, situated one third above the joint line and two thirds below the joint line. A popliteal retractor is placed to protect the neurovascular structures during an inside-out meniscus repair.
Exposure for Meniscal Insertion
Extending the inferomedial portal distally and excising a small portion of the fat pad allow sufficient access to the joint to remove remaining meniscal tissue, introduce and seat the meniscus in the posterior tunnel, and reduce the meniscus to the periphery. The miniarthrotomy also allows arthroscopic and direct visualization for meniscal repair and creates access to drill the anterior horn blind bone tunnel socket.
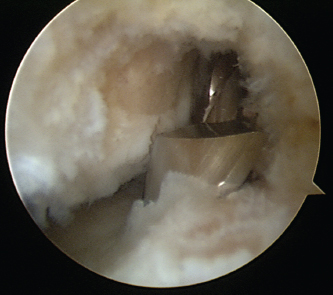
Figure 4-4 A 9 mm cannulated reamer entering the footprint of the posterior horn of the host meniscus.
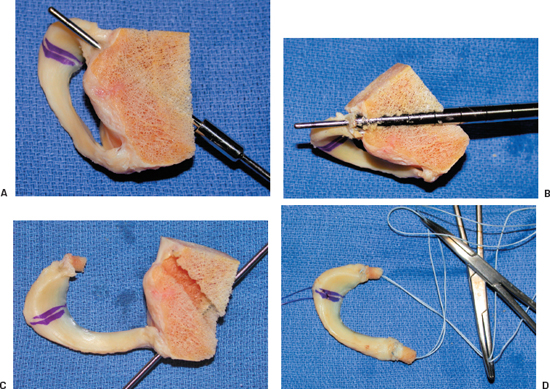
Figure 4-5 Medial meniscus allograft preparation. (A) Collared pin penetrating center of posterior horn at a 60-degree angle to insertion. (B) Cannulated coring reamer to harvest bone plug passed over collared pin. (C) Posterior plug prepared and guide pin in place in preparation for anterior horn coring reamer. (D) Completed meniscus allograft with transosseous nonabsorbable figure-eight sutures and PDS traction suture in place.
Allograft Meniscus Preparation: Medial
The meniscus is properly thawed in normal saline, and all nonmeniscal soft tissue is debrided from the periphery and from around the insertion sites. The bone plugs at the anterior and posterior horns are then fashioned. Using an 8 mm coring reamer, the posterior horn plug is created at a 60-degree angle to the insertion site to match the angle of the posterior tibial tunnel. It is then trimmed to the length of 8 mm with a rongeur. The anterior horn plug is then fashioned using a 9 or 10 mm coring reamer at a 45-degree angle to the insertion site and trimmed to 10 mm in length. A No. 2 nonabsorbable traction suture is first passed in a figure-eight fashion through the soft tissue insertion, and the ends are passed through the center of the bone using a Keith needle. Finally, a No. 1 PDS traction suture is placed at the junction of the middle and posterior one third of the meniscus to aid in reduction of the meniscus (Fig. 4–5).
Meniscal Insertion and Fixation
The first step is proper reduction of the meniscal allograft. A single-barrel zone-specific cannula is placed through the inferolateral portal and is used to advance a nitinol suture passing pin that exits the posteromedial knee capsule at the attachment site of the posterior and middle third of the meniscus. The proximal end of the nitinol pin is retrieved under direct visualization from the medial miniarthrotomy. The No. 1 PDS traction sutures in the allograft meniscus are passed through the loop of the nitinol pin, and the sutures are withdrawn through the medial accessory meniscal repair incision.
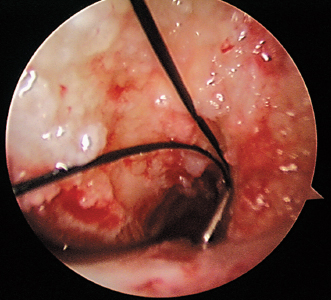
Figure 4-6 Suture passer loop entering joint following placement into posterior horn tibial tunnel in preparation for retrieving allograft meniscus posterior horn transosseous suture to facilitate seating of posterior horn bone plug.
A suture-passing device is then placed retrograde through the posterior horn tunnel (Fig. 4–6). The suture loop is retrieved from the miniarthrotomy and used to pull the No. 2 nonabsorbable sutures that were previously passed through the posterior horn bone plug so as to exit the anteromedial tibia (Fig. 4–7). By placing traction on the bone plug sutures, the posterior horn bone plug can be gently reduced, facilitated by digital and/or gentle instrumented manipulation of the plug as it is advanced between the PCL and medial femoral condyle. Simultaneous valgus stress of the knee in about 30 degrees of flexion and gentle traction on the No. 1 PDS exiting medially facilitate reduction of the soft tissue portion of the graft (Fig. 4–8).
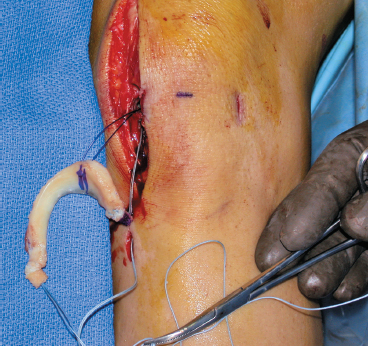
Figure 4-7 Medial meniscus allograft positioned for insertion. Posterior horn transosseous sutures entering medial miniarthrotomy and exiting anteromedial tibia. PDS traction suture entering miniarthrotomy and exiting medial meniscus repair incision.
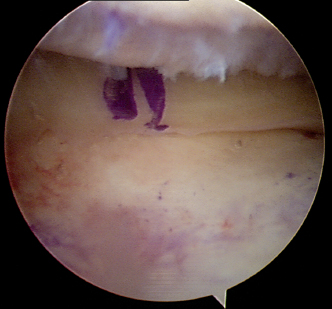
Figure 4-8 Medial meniscus allograft anatomically seated facilitated by gently pulling both traction sutures and manually seating posterior horn bone plug
The meniscus is repaired using inside-out suturing techniques with a vrtical mattress configuration and No. 2–0 nonabsorbable sutures. Sutures are placed on both sides of the meniscus (Fig. 4–9). Once the meniscus is secured, the anterior horn socket is established by creating a blind 1 cm tunnel using a 9 to 10 mm reamer. The bone plug is seated by passing a heavy-gauge needle trans-osseously through the bottom of the tunnel to shuttle the anterior horn sutures through the anterior tibial cortex to reduce and secure the anterior bone plug. These sutures can be tied over soft tissue. In addition, the posterior horn sutures should be tied independent of the anterior horn sutures using a small ligament button (Fig. 4-10). If an articular cartilage procedure is to be performed simultaneously, the arthrotomy is extended, and all remaining steps are completed (Fig. 4-11).
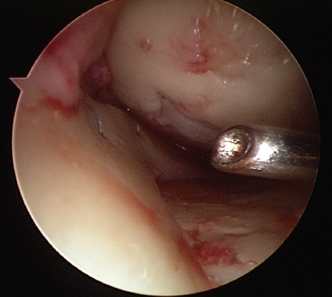
Figure 4-9 Allograft suturing performed by placing vertical mattress sutures on both sides of implant about 3 to 5 mm apart beginning posteriorly and advancing anteriorly.
Surgical Technique: Lateral Meniscus Transplantation
Arthroscopic Preparation
The technique for lateral meniscus transplant usually involves a single bone bridge between the anterior and posterior horns of the meniscus due to their close proximity. The preferred technique of the authors is a slot technique as described, but a “keyhole” technique can also be performed. Once the meniscectomy is completed (as previously described), the slot for meniscus transplant is created. First, an accessory portal through the lateral border of the patellar tendon is created and used to create a line connecting the center of the anterior and posterior horn attachment sites using electrocautery. A 4 mm bur is used to create a superficial reference slot equal to the height of the bur and parallel to the sagittal slope of the tibial plateau, along the line previously marked (Fig. 4-12).
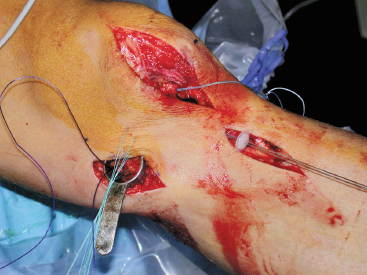
Figure 4-10 Clinical photograph demonstrating meniscus repair sutures exiting medially (some placed transcutaneously, which will be retrieved from beneath the sartorius fascia), posterior horn sutures exiting the anteromedial tibia in preparation for fixation over a ligament button, and anterior horn sutures exiting from the miniarthrotomy prior to drilling the blind bony tunnel for the anterior horn bone plug.
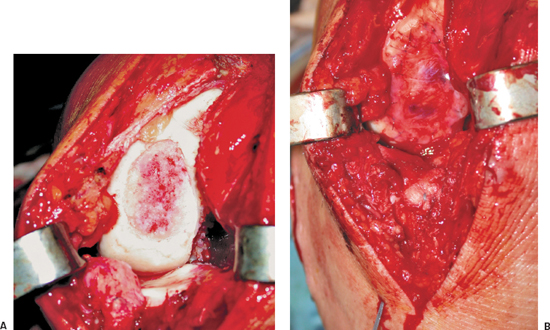
Figure 4-11 (A) Defect in medial femoral condyle exposed through extension of arthrotomy and (B) prepared for simultaneously performed autologous chondrocyte implantation.
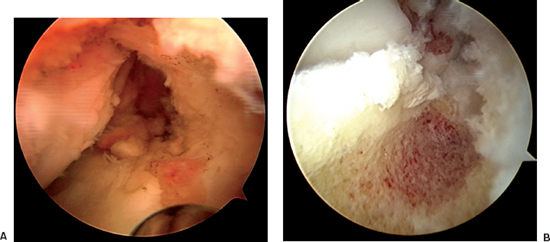
Figure 4-12 Reference slot prepared using (A) arthroscopic shaver and (B) arthroscopic bur in line with anterior and posterior meniscus horns.
All subsequent steps including instrumentation and introduction of the meniscus are performed through the transpatellar tendon accessory portal that is extended as needed. A level slot should be confirmed by placing a depth gauge in the reference slot. Using a drill guide, an insertion pin is placed under fluoroscopic guidance in a parallel fashion (Fig. 4-13). Care should be taken to be sure that the pin does not overpenetrate the posterior cortex. A 7 or 8 mm reamer is then used to drill over the guide, taking care to maintain the posterior cortex of the tibia. A slot 7 or 8 mm in width by 10 mm in depth is created by using a box cutter. Finally, the slot is rasped using the box rasp. Typically, the slot is 8 mm in width following the use of the box rasp. This ensures that the meniscus bone bridge will slide smoothly into the slot (Fig. 4-14).
Allograft Meniscus Preparation: Lateral
This technique creates a rectangular slot that is 1 cm in depth and undersized by 1 mm relative to the tibial slot. The attachment sites of the meniscus are identified on the bone block, and all accessory soft tissue is debrided. The bone bridge is then cut to a width of 7 mm and a height of 1 cm, removing any bone that extends beyond the posterior horn attachment. Bone extending beyond the anterior horn attachment can be retained at this time, because this maintains graft integrity during insertion. A vertical mattress traction suture is placed at the junction of the posterior and middle third of the meniscus using a No. 1 PDS suture (Fig. 4-15).
Meniscus Insertion and Fixation
A single-barrel zone-specific cannula for the inside-out suture technique is placed in the contralateral portal and is used to advance a long nitinol suture passing pin through the knee capsule, at the attachment site of the posterior and middle third of the meniscus. The passing pin should exit the accessory posterolateral incision, and the proximal end of the nitinol pin is then withdrawn from the transpatellar tendon miniarthrotomy site. The traction sutures are passed through the loop of the nitinol pin, and the sutures are withdrawn through the accessory meniscal repair incision. The meniscus is inserted through the arthrotomy while gently pulling on the traction suture, taking care to align the meniscus with the recipient slot. Once the meniscus is reduced, the proper size and position of the meniscus should be confirmed by cycling the knee through its range of motion. An allograft cortical bone interference screw is used to achieve final fixation of the bone bridge in the slot, by placing the screw on the medial portion of the slot over a guide pin (Fig. 4-16). The meniscus is then fixed with standard vertical mattress sutures using an inside-out technique.

Figure 4-13 Drill guide assembly used to place guide pin (lower pin) for cannulated reamer to establish a provisional tibial tunnel in line with the anterior and posterior meniscus horns. The arm of the guide lies intraarticularly and is flush with the subchondral bone of the reference slot prepared in Figure 4-12.
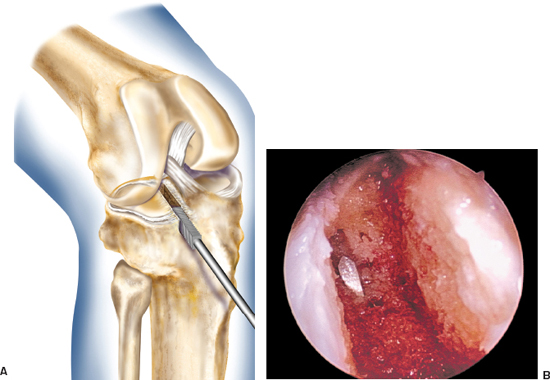
Figure 4-14 (A) Box chisel used to fine-tune definitive recipient slot prior to meniscus insertion. (B) Arthroscopic view of rectangular meniscus slot.
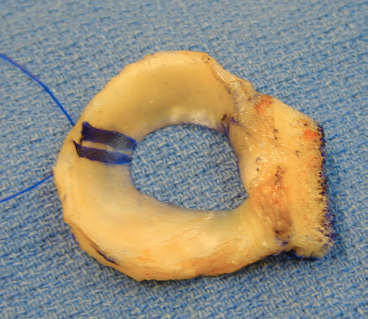
Figure 4-15 Lateral meniscus prepared on bony slot (7 mm width × 10 mm depth).
Closure
Standard closure of the arthrotomy and accessory incisions is performed. A No. 1 Vicryl suture is used to close the knee capsule, and a No. 2 Vicryl suture is used to close the subcutaneous tissue. A No. 3 Prolene running subcuticular suture is used for skin closure. An intraarticular drain is unnecessary in most cases.
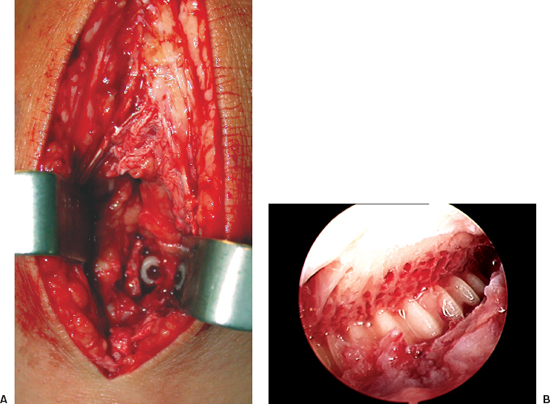
Figure 4-16 Cortical bone interference screw adjacent to meniscus bone bridge seen (A) open and (B) arthroscopically.
Postoperative Management
Following surgery, the patient is placed in a hinged knee immobilizer and is allowed immediate motion from 0 to 90 degrees. We do not routinely use a continuous passive motion machine, unless the procedure is combined with a cartilage restoration technique. Patients are allowed to progress from partial to full weight bearing with crutches over the first 4 weeks postoperation. To protect the meniscus repair, flexion beyond 90 degrees with weight bearing is limited. At 4 weeks, full range of motion is allowed, and gentle strengthening is performed. In-line running is permitted at 12 weeks, and return to full activity is allowed at 4 to 6 months, provided that the lower extremity strength is at least 80 to 85% of the nonoperated leg. Patients are cautioned regarding the inherent risks in returning to highly competitive sports that involve cutting and pivoting.
Tips and Tricks
- To facilitate passage of the meniscus, performing a limited notchplasty along the most inferior and posterior aspects of the femoral condyle adjacent to the origin of the ipsilateral cruciate ligament with a 4.0 mm burr is helpful in visualizing the posterior horn and in passing the meniscus into the appropriate position. In addition, removal of soft tissue in this region greatly facilitates graft passage. We prefer to use an electrothermal ablation device.
- When performing medial meniscus transplant in conjunction with ACL reconstruction, we prefer to place the posterior horn tunnel origin on the lateral side of the tibia. This prevents any possible convergence of the ACL graft tibial tunnel and the meniscus tunnel, which might compromise fixation.
- For lateral meniscus transplantation, the graft must be adequately seated in the slot before fixation. When fixing the graft with the cortical bone screw, a small elevator can be used through the transpatellar tendon miniarthrotomy to hold the slot in place.
- There are several technical considerations when performing concomitant procedures with meniscus transplantation. Patients with a history of meniscectomy who develop secondary varus or valgus deformity should be treated with concomitant high tibial or distal femoral osteotomy, respectively. When performed simultaneously, every effort is made to perform the majority of steps for the meniscus transplant technique first. Otherwise, the varus and valgus stress during the meniscal transplantation procedure could create excessive stress and failure at the osteotomy site. If performed as separate procedures, the limb realignment should be performed first. In addition, any concomitant ligamentous laxity must be addressed at the time of meniscal transplantation. When performing an ACL reconstruction and meniscus transplantation, all of the soft tissue portions of the meniscus transplant technique should be performed first, and then the ACL tibial and femoral tunnels should be reamed prior to meniscus slot or tunnel placement so as to avoid compromise of the ACL reconstruction. If an isolated chondral defect exists, it is not a contraindication to meniscus transplantation and can be treated at the time of meniscal transplantation. It is typically easier and safer for the chondral procedure to be performed after all steps of the meniscus transplant. This will avoid any inadvertent damage to the articular cartilage graft during instrumentation or suture placement.
Pitfalls and How to Avoid Them
- When securing the meniscal allograft, the sutures should be tied over the knee capsule only. On the medial side, one must avoid tying over the sartorius fascia, and on the lateral side, one must avoid tying over the iliotibial band. In addition, the sutures should be tied in knee extension to avoid capturing the knee capsule, which may lead to a postoperative flexion contracture.
- When using the slot technique, it is essential to protect the integrity of the bone bridge. Overreaming the slot by 1 mm relative to the graft will help allow the graft to advance easily through the slot.
Conclusion
Good and excellent results following allograft meniscus transplantation approach 85%, with patients demonstrating a measurable decrease in pain and increase in activity levels (Table 4-1). Persistent symptoms despite meniscal allograft transplantation are most frequently related to improper patient selection. The risk for graft failure seems to be greatest with radiated grafts and in patients with grade 3 to 4 osteoarthritic change. The complications following meniscus transplant are rare and are similar to those following meniscus repair, including incomplete healing of the meniscus repair, infection, arthrofibrosis, and neurovascular injury related to the meniscus repair techniques.
| Study | Mean Follow-Up (Range) | Outcome |
|---|---|---|
| Cameron and Saha1 | 31 months | 58 of 63 (92%) successful |
| Carter2 | 48 months | 45 of 51 (88%) successful |
| Cole et al3 | 2 years minimum | 16 of 20 (80%) successful |
| Garrett4 | 2–7 years | 35 of 43 (12%) successful |
| Goble et al5 | 2 years minimum | 17 of 18 (94%) successful |
| Milachowski et al6 | 14 months | 19 of 22 (86%) successful |
| Noyes and Barber-Westin7 | 30 months (22–58 months) | 56 of 96 (58%) failed (irradiated, grade 3-4) |
| Noyes and Barber-Westin7 | 30 months (22–58 months) | 56 of 96 (58%) failed (irradiated, grade 3-4) |
| Rath et al8 | 5.4 years (2–8 years) | 14 of 22 (64%) successful |
| Rodeo9 | 2 years minimum | 22 of 33 (67%) successful |
| 14 of 16 (88%) bone fixation | ||
| 8 of 17 (47%) no bone fixation | ||
| Van Arkel and de Boer10 | 2–5 years (12–66 months) | 20 of 23 (87%) successful |
References
1 Cameron JC, Saha S. Meniscal allograft transplantation for unicompartmental arthritis of the knee. Clin Orthop Relat Res 1997;337:164–171
2 Carter TR. Meniscal allograft transplantation. Sports Med Arthrosc Rev 1999;7:51–62
3 Cole BJ, Carter TR, Rodeo SA. Allograft meniscal transplantation: background, techniques, and results. Instructional Course Lectures 2003;52:383–396
4 Garrett JC. Meniscal transplantation: a review of 43 cases with two to seven year follow-up. Sports Med Arthrosc Rev 1993;1:164–167
5 Goble EM, Kane SM, Wilcox TR, Doucette SA. Meniscal allografts. In: McGinty JB, Caspari RB, Jackson RW, Poehling GG, eds. Operative Arthroscopy. Philadelphia: Lippincott-Raven; 1996: 317–331
6 Milachowski KA, Weismeir K, Wirth CJ. Homologous meniscus transplantation: experimental and clinical results. Int Orthop 1989;13:1–11
7 Noyes FR, Barber-Westin SD. Irradiated meniscus allografts in the human knee: a two to five year follow-up. Orthop Trans 1995;19:417
8 Rath E, Richmond J, Yassir W, Albright J, Gundogan F. Meniscal allograft transplantation: two to eight year results. Am J Sports Med 2001;29:410–414
9 Rodeo SA. Current concepts: meniscus allografts—where do we stand? Am J Sports Med 2001;29:246–261
10 van Arkel ERA, de Boer HH. Human meniscal transplantation. Preliminary results at 2- to 5-year follow-up. J Bone Joint Surg Br 1995;77:589–595
< div class='tao-gold-member'>









