30 TRAUMA IN THE ELDERLY
The aging of our population represents a significant change in the national demographics, which has a major impact on the delivery of health care. Projections by the U.S. Census Bureau indicate that by 2050 more than 20% of the population will be over the age of 65 years.1 That is an 8% increase from the predictions made for 2000. This is in large part due to the aging of the baby boom generation, where more than 75 million babies were born between 1946 and 1964. In response to this projected population growth of people over the age of 65 years, the elderly have become an increasingly common focus of health care research in the last decade. This ever-growing number of elderly patients and their susceptibility to injuries make them one of the larger and increasingly important consumers of health care in terms of resources and dollars.2 The Fiscal Year 2007 budget request for the Administration on Aging is $1,338,000.000.3 This budget is designed to accelerate the key systems changes needed to prepare the nation for the aging and long-term care needs of the baby boom generation.3
EPIDEMIOLOGY
Trauma is the seventh leading cause of death in Americans older than age 65 years.4 The elderly are more frequently injured from low-energy and household incidents. Their injuries are disproportionately severe and they are more likely to have comorbid conditions, suffer complications, and die after trauma.5 Elderly trauma patients account for 25% of all injury fatalities per year and consume 33% of the health care resources spent on trauma care.6 Unintentional injury deaths in individuals aged 65 years and older are primarily due to three causes: motor vehicle crashes (MVCs), falls, and thermal injuries. MVCs are the most common cause of death from trauma through age 79 years. More than 40 million older adults will be licensed drivers by 2020.7 These drivers are involved in only a fraction of the total MVCs. However, although they drive a lower number of miles, and are less likely to drink and drive than other adult drivers,8 those over the age 75 years have a higher fatality rate from MVCs than those in any other age group. These statistics yield little information about the causes of the MVC but would suggest that someone is more likely to die in a collision involving an elderly driver than in a collision involving a younger driver.
Among adults aged 80 years and older, falls are the leading cause of injury deaths.9 In 2003, more than 1.8 million seniors aged 65 years and older were treated in emergency departments for fall-related injuries and more than 421,000 were hospitalized.10 Of those who fall, 20% to 30% have moderate to severe injuries that reduce mobility and increase the risk of premature death.11 Falls are the leading cause of traumatic brain injury in older adults.12 Multiple causative factors such as balance impairment and substance abuse issues are often suggested as precursors to falls.
Death as a result of thermal injury accounts for approximately 4% of all unintentional deaths in individuals aged 65 years and older.13 Thermal injuries include flame burns, scalds, inhalation injury, direct and indirect contact with heat sources, and electrical injury.
There were 852 homicides reported in 2002 of people aged 60 years and older.14 Although the number of homicides of people aged 65 years and older has been decreasing, this age group still has the highest percentage of homicides during the commission of a felony.15
As the U.S. population ages, public health efforts have expanded to ensure the independence, function, and safety of older adults. Approximately 33,000 people aged 60 years and older in the United States were treated in hospital emergency departments for nonfatal assault-related injuries in 2001, with injuries occurring disproportionately among persons ages 60 to 69 years.16 Some of the injuries probably represent a form of elder maltreatment, which refers to acts of commission or omission that result in harm or threatened harm to the health and welfare of an older adult, occurring within any relationship in which there is an expectation of trust.17 The various forms of elder maltreatment include physical, sexual, and psychologic abuse; abandonment; exploitation; and neglect, either intentional or unintentional. For every reported incident of elder maltreatment, an estimated five incidents are unreported.18
A 50-state survey found that Adult Protective Services received 472,813 reports of elder abuse in domestic and institutional settings in 2000. Eighty-four percent of the reports received were investigated and almost half were substantiated. Adults over the age of 80 years were the most frequent victims of abuse, excluding self-neglect.19 In a recent analysis of nursing home inspections and complaint investigations from 1990 to 2000, it was found that more than 9% (1,601 homes) were cited for causing actual harm or immediate jeopardy to residents. More than 30% (5,283 homes) were cited for an abuse violation that had the potential to cause harm.20 The National Aging Resource Center on Elder Abuse estimates that 20% of elder abuse victims experience financial exploitation.21
Between 1 and 2 million Americans aged 65 years and older have been injured, exploited, or otherwise mistreated by someone on whom they depended for care or protection.22 Health care providers often unintentionally overlook elder abuse and neglect, explaining a fracture or weight loss as expected or normal consequences of the aging process.23 Health care practitioners have a responsibility to work with law enforcement and social service agencies to respond appropriately to these growing problems affecting the elderly population.
PATTERNS OF INJURY
Thermal injuries in the elderly have higher mortality rates compared with similar injuries in the young. When the burn-related mortality rate is compared with age, it is usually expressed as the percentage of burn that leads to a 50% mortality rate. Mortality is 50% in a young adult with a burn covering 80% of total body surface area (TBSA); in a person aged 60 to 70 years, a burn of 35% TBSA has a 50% mortality rate; in a person over age 70 years, a burn of 20% TBSA has a 50% mortality rate.24
INJURY THRESHOLD
INCREASED PERSONAL RISK
The aging process produces unique changes in an individual’s functional status, which contributes to increased susceptibility to injury and mortality. The process of aging is characterized by the progressive loss of function and functional reserve of organs in times of physical and metabolic stress.25
Finally, the combination of medications with the use of alcohol, in both the younger and older populations, can clearly result in impaired perception and response and can often lead to injury. The incidence of alcohol dependence and abuse has been increasing among the elderly population.26 Every elderly trauma patient should be evaluated for alcohol use to minimize morbidity and mortality rates. Elderly patients who abuse alcohol are at risk to experience acute alcohol withdrawal and are particularly at risk for this because of their age-related physiologic changes or conditions. Their use or abuse of alcohol may have been occurring for years but has now escalated to the point of causing an event that has resulted in injury. Older adults can reach a higher blood alcohol concentration sooner than young drinkers because of a decrease in total body fluid.26 Obvious symptoms of alcohol use would include the smell of alcohol on the patient’s breath, slurred speech, or difficulty paying attention. Minor symptoms of withdrawal can begin 6 to 12 hours after the last drink and can peak within 24 to 36 hours.26 These symptoms can include tachycardia, hypertension, nausea, and tremors26; however, these nonspecific signs can often be mistaken for common problems experienced by elderly patients and should be evaluated against the patient’s known preexisting conditions and the current trauma-related clinical presentation.
RESUSCITATIVE PHASE
ASSESSMENT
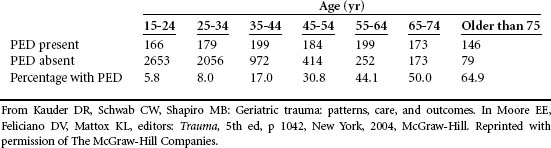
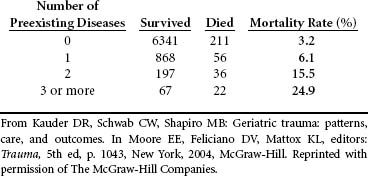
Just as with the younger trauma population, resuscitation of the elderly trauma patient should be rapid and efficient. However, a rapid and thorough assessment of the injured elderly patient may be more difficult, particularly if unfounded or inaccurate assumptions are made of the pre-trauma condition. Assessment itself can be complicated in cases when an older person presents with preexisting conditions. Although the presence of any chronic illness has not been a direct predictor of death in elderly patients with injuries, comorbid conditions have been associated with increased mortality rates, varying with the type and number of conditions25 (Tables 30-1 and 30-2).
Cardiovascular Considerations
Cardiovascular disease is one of the most common medical problems in the elderly and often leads to death in this population. Age is a major risk factor for cardiovascular disease, which accounts for more than 40% of deaths in those >65 years old.27 Diminished cardiac reserves may not affect the daily functioning of a healthy older individual, but when an elderly person has physiologic stress, such as from blood loss or hypoxia, the lack of reserve becomes apparent through cardiac dysfunction.28 Some elderly patients may be unaware of cardiac dysfunction or may have few, if any, symptoms until the time of traumatic injury or stress. As is true for all trauma patients, initial measurements of blood pressure are likely to be misleading because of compensation or prior dysfunction. The presence of “normal” vital signs may mask severe physiologic compromise.
Hypertension is one of the more common preexisting conditions in the elderly population. Diastolic dysfunction is also common in the elderly, particularly in those with hypertension, and is responsible for up to 50% of cases of heart failure in patients older than age 80 years.29 Some patients may be taking medications to treat hypertension. Both the hypertensive state and the medications can alter physiologic compensatory mechanisms and obscure signs of shock. For example, in an elderly patient taking a prescription β-blocker to treat hypertension, heart rate may not increase in response to trauma, hypovolemia, or injury-related stress. Decreased β-adrenergic receptors and diminished catecholamine release can both result in the inability to raise the maximum heart rate needed to respond to stress and can also prevent the heart from normalizing quickly after stress.
Warfarin (Coumadin) is the fourth most commonly prescribed cardiovascular agent and the eleventh most prescribed drug in the United States.30,31 The use of warfarin anticoagulation therapy in the elderly population is typically for the treatment of atrial fibrillation, cardiac valve replacement, venous thrombosis, and pulmonary embolism. Controversy exists over whether warfarin therapy increases the risk of complications from hemorrhage. Two studies highlight the differences of opinion.
A Michigan Level I trauma center study evaluated 159 consecutive trauma patients who were taking warfarin and compared their outcomes to a group of age-matched patients with head injuries who were not taking warfarin. Fifty-nine percent of patients in the warfarin study group had some type of head trauma, of which 27% had intracranial injuries, defined as evidence of subdural, subarachnoid, epidural, intraparenchymal, or intraventricular hemorrhage on computed tomographic scan.32 Of the 15 patients (9.4%) who died, an international normalized ratio (INR) of 3.3 was found compared with the INR of 3.0 that was found in those who survived. Of 70 age-matched patients with head trauma not taking warfarin, 47 (67%) had intracranial injury and 5 of those died (10%). In conclusion, the preinjury use of warfarin does not place the trauma patient at increased risk for fatal hemorrhagic complications in the absence of head trauma. Intracranial injury was strongly associated with a mortality rate significantly higher than patients with head trauma who were not taking warfarin.32
Conversely, in New York, a 7-year chart review was completed on all anticoagulated patients over age 65 years with minor head injuries. Only 32 patients were identified for inclusion in the study. Twenty-four patients were discharged from the emergency department without hospitalization. Three of the remaining eight patients had initial Glasgow Coma Scores between 14 and 15 but became comatose within 3 to 4 hours. A fourth patient was comatose 6 hours after injury. Three of these four patients died, leading to the conclusion that anticoagulated patients with even minor head trauma are at risk for neurologic deterioration within 6 hours of injury despite a seemingly normal neurologic examination.33
Serum troponin is a specific and sensitive marker of myocardial injury. An increase in serum troponin I of greater than 1.2 mcg/L after trauma is related to the degree of overall myocardial injury and physiologic stress and not mechanical chest trauma.34 Obtaining a baseline 12-lead electrocardiogram, cardiac enzymes, and troponin level is suggested. Additionally, serial electrocardiogram and laboratory studies should be completed with evidence of myocardial infarction or elevated cardiac enzymes, particularly the creatine kinase-MB isoenzyme or troponin levels.
The effect of aging on the cardiovascular system supports the use of hemodynamic monitoring in the elderly. Continuous monitoring should be instituted rapidly in elderly patients to assess trends and patterns of cardiovascular response. Invasive monitoring such as arterial lines, central venous pressure lines, and pulmonary artery catheters should be considered early in the course of treatment despite iatrogenic risk to provide more reliable assessment of cardiovascular performance and guidance of fluid replacement therapy. In addition, early and aggressive resuscitation and invasive monitoring have been shown to improve outcomes in the elderly trauma population. Scalea et al35 suggested that the elderly may appear hemodynamically stable while experiencing inadequate perfusion, which may result in delays in the recognition and treatment of underperfusion, leading to increased mortality.
Pulmonary Considerations
As a person ages, the pulmonary system undergoes physiologic changes such as increased work of breathing, which can lead to the need for ventilatory support after traumatic injury. Elderly patients have a decreased respiratory reserve and may decompensate more quickly than do younger patients.28 The pulmonary arteries thicken, increasing pulmonary vascular resistance. The lung parenchyma and chest wall become stiff, leading to diminished pulmonary compliance. Alveolar ducts enlarge and alveoli become flatter and shallower, decreasing the lung vital capacity and increasing the expiratory reserve volume, which can lead to ventilation-perfusion mismatching. Respiratory muscle fibers atrophy, decreasing respiratory muscle strength and thus heightening the elderly patient’s risk for respiratory fatigue in the face of traumatic injury. Diminished lung cilia can lead to an increased risk of pulmonary infection and aspiration. Additionally, chronic lung disease and cigarette smoking compromise the overall respiratory function and reserve when stressed.
Arterial blood gas measurements typically show a moderately reduced oxygen tension (such as a partial pressure of arterial oxygen [PaO2] of 80 mm Hg), whereas other values are within normal limits. Changes in values other than PaO2 should be interpreted in the context of the injury. Measurements across time remain essential for determining trends. In elderly patients with blunt chest trauma resulting from both falls and MVCs, multiple fractured ribs are the most common injury.36 Elderly patients who sustain blunt chest trauma with rib fractures have twice the mortality rate of younger patients with similar injuries.36 As the number of rib fractures increases, so does the incidence of pneumonia and death.36,37 A key factor in the management of rib factors is adequate pain management to provide the opportunity for pulmonary hygiene and prevention of pulmonary complications.
Neurologic Considerations
Careful assessment should be made for evidence of intracranial bleeding, particularly in trauma associated with falls and MVCs. Even minor head injuries can lead to intracranial vessel injury resulting in a subdural hematoma or subarachnoid bleeding. Cerebral atrophy, which is normal in aging, results in greater cranial space where a significant amount of blood can accumulate before any neurologic symptoms appear. Pupillary responses tend to be sluggish in the elderly, and assessment may be further complicated by eye disease such as glaucoma or previous surgery such as cataract. Several factors can affect an accurate neurologic examination in the elderly trauma patient. Determining what is normal from what is new should be done through frequent reassessments of patient’s condition.
Musculoskeletal Considerations
Cervical spine fractures in elderly patients are increasingly common as the population ages. Controversy exists over surgical stabilization versus halo vest immobilization treatment of cervical and high thoracic injuries in the elderly because of associated higher rates of cardiac and pulmonary morbidity and mortality rates with the use of halo vest immobilization.38 The decision about how to treat different patterns of cervical spine fractures is complex and often controversial. The same bony injury may have acceptable rates of healing whether treated operatively or nonoperatively. One must then consider risks and potential complications of each type of treatment and how quickly the patient will regain an acceptable functional status.39
In older patients, pelvic fractures are more likely to cause hemorrhage and require intervention. Fracture patterns differ in older patients; although severe pelvic fractures are more common in young patients, lateral compression type fractures occur more frequently and cause significant blood loss in the elderly population.40 Outcomes for older patients with pelvic fractures are also significantly worse than in younger patients. Atherosclerosis is an extremely common disease in elderly patients, and this may limit the ability of injured vessels to develop vasospasm and spontaneously tamponade. Significant blood loss needs to be addressed either by external fixator application, although this will not help lateral compression fractures, or by angiography and embolization. Blood transfusions also may be needed.40
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree