Chapter 39 Medial Ligamentous Injuries of the Knee
Acute and Chronic
Anatomy and Biomechanics
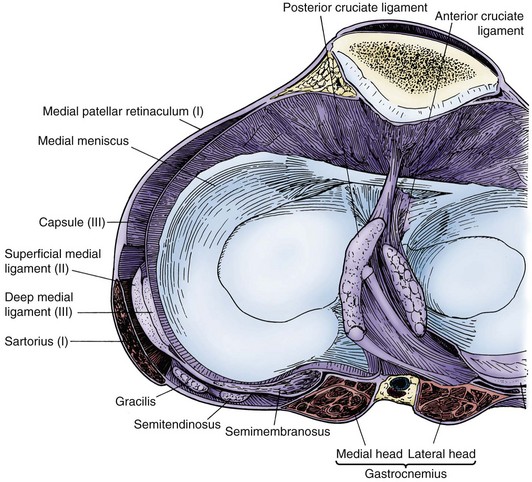
The anatomic study by Warren and Marshall provides the basis for knowledge of the medial side of the knee.43 In their classic paper, these authors described medial knee anatomy using a spatial concept of three distinct layers (Fig. 39-1). Layer 1 consists of the crural fascia of the knee and is present from the patella anteriorly to the popliteal fossa posteriorly. The sartorius fascia is found in this layer and blends with the crural fascia anteriorly as it attaches to the tibia. The gracilis and semitendinosus tendons are found between layers 1 and 2.
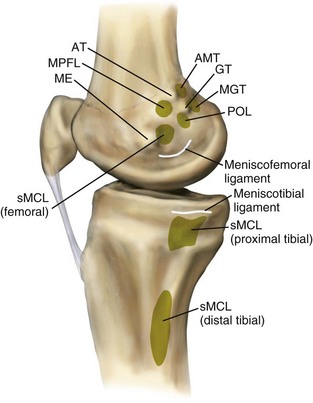
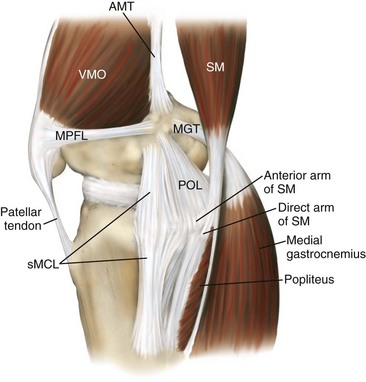
Layer 2 is the superficial medial collateral ligament (sMCL), which, in the absence of scarring, can be easily identified deep to the gracilis and semitendinosus tendons once the crural fascia is incised. In a quantitative study, LaPrade found that the sMCL was attached to the femur an average of 3.2 mm proximal and 4.8 mm posterior to the medial epicondyle25 (Fig. 39-2). The tibial attachment of the sMCL has two divisions, with the proximal division attaching to soft tissue and the distal division attaching directly to the posteromedial tibia. Vertically oriented fibers of the sMCL anteriorly blend with more obliquely oriented fibers in the posterior portion of the knee capsule and semimembranosus insertion at the posteromedial corner (Fig. 39-3). This blending of tissue planes forms the posteromedial capsular pouch enveloping the medial femoral condyle.
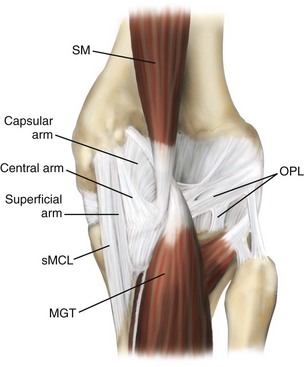
The third and final layer of the knee consists of the knee joint capsule. This capsule thickens from anterior to posterior, and a distinct component of the capsule deep to the sMCL represents the deep medial collateral ligament (dMCL), which has meniscofemoral and meniscotibial attachments but no attachment to the overlying sMCL.25 The nomenclature describing the structures of the posteromedial corner has become better defined in the orthopedic literature.20,25,35 The posterior oblique ligament (POL) has been identified as a thickening of the posterior medial capsule (PMC) in this region, and its importance in medial stability has become increasingly recognized. The POL attaches proximally and posteriorly to the attachment site of the sMCL on the femur. The previously described oblique portion of the sMCL is now recognized as the POL. The POL has superficial, central, and capsular arms; the central arm is the most robust of the three and is the primary portion of the POL that should be repaired or reconstructed upon medial injury (Fig. 39-4). The posteromedial capsule is further reinforced by contributions from the semimembranosus and its sheath through multiple attachments.
In contrast to the anatomic nomenclature, little debate exists regarding the biomechanical role of the medial knee structures. Robinson found that the anterior aspect of the sMCL remained taut throughout motion, while the PMC consistently loosened in flexion and tightened in full extension and internal rotation.35 Griffith et al demonstrated that both divisions of the sMCL serve as primary restraints to valgus load and external rotation, and that the degree of knee flexion affects the load response.15 Additionally, the POL serves as a restraint to internal rotation and valgus at and approaching full extension, and exhibits a flexion-dependent reciprocal role in resistance to internal rotation with the sMCL. In a second biomechanical study, Griffith et al further defined the primary static stabilizers of the knee.14 These authors found that the proximal division of the sMCL serves as the primary stabilizer to valgus stress, the distal division of the sMCL serves as the primary stabilizer to external rotation at 30 degrees of flexion, and, when viewed as a single functional unit, the sMCL serves as a primary restraint to valgus and internal rotation at all flexion angles and to external rotation at 30 degrees of flexion. The primary restraints to internal rotation were the POL and the distal sMCL division at all flexion angles. Additionally, investigators found that the dMCL made an important contribution to flexion-dependent internal rotation stability. Wijdicks et al reported that these relationships and load values changed with sequential cutting of structures, demonstrating the intricate load-sharing properties of the medial knee structures.45
Diagnosis
The amount of joint line opening with valgus stress at 0 and 30 degrees determines the grade of the MCL injury. Comparison is made with the uninjured knee, with <5 mm of increased opening indicating a grade I injury, 5 to 10 mm indicating grade II, and >10 mm termed grade III. Placing a finger along the joint line and comparing with the uninjured knee helps to quantify the amount of joint line opening. The quality of the endpoint should also be recorded. Increased laxity in full extension is indicative of injury to the POL and often indicates a combined ligament injury, most commonly an ACL tear. Fetto found an 80% incidence of combined ligament injury with grade III MCL tears.9 Attention should be paid to rotational instability as well. The posteromedial corner complex limits internal rotation (IR) of the knee, and increased rotational motion should raise suspicion of injury to this structure. Increased external rotation (ER) has been primarily attributed to lateral side and posterior cruciate ligament (PCL) injury. However, Griffith demonstrated that the sMCL serves as a primary restraint to ER, and this should be considered during that portion of the examination.14 Visual inspection of the tibia during ER will help determine whether the increased ER is related to medial or lateral injury. Injury to the medial structures will result in rotation of the anteromedial tibia anteriorly; in contrast, the posterolateral tibia will effectively fall away when increased ER results from a lateral injury. Often, with multiligamentous injuries, an examination under anesthesia is needed to determine the degree of functional integrity of collateral ligaments.
Imaging
Magnetic resonance imaging (MRI) has become an invaluable tool in assessment of the medial ligamentous structures; it can define the location and quality of the MCL injury (Figs. 39-5 and 39-6). In addition, MRI allows evaluation of the knee for meniscal lesions, osteochondral injury, and damage to other ligaments. Distal avulsion of the MCL with displacement superficial to the pes tendons, similar to a Stener lesion in the thumb, may indicate the need for operative repair. Rubin compared MRI findings versus findings at the time of surgery and noted diagnostic sensitivity and specificity of 94% and 99%, respectively, for ligament and meniscal damage with an isolated injury.36 These values decreased to 88% and 84%, respectively, when two or more structures were damaged. Additionally, Rasenberg et al noted a high degree of agreement between instrumented grading of MCL injury and grading by MRI.33 Miller et al noted that trabecular microfractures or “bone bruises” occurred in 45% of patients with isolated MCL tears, and that all of these injuries resolved in 2 to 4 months on follow-up imaging.28 The information obtained on MRI should be correlated with the history and physical examination findings to determine the extent of injury and develop an appropriate plan of care for the patient.

Figure 39-5 Coronal magnetic resonance imaging (MRI) of a proximal medial collateral ligament (MCL) rupture.
Treatment
Brace Wear
Prevention of MCL injuries has been studied extensively. Prophylactic knee braces (PKBs) are commonly used in collegiate down linemen football players to protect the medial knee structures. Several studies have shown that PKBs decrease strain on the MCL.5,10,11 Surrogate modeling in vitro testing demonstrates that bracing decreases forces across the MCL by 20% to 30%, and that custom bracing provides improved protection over off-the-shelf versions.5 Although these models have been validated, obvious limitations are seen when a surrogate knee model loaded in an in vitro setting is compared with an athlete’s knee injured during competition.
Similar to laboratory testing, clinical studies have demonstrated some limited protective benefit of PKBs in certain sporting populations.1,2,40 Sitler analyzed the effects of prophylactic knee bracing on knee injury in West Point cadets playing full contact American football.40 The incidence of MCL injury was decreased in braced defensive players compared with unbraced controls. However, the severity of injury was not affected by brace wear. Additionally, in a study sponsored by the Big Ten football conference, Albright et al showed that linemen, linebackers, and tight ends were at highest risk for MCL injury, and that bracing consistently decreased injury rates both at practice and in games.2 The linebacker and tight end groups were less likely to wear PKBs, citing concern for performance limitations with the brace.
Performance effects of prophylactic knee bracing have been well documented. Styf et al showed that intramuscular pressures increased with brace wear and raised the potential for early muscle fatigue as a result.41 Greene demonstrated that some braces worn to protect against knee injury might cause decreased speed and agility.13 With the trade-off of protection for performance, a decision must be made as to which athletes benefit most from prophylactic bracing.29 The most common practice consists of PKB use in offensive and defensive down linemen, with skill position players opting to perform without braces.
Isolated MCL Injury
Injury to the MCL results in a robust healing response because of its blood supply, relatively wide surface area, association with other secondary stabilizers, and extra-articular location. These factors contribute to the well-documented ability of the MCL to heal without the need for surgical repair or reconstruction. In the absence of injury to secondary stabilizers, particularly the ACL, acute MCL injuries will heal with rare exception. In a rabbit model, Frank showed that MCL injuries at the proximal or distal insertion sites were slower to heal than those seen with midsubstance disruption.12
The mainstay of treatment for isolated MCL injury has long been nonoperative with an expectation of good outcomes.* Lundberg et al reported that patients treated nonoperatively with grade I or II MCL injury can expect good return of function, normal to near normal stability, and no increased risk of osteoarthritis at 10-year follow-up.27 The authors believed that exclusion of additional ligament injury, namely, anterior cruciate ligament (ACL) injury, was imperative for successful treatment of these injuries. Indelicato et al followed 21 athletes for a mean of 46 months with isolated grade III MCL injuries treated nonoperatively and demonstrated 95% good and excellent results.21 Average return to full contact sport occurred 9.2 weeks after injury for the group, and all athletes with remaining college eligibility returned to play football. Holden et al treated 51 football players with grade I and II MCL injuries nonoperatively, and 80% of the players returned to sport in an average of 21 days.19 The 20% of players who failed to complete rehabilitation were found to have previously unrecognized injury associated with the ACL and/or the medial meniscus. The authors stressed that truly isolated injury to the MCL could be treated nonoperatively with an expectation of good functional results, and that vigilance is required to detect other potential injuries, because their presence consistently compromised the results of rehabilitation. Jones et al reported on 24 high school football players with isolated grade III MCL injury treated nonoperatively.22 Twenty-two of the 24 athletes returned to football in an average of 34 days.
Although no standardized rehabilitation protocol for isolated MCL injury exists, several basic tenets of treatment are typically employed. First, the knee is stabilized in a brace to protect against a second valgus insult. Bracing may also improve pain control and may allow the injured athlete to participate more actively in the rehabilitation program. Second, early motion and weight bearing are encouraged and improve the rate and quality of the healing response.42 Third, quadriceps and hamstring strengthening is started early in the process to prevent deconditioning and to optimize the function of the knee’s dynamic stabilizers. The decision to allow athletes to return to play is dictated by their pain level, functional improvement, and stability on examination. In a prospective study of athletes with grade III MCL injury, Reider instituted a functional rehabilitation program that adhered to these principles.34 At 5-year follow-up, the mean Hospital for Special Surgery (HSS) knee score was 45.9, and the authors believed that the functional, nonoperative treatment of these injuries with functional rehabilitation produced results as good as those attained with surgical treatment or immobilization, without the treatment-related morbidity noted with those two approaches.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree