23 Meniscal Injuries/Repair: Staples
The surgical effort to repair a meniscus rather than remove it recognizes the importance of this structure. The importance of the meniscus in knee stability, load transmission, joint lubrication, and articular cartilage nutrition is clear. Loss of the meniscus leads to degenerative changes over time. Repair approaches include the inside-out, out side-in, and all-inside techniques. Special meniscal repair devices have been developed to facilitate the all-inside repair. Various biodegradable materials are available. Among the more rapid reabsorption profiles is a copolymer of poly L-lactic acid (PLLA) and polyglycolic acid (PGA). Taking advantage of this material, the Polysorb (USS Sports Medicine, North Haven, CT) meniscal staple provides an all-inside repair technique that avoids posterior incisions.
Indications
- Longitudinal, peripheral meniscal tears with a good blood supply. Suitable tears are located at the synovial meniscal junction or in the red/white region.
- Tear length: long tear cannot be accessed well with this technique, but tears between 1.5 and 2.5 cm are appropriate.
- Tears in the posterior medial or posterior lateral corner where other techniques might injure neurovascular structures
- Patients who do not wish to have any secondary incisions associated with the conventional meniscal repair
Contraindications
- Good meniscal blood supply is crucial; therefore, avoid repairs in older patients and horizontal cleavage tears.
- Degenerative articular cartilage change
- Allergy to lactic acid or polyglycolic acid
Physical Examination
- Joint line tenderness
- McMurray’s test (or other meniscal tests) positive
- Effusion
Diagnostic Tests
- Physical examination
- Knee radiographs
- Magnetic resonance imaging (MRI) (sometimes indicated)
Special Considerations
The outside-in, single vertical suture is the “gold standard” for meniscal repair. Other techniques may approach the good results of this technique. Most repairable meniscal tears are found associated with anterior cruciate ligament (ACL) injury. The surgeon performing an ACL reconstruction should also be prepared to repair the meniscus. Healing rates for “isolated” meniscal repairs in stable knees are approximately 80%, whereas in knees undergoing ACL reconstruction the healing rates are 90 to 95%. The Polysorb staple is made of a copolymer of 18% PGA and 82% PLLA. Absorption begins by 3 months and is almost complete within 1 year.1 An inflammatory reaction may be observed. The suture attached to the two rigid prongs of the staple is biodegradable as well and is also composed of the PGA/PLLA copolymer. Evidence suggests that nonabsorbable sutures may provide better results.2
Preoperative Planning and Timing of Surgery
- Early intervention has not been demonstrated to improve the results, but avoiding continued injury to an already torn meniscus is desirable. With the ACL-injured knee, wait until the effusion is resolved and good motion established. This is even more critical when a meniscus repair is performed because of the tendency for postoperative stiffness and swelling to develop.
- The Polysorb staple gun requires careful placement to avoid articular cartilage scuffing and to present the best angle for staple insertion.
Special Instruments
- Polysorb staple gun comes preloaded with six staples
- Operative cannula
Anesthesia
Options are general anesthesia, regional anesthesia, or local anesthesia.
Patient and Equipment Positions
- Patient is supine with knee in leg holder
- Standard knee arthroscopy setup
- Standard anterolateral, anteromedial, or central arthroscopy portals
- View through the ipsilateral (or central) portal; instrument through the contralateral portal
- Operative cannula (8.4 mm X 50 mm) is inserted through the instrument portal
- To access the posterior medial meniscus, hold the knee slightly flexed with valgus stress. Access the posterior lateral meniscus by holding the knee in a figure-four position (~90 degrees) with varus stress.
- Procedures to promote meniscal healing (vascular access channel punch,3 meniscal rasp, synovial abrasion) should be used.
Surgical Procedure
- Establish standard viewing portals. View through the ipsilateral (or central) portal and instrument through the contralateral portal to prepare the meniscus for repair.
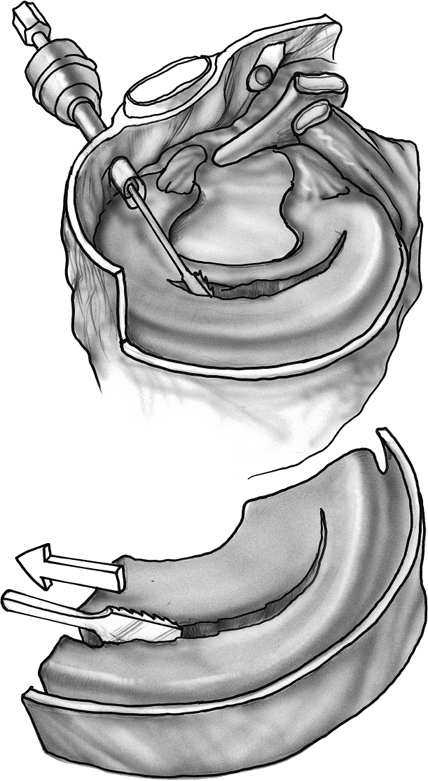
- Encourage a healing response by rasping, creating vascular access channels, and synovial abrasion (Fig. 23–1).
- Place the operating cannula through the portal providing the best access to the tear. The ipsilateral portal works best for posterior horn tears and the contralateral portal works best for middle third tears.
- The stapler is inserted through the operating cannula and its tip is positioned on the superior surface of the meniscal inner rim.
- The sharp points on the stapler nose are placed ~3 mm in from the tear edge and used to carefully maintain meniscal reduction, keeping both sides of the tear in proper position for repair (Fig. 23–2).
- Firm pressure is maintained on the superior surface with the stapler while the handle is slowly pulled.
- A slight recoil occurs when the staple fires.
- Place staples every 3 to 4 mm along the tear (Fig. 23–3).
- Place the operating cannula through the portal providing the best access to the tear. The ipsilateral portal works best for posterior horn tears and the contralateral portal works best for middle third tears.
Dressings, Braces, Splints, and Casts
- A simple absorptive sterile dressing is applied to the skin.
- Compression with Ace bandage.
- Progressive weight bearing with crutches as needed
Tips
- The Polysorb staple is designed only for fixation of longitudinal vertical meniscal tears.
- Place the posterior staple first and then move forward.
- Be certain that the stapler is firmly held against the meniscus.
- Have an assistant hold the leg steadily while placing the stapler and firing it to avoid scuffing the articular cartilage. It is a tight fit!
Pitfalls and Technique Errors
- Although this technique is straightforward, challenges exist!
- The PGA/PLLA staple will degrade more rapidly than the material used in most other meniscal repair devices. Be aware that inflammatory problems may develop.
- Because of the size of the stapler, if the knee is too tight, another technique may be required.
- Although it is difficult to completely staple a long tear, this technique works well with short posterior horn tears.
- Horizontal staple orientation is not an issue because the crosspiece is a suture.
Postoperative Care and Rehabilitation
- For meniscal repairs performed in association with ACL reconstruction, the usual ACL reconstruction protocol should be followed,4 although using meniscal repair devices may require a different rehabilitation program than one used for suture repairs.
- Loaded knee flexion should not exceed 90 degrees for the first 8 weeks.
- Early motion is permitted as swelling decreases.
- Weight bearing as tolerated is permitted.
- When there is no effusion, full extension, and flexion to 135 degrees, straight-ahead jogging is permitted.
- Full pivoting sports may begin when there is no pain, swelling, or reduced motion despite running and agility training.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








