27 Meniscal Transplantation: Double Bone Plug Technique
The meniscus serves many vital roles in the successful well-being and performance of the knee.1 With the known increased incidence of knee pain and arthritis with meniscal excision, meniscal allograft transplantation has been explored in efforts to decrease or prevent these sequelae.2 Experimental evidence has found the allografts can heal, repopulate with host cells, and have normal appearance.3,4 Early clinical evidence has shown the procedure to be successful in decreasing patients’ symptoms and increasing their activities.5–9 Until long-term studies determine graft durability and capacities to impede arthritis, cautious optimism is appropriate.
Indications
- Knee discomfort localized to the side of meniscectomy
- Chondromalacia of grade III or less in the involved compartment and no appreciable chondromalacia of other compartments
Contraindications
- Grade IV chondromalacia
- Radiographic evidence of flattening of the femoral condyles or appreciable osteophyte formation
- Diffuse knee pain
- Limb malalignment (relative)
- Ligamentous instability (relative)
Physical Examination
- Unremarkable physical findings except possible joint line tenderness
Diagnostic Tests
- Forty-five-degree flexion weight bearing posteroanterior (PA) radiograph, true lateral view, and 30-degree patella view to evaluate the degree of arthritic changes
- Standing full leg length radiograph to evaluate mechanical axis
- Technetium bone scan if there is a question of increased activity isolated to the involved compartment
- Magnetic resonance imaging (MRI) scan if there is a question of extent of meniscus excision or other knee pathology
Special Considerations
Due to the high variability of the anterior horn attachment of the medial meniscus, the double bone plug technique is recommended for medial transplantation.10 With only 1- to 1 1/2-cm distance between the horn attachment on the lateral side, they are typically transplanted with a bone bridge. If there is mechanical malalignment of more than a few degrees or ligamentous laxity, they should be corrected prior to or during the time of the procedure.
Preoperative Planning and Timing of Surgery
- Forty-five-degree flexion weight-bearing PA and true lateral radiographs with magnification marker for graft sizing; MRI or computed tomography (CT) scans are not routinely required.11,12
- If either ligament reconstruction or osteotomy is required, it is routinely done at the same time as the meniscal transplantation. If both are to be performed, osteotomy is done as a separate procedure prior to the reconstruction/transplantation due to the overlap of tunnel and hardware placement.
- Cyropreserved or fresh allografts are recommended, as gamma irradiated or freeze-dried grafts alter the graft’s biomechanic properties.
Special Instruments
- Coring reamer for bone plug harvest (Arthrex, Naples, FL)
- Polyethylene button
Anesthesia
General anesthesia
Patient and Equipment Positions
Routine knee arthroscopy position
Surgical Procedure
- Standard arthroscopic instruments and techniques are used to confirm the need of a meniscal transplant. An assistant prepares the allograft for placement while the surgeon prepares the knee.
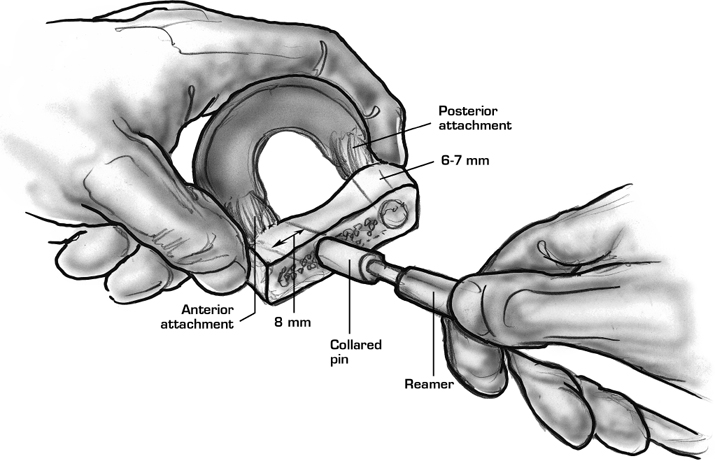
- The allograft bone plugs, which can be fashioned “free hand,” are routinely prepared using coring reamers. A guide pin is placed through the center of the horn attachment with 6-mm-diameter, 8-mm-long posterior and 8-mm-diameter, 10-mm-long anterior plugs harvested. A No. 0 permanent suture is placed through the posterior bone plug incorporating the horn attachment to be used for graft placement. A guide suture is placed in the posteromedial meniscus to aid in subsequent graft passage (Figs. 27–1 and 27–2).
- Meniscal punches and shaver are used to debride the meniscal remnant, leaving a 2-mm, bleeding, menis-cal capsular rim. To save time the anterior one-third can be excised at the time of the arthrotomy.
- To prepare the posterior tunnel, a low-profile anterior cruciate ligament (ACL) guide is placed through the intercondylar notch to deliver a guide pin at a 60-degree angle into the middle of the posterior remnant attachment. A 7-mm-diameter drill is used to make a tunnel 1 mm greater than the bone plug to aid in its reduction.
- An arthrotomy is made, and the posterior bone plug suture is passed down the tunnel using a suture retriever. The meniscal guide suture is placed into the joint and retrieved through a posterior medial incision. Gentle traction is applied to the sutures, while the index finger is used to guide the plug through the notch. With the plug and graft reduced, the bone tunnel suture is tied over the tibia using a polyethylene button (Fig. 27–3).
- The anterior horn attachment is identified and marked with a guide pin. The anterior socket is made to a depth of 10 mm with an 8-mm-diameter drill. The bone plug is then placed in a press fit fashion.
- With graft placement completed, the anterior meniscus is sutured under direct visualization, and the arthrotomy closed. Arthroscopic techniques, typically inside-out sutures, are used to finish the repair of the allograft (Fig. 27–4).
- To prepare the posterior tunnel, a low-profile anterior cruciate ligament (ACL) guide is placed through the intercondylar notch to deliver a guide pin at a 60-degree angle into the middle of the posterior remnant attachment. A 7-mm-diameter drill is used to make a tunnel 1 mm greater than the bone plug to aid in its reduction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








