12 MECHANISM OF INJURY
In Webster’s Dictionary, trauma is defined as “an injury or wound to a living body caused by the application of external violence.” Injury is a public health problem of vast proportions. In 1999 injury was the leading cause of death for persons ages 1 to 34 and was the fifth leading cause of death overall.1 There were 29 million nonfatal injuries from all causes in 2005 for a rate of 9,871 per 100,000.2 Some 93% of these injuries were unintentional.
Mortality is the most common way to assess the impact of injury. In 2004 there were 167,184 injury deaths in the United States, for a rate of 57 per 100,000. The most common cause of injury death was motor vehicle crashes, with a total of 44,933 deaths and a rate of 15.30 per 100,000.2 Among people age 65 and older, falls are the most common cause of injury death and nonfatal injuries.1
Another way to measure the impact of injury to our society is to examine the years of potential life lost.3 Unintentional injury accounts for more than 2 million years of potential life lost before the age of 65, compared with 1.8 million for cancer and 1.4 million for cardiovascular disease. Suicide and homicide each account for more than a half million years of potential life lost.
A final method to evaluate the effect injury has on society is to estimate the cost of injury, done by the National Safety Council.4 These estimates of the costs of unintentional injury emphasize the value of preventive initiatives that reduce unintentional injury rates. Their estimates are provided as averages. In 2005, the economic cost of a death was $1,150,000; for a nonfatal disabling injury it was $52,900 and for a nondisabling injury it was $7500. These figures do not include long-term costs for the disabling injuries. An estimate in 1995 dollars places the total injury costs at $260 billion.1 However you assess impact, injury remains a major drain on our society.
RISK FACTORS
AGE
Death rates from injuries are highest in patients age 75 or older.5 A factor contributing to this high death rate in the elderly may be presence of associated medical conditions.5,6 The in-hospital fatality rate for this group is 15% to 30% compared with 4% to 8% in younger patients.5 In patients with rib fractures, the mortality rate for patients older than age 55 is twice that for those younger than age 55.7,8
The highest injury rate occurs in persons between the ages of 15 and 341 because of their participation in high-risk activities. Poor judgment associated with the use of alcohol and drugs also contributes to the high injury rate. The lowest injury rate is for children ages 5 to 14.1 The highest homicide rate occurs among people ages 15 to 24.1 Suicide rates for both sexes show little variation with age. The incidence of domestic violence is highest among women between ages 16 and 24.9
Specific injury mechanisms and risk of injury also vary by age. The elderly suffer a disproportionate number of falls, as well as pedestrian-related injuries.10,11 They are more likely to suffer significant injury with minimal energy transfer.10 Assault among elderly patients is recognized as a health care problem. During 2001, more than 30,000 persons age 60 and older were treated in U.S. emergency departments for nonfatal assault injuries.12 This is a rate of 72 per 100,000 population. Rates were highest among the 60- to 69-year age group. Although not well recognized, some of these assaults probably represent elder maltreatment.13
GENDER
Injury rates are highest for 15- to 24-year-old males.1 The mortality risk for males is 4.6 times that for females, possibly because of male involvement in hazardous activities. The unintentional injury death rate for males peaks between ages 15 and 24. It is the third most common cause of death for males and females in the 45- to 54-year age group.1 The rate of homicide is among the top three causes of death for males ages 10 to 34.1 In females, the death rate peaks at ages 15 to 19 for unintentional injury and at 20 to 24 for homicide. Women in their late 40s have the highest suicide rate. Nonfatal injury rates for men and women do not differ significantly, suggesting that injuries to males are more severe than those to females.1
Domestic violence is more often directed against females than males.14 In 1996, 75% of the approximately 1,800 homicides perpetrated by an intimate partner involved a female victim. An intimate partner is responsible for 28.5% of homicides in women ages 18 to 24 compared with only 2.5% of male victims.9 In addition to those hospitalized as a direct result of intentional injury, intimate partner violence is much more prevalent in patients admitted for unintentional injury than in the general population. It is related to alcohol use disorders in both the perpetrator and the victim.15
RACE AND INCOME
Injury death rates vary according to race and socioeconomic level. In a depressed economy the suicide and homicide rates increase and the number of motor vehicle crashes (MVCs) decreases.16 Native Americans (Indians, Eskimos, and Aleuts) have the highest death rate from unintentional injury regardless of income. In 1999, this was estimated to be 61 per 100,000 population.1 African Americans have the highest homicide rate. Caucasians and Native Americans have the highest suicide rate. Asian Americans (Chinese, Japanese, Koreans, Hawaiians, Filipinos, Guamanians) have the lowest death rates from unintentional injuries, homicide, and suicide. The unintentional injury rate is higher in low-income areas than in the wealthiest areas. An inverse relationship exists between income levels and death rates for African Americans and Caucasians; that is, the higher the income, the lower the death rate. This relationship is maintained for domestic violence.17
ALCOHOL
Alcohol not only contributes to injury-producing events, such as MVCs, it also can increase the severity of injury.18 Alcohol is a major factor in many motor vehicle, home, industrial, and recreational injuries and in crime, suicide, and family abuse.19 Unhealthy alcohol use is believed to occur in 4% to 30% of the population.20 Alcohol abuse occurs in 5% and alcohol dependence in 4% of the population. Recent evidence suggests that alcohol interventions in a trauma center may reduce the risk of injury recurrence.21 A brief intervention regarding alcohol consumption resulted in fewer arrests in the subsequent 3 years for driving under the influence of alcohol.22 The value of these brief interventions for patients with acute alcohol intoxication has been endorsed by the American College of Surgeons Committee on Trauma in their trauma center verification program since 2006.23
RURAL VERSUS URBAN
Patterns of injury differ between rural and urban environments. A major difference is a higher intentional injury rate in large urban areas. Homicide is highest in cities. Suicide is 80% greater in rural areas than in metropolitan areas. Clearly the physical environment has an important influence on injury rate.24 Overall mortality rates from injury are higher in rural communities compared with urban communities. When considering MVCs, the higher mortality might be related to road characteristics, lower use of seatbelts, reduced density of traffic enforcement officials, slower detection of crashes, and distance to the closest trauma center. In rural settings, agricultural equipment is another source of injury, especially among children. Cuttings and machinery injuries are also common causes of injury in rural environments.25 Falls are a common unintentional injury in rural and urban communities. Urban and rural environments share poisoning as a common unintentional injury. However, urban poisonings are commonly medications and household chemicals, whereas rural poisonings are usually related to agricultural products.
INITIAL ASSESSMENT AND HISTORY
In the initial evaluation of the trauma patient, a careful history of the events leading to the injury must be obtained. The practitioner must attend to urgent therapeutic needs along with the usual diagnostic evaluation.26 Obtaining an accurate history—especially asking about the mechanism of injury—can help identify likely injuries and thereby reduce morbidity and mortality.
Answers to questions about the circumstances of the impact are helpful when assessing potential injuries sustained in a motor vehicle–related crash (such as automobile, motorcycle, and pedestrian injuries). At the site of the incident, prehospital care personnel should quickly survey the scene, noting the appearance of the vehicle(s) involved and the damage sustained to the passenger compartment. It is important to know the speed the vehicle involved was traveling, the point of impact, and the type of impact (single-vehicle, high-speed, front-end, rear-end, or T-bone intersection collision). In a MVC with a combined speed of 30 miles per hour, near-side lateral impact crashes have the highest risk of injury, followed by far-side lateral impact and frontal crashes.27 The evaluating team should determine whether the patient was the driver or the passenger, whether safety devices (safety belt, child safety seat, and airbag) were used, and where the victim was found at the scene. Death of an occupant in the vehicle should alert the team to potential energy forces within the collision. Patients from a vehicle in which an occupant has died and individuals who are ejected from a vehicle have a higher morbidity and mortality and warrant a thorough evaluation for injury.
Frontal-impact collisions that cause a bent steering wheel or column, knee imprints in the dashboard, or a broken windshield are associated with head injuries, hemopneumothoraces, injuries to the spleen or liver, and dislocation of the patella.28,29 Femur fractures with or without posterior fracture-dislocation of the ipsilateral hip must be considered. Deceleration injuries such as aortic rupture and small bowel injury must be ruled out.
Side-impact collisions produce contralateral neck sprains, cervical fractures, head injuries, lacerations to the soft tissues, lateral rib fractures or flail chest, abdominal injuries, and pelvic and acetabular fractures. Although the mechanism is not as classic as frontal deceleration, aortic injuries often result from side-impact collisions. The risk is significantly higher for near-side rather than far-side impact.30
Rear-impact collisions result in hyperextension neck injuries, and there may be rebound frontal-impact injuries. Ejection from the vehicle produces a multitude of injuries, such as penetrating impalement wounds, head injuries, cervical fractures, and road burns. Ejection increases not only the risk of injury, but the risk of serious injury.27,31
Pedestrians hit by vehicles may have many injuries. The prehospital team should identify (or estimate) how fast the vehicle involved was traveling, the type of vehicle, the point of impact, and whether the victim was thrown or dragged. Waddell’s triad (Figure 12-1) occurs when a pedestrian is struck by a car.32 Age influences both type and severity of injuries.33 When the victim is a child, injuries are caused by three events: (1) the bumper and hood impact the femur and/or chest, (2) the victim is thrown upon impact, and (3) the contralateral skull is injured by the force of impact upon hitting the ground. One of the resulting injuries is often missed in the initial evaluation. Adult pedestrians receive a lateral impact from contact with the bumper and hood, injuring the lower and upper leg, because adults try to protect themselves by turning sideways (Figure 12-1). Fractures to this area are recognized, but ligament damage in the other knee is often overlooked.
A quick, thorough physical examination must be performed during or immediately after resuscitation. It is important to systematically examine the undressed patient to avoid overlooking injuries. Injuries are easier to detect in patients with penetrating trauma than in those with blunt injury, because surface injury may or may not be present with blunt injury. Failure to diagnose the patient’s injuries correctly is associated with a high mortality rate.28 An index of suspicion for associated injuries based on the mechanism of injury must be maintained.
Some body areas do not lend themselves easily to physical examination, such as the cranium, vertebral column, and bony thorax. Injury may exist without classic signs, but the mechanism of injury may raise suspicion enough to warrant further diagnostic examinations. Examples include computed tomography (CT) for diagnosis of brain injury, CT or angiography for blunt chest injury and possible aortic injury, and plain radiography, CT, and magnetic resonance imaging for spinal column evaluation.34 Specific protocols to evaluate certain types of injury may help identify injuries while conserving resources. All tests must be performed without placing the patient at risk of further injury. The patient is reexamined continually to identify changing physical findings.
Complete assessment of the trauma patient is aided by knowing the cause of injury. MVCs are the most common cause of injury, followed by falls. Other causes of injury are pedestrian collision, drowning, fire, burn, explosion, poisoning, firearm, assault, aspiration, machinery, and sports activity. In some cases the cause can be related to an expected pattern of injury. For example, distinct injury patterns may be found with sports-related trauma associated with sudden deceleration (diving, falling), excessive forces (twisting, hyperextension, hyperflexion), or changes in momentum (boxing). Because of repeated blows to the head in boxing, cumulative brain damage may occur, with resultant neurologic damage depending on the affected area. Spinal cord injuries can occur while participating in gymnastics or playing football. Head injuries can occur while playing football or horseback riding. Skiing can produce fractures, and knee injuries are common with skiing and football. This information plus the events preceding the incident can provide clues to the practitioner regarding the patterns of injuries, expected severity of injury, and possible occult or missed injuries.28 Common areas where injuries are missed include the extremities (hand and foot), upper extremities (forearm and upper arm), and skin (scalp lacerations). Repetitive examinations and review of information after admission will detect missed injuries in 10% of patients.35,36
MECHANISM OF INJURY
BIOMECHANICS
The field of biomechanics involves a variety of disciplines, including engineering, physiology, medicine, biology, and anatomy.37 Knowledge of injury mechanisms allows the appropriate biomechanical measurements to be made to characterize injuries. Many approaches are used in this field of inquiry, and research is best conducted with representatives of as many of the disciplines as possible. For example, the Crash Injury Research and Engineering Network (CIREN) program uses a multidisciplinary approach to explain the injuries that result from car crashes and direct biomechanical research to improve car safety.38
INJURY CONCEPTS
Among the factors that influence injury are velocity of collision, object shape, and tissue rigidity. Body tissue has inertial resistance as well as tensile, elastic, and compressive strength. Tensile strength equals the amount of tension a tissue can withstand and its ability to resist stretching forces. Elasticity is the ability of a tissue to resume its original shape and size after being stretched. Compressive strength refers to the tissue’s ability to resist squeezing forces or inward pressure. Whenever the force exceeds maximum tissue strength, a fracture or tear occurs.39
The more slowly the force is applied, the more slowly energy is released, with less subsequent tissue deformation. If the same force is dissipated over a large surface area, the tissue disruption is further reduced. The forces most often applied are acceleration, deceleration, shearing, and compression. Acceleration is a change in the rate of velocity or speed of a moving body. As velocity increases, so does tissue damage. Deceleration is a decrease in the velocity of a moving object. Shearing forces occur across a plane, with structures slipping relative to each other. Compressive resistance is the ability of an object or structure to resist squeezing forces or inward pressure.39
Viscoelastic properties of tissue help absorb energy and protect vital organs from the effects of impact. If the energy transmitted to the tissue remains below the limit of injury, the energy will be absorbed without causing injury.40 This phenomenon is used to protect against injury by using energy-absorbing structures and padding. These protective objects do not prevent deformation of tissues but can extend the duration and reduce the force of impact below the limit of injury.
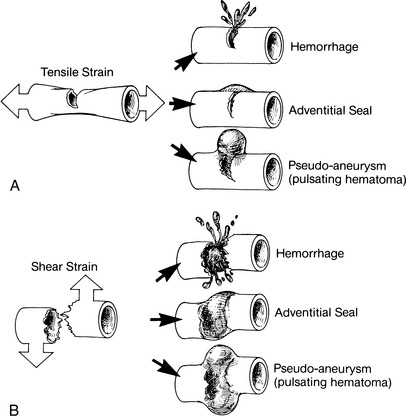
When the tissues are deformed beyond the recoverable limit, injury occurs. Tissue or structure deformation can be measured according to changes in shape, commonly defined as a change in length divided by the initial length. Another term for this change is strain. Two major types of strain are tensile and shear. A third type is compressive, which is less common and is responsible for crushing injuries. Tensile and shear strain applied to an artery is illustrated in Figure 12-2. Stretching of the artery along its longitudinal axis increases its length and tissue strain. If the strain or increase in length is too great, the tissue will break. An “all or none” phenomenon is not present, so the artery may completely or partially break. A similar result can be produced by a force applied at 90 degrees to the long axis of the artery. This shear strain occurs when the movement of tissue in opposite directions exceeds recoverable limits. Other examples of tensile strain injuries are femur and rib fractures. Shear strain injuries include hepatic vein laceration from differential movements of hepatic lobes and brain injury from movement of the brain within the skull. Compressive or deformation strain is a factor in contusion injury. This type of injury often leaves the surface of the tissue undamaged (Figure 12-3).
Another factor in strain injury is the loading or strain rate.41 Tissue response depends on both strain and rate of strain application. Bony injuries can be used to demonstrate this principle. Compact bone will fail at lower strain values if the strain applied is at a rapid rate. The same strain applied more slowly will not cause tissue failure. In general, the viscous tolerance of a tissue is proportional to the product of loading rate and amount of compression. A tissue’s tolerance to compression decreases as the rate of loading increases.
Our overall knowledge regarding injury mechanisms for specific organ systems continues to improve. The CIREN has been instrumental in enhancing our knowledge regarding injuries in MVCs.38 The mission of this program is to improve the prevention, treatment, and rehabilitation of MVC injuries, thereby reducing deaths, disabilities, and human and economic costs. CIREN is sponsored by the National Highway Traffic Safety Administration and uses a multidisciplinary approach to investigate crashes. Information from this program demonstrates that proper seat belt restraint reduces head injury from frontal crashes, but not lateral crashes.42 Also, belts do not prevent abdominal injuries in lateral crashes, and contact intrusion injuries commonly cause brain, liver, and lung injuries. Many engineering changes in vehicle design can be traced to findings made by CIREN investigations.
Impact biomechanics is an important aspect of injury mechanisms, especially for MVCs. Impact biomechanics has four principal areas of study: (1) understanding the mechanism of injury, (2) establishing levels of human tolerance to impact, (3) soliciting the mechanical response to injury, and (4) designing more human-like test dummies and other surrogates.43 The following discussion covers trauma caused by blunt, thermal, and penetrating mechanisms and the various organ responses to these forces.
BLUNT INJURY
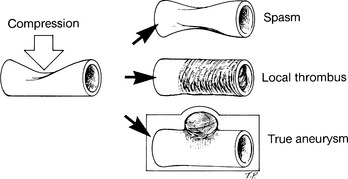
Acceleration-deceleration forces are a common cause of blunt injury. An example is injury to the thoracic aorta. Rapid deceleration in MVCs can cause major vessels to undergo stretching and bowing. Thoracic deceleration leads to nonphysiologic stretching of localized aortic regions. Shearing is produced when stretching forces exceed the elasticity of vessels. Shearing damage is seen in the vessel walls, causing them to tear, dissect, rupture, or form an aneurysm.44 The aorta is fixed by the left subclavian artery and the ligamentum arteriosum. Movement of the aorta above and below this fixation point produces a shearing force, causing injury (Figure 12-4). Although aortic injuries are most commonly seen after frontal MVCs, side-impact acceleration-deceleration also occurs, as side-impact collisions are responsible for up to 30% of aortic injuries.45 The lowest rate of aortic injury in MVCs is associated with use of three-point restraint belts and an air bag.46 Similar deceleration occurs in falls from heights greater than 12 feet, and in pedestrians struck and thrown significant distance.44
Previous attempts to define the patient population at risk for aortic injury have not identified many factors beyond a sudden, violent deceleration. This potential for significant deceleration obtained from the history is key in making the diagnosis of this injury, as the physical examination is often unrevealing. Visible chest wall injury is present in less than 50% of patients with blunt aortic injury. In addition, a normal chest radiograph on hospital admission is not uncommon among patients with a blunt thoracic aortic injury.47
BRAIN INJURIES
The Centers for Disease Control and Prevention (CDC) estimates that at least 5.3 million Americans or about 2% of the U.S. population currently have a long-term or lifelong need for help to perform activities of daily living secondary to an injury to their brain.48 Traumatic brain injury (TBI) ranges from mild, when there is a brief change in mental status or consciousness, to severe, when the individual has an extended period of unconsciousness or amnesia after the injury. Approximately 75% of TBIs that occur yearly are concussions or a mild form of TBI.49
One review suggests approximately 1.4 million people sustain a TBI each year in the United States. A number of outcomes are possible for these patients. It is estimated that 50,000 die, 235,000 require hospitalization, and 1.1 million are treated as outpatients.50
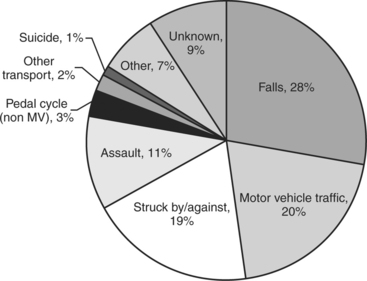
Falls are the most common cause of brain injury followed by motor vehicle crashes (Figure 12-5). Primary brain injury is produced by the initial impact. The impact can cause skull fracture, brain contusions, hematomas outside or within the brain, lacerations of the brain as it moves across the inner surfaces of the skull, and diffuse axonal injury, which is felt to be secondary to shear forces applied to the various nerve fibers within the brain. Secondary brain injury can increase the severity of brain injury. It is caused by a number of physiologic vascular and biochemical effects. These events can occur secondary to brain swelling with increased intracranial pressure, hypoxemia, systemic hypotension, electrolyte changes, and a number of other factors.51 The value of preventing secondary brain injury is suggested by outcome data that show aggressive control of factors known to exacerbate secondary TBI, such as intracranial pressure, in the brain-injured patient lowers mortality.52 (The reader is referred to Chapter 20 for more extensive information of this topic.)
A confounding problem with brain injuries is their high incidence in the elderly who may be taking anticoagulants. An elevated coagulation profile secondary to warfarin in the head-injured patient will worsen the outcome. Early reversal of anticoagulation with fresh frozen plasma improves outcomes.53
SPINAL CORD INJURIES
The soft tissue and bony supports of the spinal cord are insufficient to tolerate violent forces. Spinal injuries are most prevalent in the cervical region where the vertebrae are small, a high degree of flexibility is conferred, and there is less strength in stabilizing structures (i.e., bones, ligaments, muscles). Mechanisms of injury involved with spinal cord damage include penetration, axial loading, flexion, extension, rotation, lateral bending, and distraction54,55
In hyperextension injuries the spine is bent back sharply. A downward force causes compression of the vertebral bodies. Fracture of the pedicles or lamina can be seen, depending on the direction and intensity of the force.54 Posterior dislocation of the upper vertebrae on the lower occurs, further complicating the injury. These injuries can squeeze the spinal cord, supplying the main stress in the center of the cord, resulting in the syndrome of acute central cervical cord injury. In this syndrome, there is greater motor impairment of the upper limbs compared with the lower because the motor nerve fibers supplying the lower limbs are more peripherally situated and suffer less damage.
Hangings are associated with distraction injury to the cervical spine, a separation of the spinal column with cord stretching.55 The axis pedicle fractures seen in MVCs are often called hangman’s fractures but actually have a different mechanism. The hangman’s fracture is caused by severe hyperextension and distraction between C1 and C2. The fracture seen in patients after an MVC or fall is caused by extension, axial compression, flexion, and disk disruption. Neurologic involvement is not common. Whiplash injury is another form of cervical spinal column injury that has three components that may cause injury. These include extension, downward loading, and rebound.56
FRACTURES
Some basic definitions used to describe fracture biomechanics are helpful in understanding possible injuries. Force and strain have already been discussed and defined. Stress is defined as the internal resistance to deformation or the internal force generated from the application of a load.41
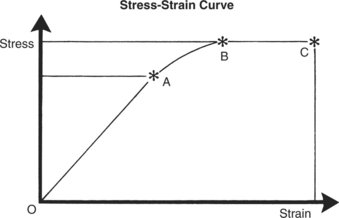
Both extrinsic and intrinsic factors are important determinants of whether a bone will fracture when stress is applied. Extrinsic factors include magnitude, duration, direction, and rate of force application. Intrinsic factors are properties of bone that determine its susceptibility to fracture. These include energy-absorbing capacity, modulus of elasticity (Young’s modulus), fatigue, strength, and density.39 Energy-absorbing capacity is related to the strain characteristics of the bone. Stress-strain curves (Figure 12-6), or Young’s modulus, measure elasticity. Fatigue failure occurs when a material is subjected to repeated stresses that are below its breaking point but the cumulative stress results in failure. Bone strength is directly related to its density. As bone density is reduced by osteoporosis, the stress required to fracture the bone decreases.
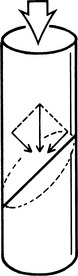
Fractures can be classified by their mechanism of injury. Fractures caused by direct trauma are tapping, crush, low-velocity penetrating, and high-velocity penetrating. Tapping injuries occur from blows to bony areas (e.g., kicks to the shin, hit with a nightstick). Little energy is absorbed by soft tissue. Crush and high-velocity injuries produce multiple comminuted areas as well as soft tissue damage. Indirect trauma also can produce fractures. Traction injuries usually involve tendons pulling pieces of bone away at their attachments, such as external rotation injuries of the ankle. Angulation fractures are explained by tension and compression stress. As a lever is angulated, the convex surface is under tension stress and the concave surface is under compression stress. The convex surface fails first, giving rise to a transverse fracture. Rotational fractures are rare because it is difficult to apply a true rotation force to a bone. Compression fractures do occur and are explained by vector analysis. If a homogeneous cylinder is loaded axially until it fails, the fracture will appear at an angle of almost 45 degrees (Figure 12-7). Because bones are not homogeneous, most axial loading produces T- or Y-shaped fractures at the lower end of the bone. Combinations of forces usually produce oblique or curved fracture lines.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree