Medial Meniscal Transplant
James R. Romanowski
Christopher D. Harner
INTRODUCTION
One of the earliest treatments for medial knee pain was a total meniscectomy. This procedure, however, led to accelerated arthritic changes and poor patient outcomes (1,10,21). Long-term follow-up (avg: 17.5 years) in patients with prior meniscectomy has shown that 74% of operative knees have arthritic changes versus only 6% of in the nonoperative limb (9). Prospective, 30-year follow-up evaluation of adolescents undergoing total meniscectomy showed the operative knee to have three times the rate of arthritic changes versus the contralateral side (12).
Previously thought of as a developmental remnant, the meniscus’ role in force transmission, biomechanics, and joint stability of a healthy knee gradually was understood and appreciated. The importance in articular force dissipation cannot be understated as even a partial meniscectomy of 16% to 34% can lead to a 350% increase in cartilage contact forces (5,11). Consequently, the focus shifted from cavalier excision toward preservation. Damage to the meniscus can take many forms and the ideal treatment for a torn meniscus is repair. Repair, however, is not always possible, particularly in the degenerative setting or with complex patterns not amenable to healing. In these situations, partial and total meniscectomy may be the result.
Although long-term meniscal transplant outcome studies are limited, short-term results have shown significant improvements in pain and function (5). The preventative role on long-term arthritic joint changes remains unknown.
INDICATIONS/CONTRAINDICATIONS
Young patients with isolated, medial compartment pain and a history of medial meniscectomy are most likely to benefit from a meniscal transplant. There are no specific age limits, but the procedure should be avoided in skeletally immature patients to prevent growth plate damage. The upper age limit is related to arthritic changes in the knee. The Fairbanks classification system and associated articular changes actually were based on patient’s undergoing meniscectomy and are useful for predicting the outcome of surgical graft placement (6). The Outerbridge classification system is also useful for grading articular changes and selecting patients for surgical intervention.
Meniscal transplant has been shown to be more successful in patients with low grade (Outerbridge I, II), unicompartmental arthritic changes (8,15). Relative contraindications include Outerbridge grade III, IV changes as these been shown to have inferior results. Meniscal transplantation with grade IV chondral changes has a 50% failure rate (15,18).
Successful surgical candidates must also have an acceptable mechanical alignment. For medial meniscal transplants, it is particularly important to address varus alignment deformities. A weight-bearing axis that passes through the medial compartment has been shown to have significantly inferior outcomes when compared to transplant patients who have concomitant high tibial osteotomies to neutralize the alignment of the affected limb (2,22). The goal is to shift the mechanical axis laterally and between the intercondylar tibial spines. Failure to address the limb alignment is a relative contraindication to meniscal transplant.
Ligamentous stability is a prerequisite to medial meniscal transplant. It is not uncommon for patients to additionally have ACL dysfunction, and with loss of this primary stabilizer to anterior translation, increased stresses are placed on the medial compartment.
PREOPERATIVE PLANNING
Radiographic imaging is critical for both diagnosis and meniscal graft templating. Standard films include a single cassette bilateral 45-degree flexion weight-bearing posterior-anterior radiograph, a 45-degree flexion lateral of the involved knee, and a sunrise view. Additional imaging should include long cassette bilateral lower extremity radiograph evaluating for any varus or valgus malalignment. Should the history/physical suggest additional pathologies, an MRI may be appropriate. An MRI dedicated to cartilage sequences may provide additional information.
Patients have often had prior meniscal or ligamentous surgery. In cases where enlarged bony tunnels are present in the setting of a dysfunctional or absent ACL, a staged reconstruction with bone grafting may be necessary. The interval for definitive surgery is usually 4 to 6 months to allow the bone graft to incorporate.
Deformities resulting in varus or valgus malalignment require osteotomies. If a single stage correction is desired, a closing wedge osteotomy should be pursued as opening wedge methods with graft add complexity and additional concerns of nonunion.
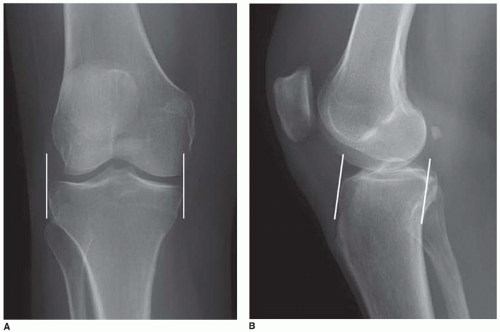
Many methods exist for sizing the medial meniscal allograft. Radiographs, CT scans with and without contrast, MRI, as well as the patients height have all been used for assessing the needed graft dimensions (17). Perhaps the most reliable and cost-effective method is using ipsilateral AP and lateral plain radiographs. The actual coronal width is determined on the AP radiograph as the distance between the medial and lateral metaphyseal margins (Fig. 24.1A). Sagittal width is determined by measuring the distance between a line parallel to the anterior tibia and a second line perpendicular to the articular surface at the posterior margin of the medial tibial plateau (Fig. 24.1B). The sagittal value is multiplied by 0.8 conversion factor. Osteophytes are not included within the measurements.
SURGERY
Anesthesia
The patient is identified in the preoperative holding area and the surgical site is verified, marked “yes,” and signed. An anesthetic regimen is chosen after discussion with the patient, anesthesiologist, and surgeon. General anesthesia is often utilized and augmented with regional blocks for postoperative pain control.
SETUP, PATIENT POSITIONING, AND EXAM UNDER ANESTHESIA
The patient is transferred to a standard operative table and placed supine. After the induction of anesthesia, a Foley catheter is inserted as part of fluid management. An exam under anesthesia is performed. It is not uncommon to have associated ligamentous pathology; therefore, a careful exam is necessary. Ranges of motion and ligamentous stability are assessed through Lachman, pivot shift, anterior/posterior drawer, and varus/valgus stress testing at 0 and 30 degrees. The patient’s heels are even with the end of the operative table and a bump is placed under the ipsilateral hip. The involved extremity is flexed to 90 degrees and a second bump is secured with tape to allow the heel to rest in this position during surgery. A lateral post is placed at the level of the greater trochanter to allow the extremity to balance in the flexed position and prevent it from falling into abduction (Fig. 24.2). It is not necessary to use a tourniquet.
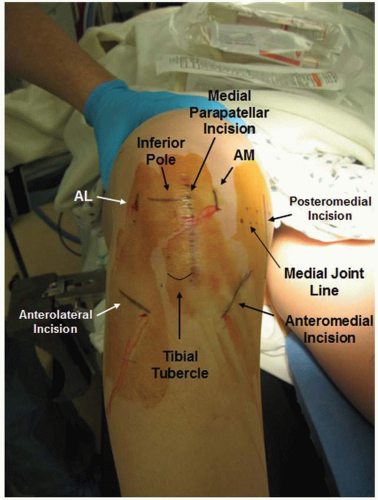
ANATOMIC LANDMARKS AND INCISIONS
The identification of several anatomic landmarks is necessary as multiple incisions are made for placement of the meniscal allograft. Once the surgical incisions are marked, a subcutaneous injection of 1% marcaine with 1:200,000 epinephrine is placed under each site. The superior and inferior poles of the patella, patella tendon borders, tibial tubercle, medial joint line, and anterolateral tibial crest are identified (Fig. 24.3). The patient is then sterilely prepped and draped. The following incisions are placed with the knee positioned in 90 degrees of flexion. Standard anterolateral and anteromedial (AM) arthroscopy portals are utilized. The anterolateral portal is made on the lateral border of the patellar tendon at the level of the inferior pole of the patella and extended distally approximately 1 cm. The AM portal is also started at the same level, but approximately 1 cm medial to the medial border of the patellar tendon. A medial parapatellar arthrotomy is utilized for securing the anterior horn of the allograft to that of the native meniscus. This incision is just medial to the patellar tendon beginning at the level of the inferior pole of the patella and extended distally to the joint line. The incision may incorporate and extend distally from the AM portal. As an extensile approach, it may be further extended for tibial tunnel
placement when additional ACL reconstruction is necessary. It remains imperative to recognize the joint line as some patients have patella baja that may risk further damage to the meniscus when the inferior pole is used as a reference. Oftentimes, patients may have prior surgical incisions and it may be necessary to incorporate these as part of the approach.
placement when additional ACL reconstruction is necessary. It remains imperative to recognize the joint line as some patients have patella baja that may risk further damage to the meniscus when the inferior pole is used as a reference. Oftentimes, patients may have prior surgical incisions and it may be necessary to incorporate these as part of the approach.
 FIGURE 24.2 The patient is positioned with the knee flexed at 90 degrees, secured by a lateral post on the thigh and bump at the foot. |
A posteromedial (PM) incision is also necessary for placement of the transplant allograft. Similar to inside-out meniscal repair techniques, the vertical incision is placed over the PM joint line, just posterior to the MCL. Approximately one third of the incision is superior to the joint line and two thirds is distal. Careful attention is paid toward identifying and avoiding the saphenous nerve. The PM portal is established early for visualization of the posterior meniscal root, while the arthrotomy is not necessary until allograft passage.
An anterolateral incision is necessary for anterior and posterior meniscal root tunnel placement. This curvilinear incision is placed along the anterolateral border of the proximal tibia at the level of the tibial tubercle and extends for approximately 4 cm. The anterior compartment is entered via a similar curvilinear fascial incision and subperiosteal elevation pushes the tibialis anterior musculature laterally as to protect the underlying neurovascular structures.
An outflow portal is utilized and, with the leg in full extension, is marked at the level of the superior pole of the patella and at the lateral border of the vastus lateralis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree