28 THE PREGNANT TRAUMA PATIENT
The pregnant trauma patient presents a double challenge: two lives must be treated concurrently. When the trauma patient is pregnant, response to shock is different, and unique injuries, life threatening to both the mother and the fetus, can occur. While caring for the pregnant trauma patient from resuscitation through rehabilitation, the nurse must assess the patient, interpret the assessment findings, and make decisions pertinent to the patient’s care. The nurse is the integral link between the many specialists consulting with the pregnant trauma patient. Therefore, it is essential for the nurse to develop a firm knowledge base and proficient assessment skills regarding the needs of this unique patient population so that sound decisions can be made to enhance the care of both mother and child.
EPIDEMIOLOGY
The number of births and the fertility rate in the United States increased by nearly 1% in 2004.1 With 4.1 million births in 2004, it stands to reason there are a large number of pregnant women in our society. Trauma has become the leading nonobstetric cause of morbidity and death during pregnanacy.2 The most common causes of traumatic injuries for the pregnant population include motor vehicle crashes, physical abuse or interpersonnel violence, falls, firearm injuries, and burns.3–8 Early studies identified the number of pregnant patients treat-ed at specific trauma centers and emergency departments and their mechanisms of injury. At one major trauma center, 79 injured patients admitted over a 9-year period were pregnant. This total represents less than 1% of total acute admissions, 1.7% of all female admissions, and 2.6% of women of childbearing age (14 to 45 years, now considered 12 to 51 years) admitted.9 In this study, blunt mechanisms of injury had been incurred by 96% of the study population and penetrating mechanisms had injured 4%.
More recent studies, such as the 10-year retrospective review by Baerga-Vaula et al,3 also found that pregnant trauma patients represent a small portion of trauma admissions, less than 1% per year. A slightly higher percentage was noted in an 8-year study from the University of New Mexico Health Science Center. That study of 15,268 trauma patients identified 271 who were pregnant victims of blunt trauma, or 1.8% of trauma admissions.10
Over the past decade, studies have attempted to characterize patterns of injury and risk factors that predict fetal death. This is clinically significant because fetal mortality can be as much as three times higher than maternal mortality. Fetal loss was higher in patients with a higher Injury Severity Score (ISS), evidence of shock, and abdominal injuries.10
A 5-year Canadian study looked at factors associated with high fetal mortality rates in patients with an ISS of more than 12. The most common mechanism of injury was motor vehicle crash. Fetal death was correlated with higher maternal ISS, lower maternal hemoglobin level, and greater number of blood transfusions plus the presence of disseminated intravascular coagulation (DIC).11 In a large multi-institutional study of factors associated with fetal death, similar results were noted. Fetal death was associated with a higher ISS, a decreased Glasgow Coma Scale score, and lower admitting maternal pH. Many of these patients arrived in shock, with the fetus in distress.12
Historically, motor vehicle crashes have been the leading cause of death for women aged 12 to 51 years, which are generally considered the childbearing years.13 There are nearly ten times more fatalities from motor vehicle crashes than from any other mechanism of injury during the reproductive years.14 This is clearly supported in numerous multicenter studies that reviewed trauma during pregnancy and found that motor vehicle crashes are the most significant mechanism of injury.3–5,7–9 In the past, pregnant women secluded themselves and traveled less often, but pregnant women of today continue to drive and ride in vehicles until the time of delivery, and many of them do not use protective restraints properly or at all.6
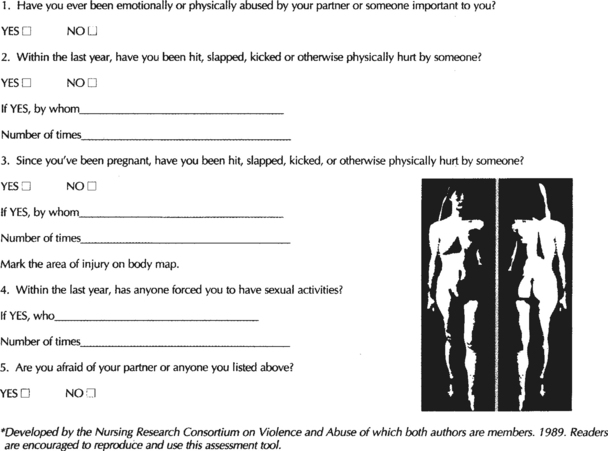
Physical abuse, or interpersonal violence, is a common source of trauma during pregnancy. In the United States, an estimated 1.5 to 1.8 million women annually are victims of violence from male partners or cohabitants.15 As many as one in five women has been battered by her male partner.15 Parker et al16 documented that 20.6% of pregnant teenagers and 14.2% of pregnant adults were physically abused during pregnancy. In a review of 13 studies on violence against pregnant women, Gazmararian et al17 found that the reported prevalence of violence during pregnancy ranges from 0.9% to 20.1%. A review of 1,195 pregnant patients from the American College of Surgeons National Trauma Data Bank found that interpersonal violence accounted for 11.6% of trauma during pregnancy6 (Figure 28-1). Physical abuse during pregnancy has been associated with low fetal birth weights, low maternal weight gain, and a higher maternal incidence of hypertension, anemia, infections, and first- and second-trimester bleeding.16,18 Additionally, intimate partner violence during pregnancy is associated with significantly higher maternal rates of depression, suicide, and tobacco, alcohol, and drug use.19,20 Women who claim to have fallen but whose injuries do not seem to match the described event may have been victims of assault. They must be interviewed in private to investigate the possibility of abuse.21
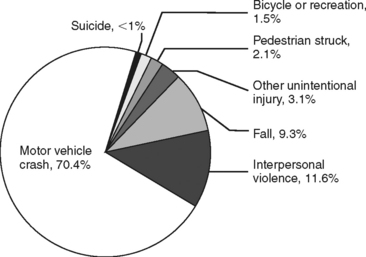
FIGURE 28-1 Mechanism of injury data for 852 pregnant women of childbearing age.
(Redrawn from Ikossi DG, Lazar AA, Morabito D et al: Profile of mothers at risk: an analysis of injury and pregnancy loss in 1,195 trauma patients, J Am Coll Surg 200:49-56, 2005.)
Penetrating injuries resulting from ballistic trauma and stab wounds also occur during pregnancy. Historically, firearms have been second only to motor vehicle crashes as a cause of fatal injury. A classic study from the Cook County Medical Examiner found that, of the 44 maternal deaths resulting from trauma between 1986 and 1989, 22% were from gunshot wounds and 13.6% were from stab wounds.2 The pregnant abdomen may be the target of penetrating trauma when angry behaviors are displayed or when attempts to abort the fetus are made. The pregnancy may actually be the precipitating factor for a shooting or a stabbing.16
Pregnant women also can receive burn and inhalation injuries although these types of injuries occur less frequently than those previously mentioned. Thermal injuries during pregnancy usually occur at home or in the work environment and are caused mainly by flame or hot liquids. The incidence of thermal injuries to pregnant women is low in the Western world, but it is higher in developing countries.22
NURSING DATABASE
All female trauma patients of childbearing age should be considered pregnant until proven otherwise. Sherer and Schenker23 suggest that it is difficult to determine the actual incidence of trauma during pregnancy because of failure to question or document. They cite two clinical examples in which this information may not be recorded: the mild traumatic event that is poorly documented in the medical record and the life-threatening situation in which pregnancy may not be considered. Therefore, it is of utmost importance that an accurate database and patient health history be obtained as soon as possible. An obstetric history, starting with questions about pregnancy, should be initiated immediately. This information not only helps to establish a pregnant condition but can often provide information that aids in both the diagnosis and management of traumatic injuries during pregnancy. Because the patient may be unable to provide reliable information or may be unaware of her pregnancy status, a pregnancy test should be performed if she is of child-bearing age. A description of the events preceding an injury and, whenever possible, of the actual event itself is important to obtain, particularly when the trauma patient is pregnant. If loss of consciousness, headache, back pain, or abdominal pain precedes an incident involving a pregnant woman, an underlying obstetric etiology should be suspected.
MECHANISM OF INJURY
Motor Vehicle Crash
The information important to obtain after a pregnant woman’s involvement in a motor vehicle crash includes whether she was a driver or passenger in the vehicle, whether she was wearing a seat belt and shoulder harness, and whether the air bag deployed. The dynamics of the crash are significant (see Chapter 12) and should be considered in anticipating maternal and fetal injuries. If the woman was the driver of the vehicle, then the protuberant abdomen may have been injured by the steering column, particularly if safety restraints were not used. Proper use of seat belts may decrease the severity of maternal injuries and increase maternal survival3,24 (Figure 28-2). Seat belts prevent ejection from the vehicle, decrease the likelihood of severe head injury, and in general lower mortality rates. Because the overall leading cause of fetal death is maternal death after motor vehicle crashes, seat belts also increase the chance of fetal survival.3,25–27 After motor vehicle crashes, unbelted women have lower birth weight infants and are more likely to give birth within 48 hours.28
When prehospital care providers have information about the events that precipitated a crash or its severity, this information should be conveyed to the health care providers at the receiving facility. One study examined the relationship between type of collision and resultant maternal injuries in 441 pregnant women who were involved in motor vehicle crashes.24 When there was minor damage to the vehicle, fewer than 1% of the women were injured. When the damage to the vehicle was severe, more serious injuries were found, as expected. Seven percent of those who were involved in severe crashes died and 12.9% were injured. More recent studies have focused on maternal factors such as the ISS, Acute Physiology and Chronic Health Evaluation (APACHE) score, lactate level, maternal injury, head injury, pelvic fractures, and Kleihauer-Betke (KB) smear as predictors of fetal outcome.10,11
Intimate Partner Violence
When the patient has a pattern of injuries that does not match the reported mechanism, the nurse should suspect intimate partner violence (IPV) and administer an assessment screening to the patient in a private area separate from the mate. If IPV is suspected, the patient must receive follow-up care. To prevent future repeated IPV, the pregnant woman should be educated about safety behaviors, including hiding money, having extra keys, having a family code, and removing weapons.29 All women should be aware that the National Domestic Violence Hot Line is available to them by calling 1-800-799-SAFE or, for the hearing impaired, 1-800-787-3224. The Web site is www.NDVH.org.
In view of this strong epidemiologic basis for violence during pregnancy and the potential obstetric complications, nurses must maintain a high index of suspicion and probe to ascertain information detailing the events leading to injury. Parker and McFarlane21 suggest that routine prenatal assessment provides an excellent opportunity to conduct an abuse assessment screening. Hospitalization for an unexplained traumatic event is also a time to conduct such an assessment. As stated by Parker and McFarlane, a nonjudgmental, gentle approach is essential, but the questions must be direct. An assessment screening tool developed by the Nursing Research Consortium on Violence and Abuse is presented in Figure 28-3.
Burns and Inhalation Injuries
If the pregnant patient has a suspected inhalation injury, carbon monoxide (CO) intoxication should always be suspected and carboxyhemoglobin (COHb) levels should be measured. CO intoxication is a common cause of all poisoning deaths, including fetal poisoning deaths, in the United States.30 If the patient has been a victim of trauma associated with fire, automobile exhaust, faulty heating systems, or generator use, CO intoxication should be considered.
The fetal effects of CO poisoning are more severe than maternal effects because the concentration of COHb is 10% to 15% higher in the fetus as a result of the higher affinity of fetal hemoglobin for CO.31 Extensive research by Longo and Hill32 demonstrated that fetal COHb concentration rises more slowly than does the maternal level but surpasses maternal levels after 5 hours. Maternal CO will reach a steady state in 7 to 8 hours, but fetal concentrations continue to rise for 36 to 48 hours.32 The CO half-life in the fetus is twice as long as the maternal half-life. Therefore, the fetus is more susceptible to CO poisoning.
Fetal effects include teratogenicity, neurologic dysfunction, decreased birth weight, and increased fetal death because the fetal partial arterial oxygen concentration (PaO2) decreases in direct proportion to the increase in COHb. CO poisoning impairs the release of oxygen from the mother to the fetus and from fetal hemoglobin to fetal tissue. Prompt diagnosis and appropriate management of inhalation injuries are therefore essential.33
OBSTETRIC HISTORY
When pregnancy is suspected, an obstetric history should be considered an important component of the patient’s health history. The gestational age of the fetus and status of the pregnancy must be established, and a complete obstetric history should be obtained as soon as possible. Suspicion of pregnancy increases if more than 4 weeks have lapsed since the last menstrual period (LMP) or if the LMP was unusual in any way. To determine the gestational age, early ultrasonography is most reliable.34–36
A more thorough obstetric history includes determining parity (Table 28-1), which indicates any previous abortions or premature deliveries. The history for each delivery, including gestational age of the fetus, number of hours of labor, and type of birth (vaginal or cesarean), also should be obtained along with the maternal Rh factor. This information can alert medical personnel to potential problems, including premature labor and delivery. When possible a spouse, family member, or significant other should be interviewed to help obtain and verify this information. Information should also be obtained concerning what, if any, form of contraception was used and how assiduously it was used.
| In many institutions, obstetric history is summarized by digits and dashes (e.g., 3-1-0-4). | |
| First digit | Number of term infants (38 weeks) |
| Second digit | Number of premature infants (20-37 weeks) |
| Third digit | Number of abortions (any loss before 20 weeks, including ectopics and induced abortions) |
| Fourth digit | Number of children currently alive |
| In the example above (3-1-0-4), the woman had 3 term births and 1 premature infant and has 4 children alive. (Many recall this with the mnemonic Florida Power And Light, which stands for Full-term, Preterm, Abortions, and Living.) | |
Data from Pritchard J, MacDonald P, Gant NF: Williams’ obstetrics, 17th ed, p 246, Norwalk, CT, 1990, Appleton-Century-Crofts.
RESUSCITATION PHASE
Early signs of pregnancy may be easily overlooked. Therefore, the astute nurse is alert to even the most subtle changes that can occur during pregnancy (Table 28-2). On admission, a pregnancy test should be performed on any woman of child-bearing age. Early recognition that the trauma patient is pregnant can lead the nurse through the dual assessment of mother and fetus.
TABLE 28-2 Presumptive, Probable, and Positive Signs of Pregnancy
Data from Pilliteri A: Maternal-newborn nursing care of the growing family, 3rd ed, p 320, Boston, 1985, Little Brown.
The general principles on which trauma management is based must not be ignored in caring for a pregnant trauma patient. The implementation of a rapid primary survey followed by a secondary assessment is imperative, with airway, breathing, and circulation (the ABCs) acknowledged as first priorities.37 Early recognition of pregnancy should trigger the nurse to be suspicious of unique injuries and to be alert for the pregnancy-related changes that may alter assessment findings and mask signs of shock.
CLINICAL MANAGEMENT/TEAM APPROACH
The key to successful management of the pregnant trauma patient is a team approach. Both emergency/trauma personnel and obstetric personnel should be involved in the patient’s care.37,38 Although obstetric management is imperative, the ABCs of trauma resuscitation remain the first priority because the best guarantee of fetal survival is prompt maternal care after traumatic injury.
In 1974, Crosby39 identified complications associated with the management of injured pregnant women:
Today, more than 30 years later, the situation as Crosby describes it may not be as common in the trauma setting, but the concept of therapeutic paralysis does persist. The development and continuing provision of an Advanced Life Support in Obstetrics course for improved obstetric emergency management suggests that concerns continue about the management of obstetric emergencies.40 The fact that aggressive maternal care is essential for the best fetal outcome must be emphasized.2,41,42
MATERNAL ASSESSMENT
To render prompt and aggressive care to the pregnant trauma patient during the resuscitation phase, the nurse must have knowledge not only about initial trauma management interventions but also about the normal anatomic and physiologic changes that occur during pregnancy and the significat of these changes43,44 (Table 28-3). This knowledge must be applied during the initial assessment process and as resuscitation efforts continue.45,46 Care of the pregnant trauma patient becomes more complex when obstetric complications are encountered in addition to traumatic injuries. These assessment considerations are not limited, however, to the resuscitation phase of care; they must be considered throughout all phases of trauma care.
TABLE 28-3 Normal Anatomic and Physiologic Changes During Pregnancy
| Body System | Alteration | Significance of Change |
|---|---|---|
| Neurologic | Increased risk of fainting | More prone to fall |
| Easily fatigued | Increased risk of trauma | |
| Cardiovascular | Hypervolemic (increased volume of as much as 50% above prepregnancy levels) | Signs of blood loss can develop subtly |
| Supine hypotension | Increased fluid needs for resuscitation | |
| Physiologic anemia | Vital signs and laboratory tests must be assessed against normal pregnancy values (see Tables 28-5 and 28-6) | |
| Increased heart rate | ||
| Hypercoagulability | Increased risk for thromboembolism | |
| Respiratory | Engorged upper respiratory passages | Potential for nasopharyngeal bleeding making gentle oral intubation with smaller well-lubricated tube preferable |
| Increased tidal volume | Altered response to inhalation anesthetics | |
| Increased vital capacity | ||
| Increased respiratory rate | Decrease in blood buffering capacity | |
| Decreased functional residual capacity | Early use of oxygen therapy essential as a result of decreased functional residual capacity | |
| Elevated diaphragm | Greater risk for diaphragm rupture | |
| Gastrointestinal | Physiologic ileus | Increased risk of aspiration |
| Increased gastric acidity | ||
| Compartmentalization of abdominal contents | Altered internal injury patterns | |
| Genitourinary | Increased urinary frequency | |
| Increased glomerular filtration rate | ||
| Dilation of renal calyces, renal pelvis, and ureter | Altered appearance of IV urogram | |
| Bladder pulled into abdomen | Bladder susceptible to abdominal trauma | |
| Musculoskeletal | Alterations in gait and balance | Increased risk of fall |
| Widened symphysis pubis | Possible increased risk of spinal subluxation | |
| Lordosis |
Neurologic Considerations
Neurologically, a pregnant woman has an increased risk of fainting and is more easily fatigued.46 The pregnant woman also may have changes in gait and balance, primarily during the third trimester. Changes in vision, complaint of headaches, and seizure activity (especially in a patient with no history of seizure) are abnormal and, when present, suggest obstetric complications such as preeclampsia and eclampsia (Table 28-4). Prompt identification of an obstetric complication can guide care and decrease the incidence of both maternal and fetal compromise.
TABLE 28-4 Signs and Symptoms of Preeclampsia
| Mild Preeclampsia | Severe Preeclampsia |
|---|---|
| When any of the following exists: | |
| Systolic blood pressure of at least 140 mm Hg or a diastolic blood pressure of at least 90 mm Hg | Blood pressure >160 mm Hg systolic, >110 mm Hg diastolic |
| Seizures = eclampsia |
From American College of Obstetricians and Gynecologists: Hypertension in pregnancy, ACOG technical bulletin No. 219, Washington, DC, 1996, American College of Obstetricians and Gynecologists.
Respiratory Considerations
During pregnancy, there may be as much as a 40% increase in tidal volume and a rise of 100 to 200 ml in vital capacity. The respiratory rate may remain unchanged or increase by 15%.44 The combined effects of these respiratory changes place the pregnant woman in a chronic state of “hyperventilation” that results in arterial blood gas alterations. The partial arterial carbon dioxide (PaCO2) levels drop to approximately 30 mm Hg, and PaO2 increases to 101 to 104 mm Hg. A normal pH is maintained by the excretion of bicarbonate by the kidneys (Table 28-5).
TABLE 28-5 Laboratory Value Adjustments During Pregnancy
| Nonpregnant | Pregnant | |
|---|---|---|
| Electrolytes and Acid-Base Values | ||
| Sodium (mEq/L) | 135-145 | 132-140 |
| Potassium (mEq/L) | 3.5-5.0 | 3.5-4.5 |
| Chloride (mEq/L) | 100-106 | 90-105 |
| Bicarbonate (mEq/L) | 24-30 | 17-22 |
| Pco2 (mm Hg) | 35-50 | 25-30 |
| Po2 (mm Hg) | 98-100 | 101-104 |
| Base excess (mEq/L) | 0.7 | 3-4 |
| Arterial pH | 7.38-7.44 | 7.40-7.45 |
| BUN (mg/dl) | 10-18 | 4-12 |
| Creatinine (mg/dl) | 0.6-1.2 | 0.4-0.9 |
| Creatinine clearance (ml/min) | 3.5-5.0 | 2.0-3.7 |
| Osmolality (mOsm/kg) | 275-295 | 275-285 |
| Lipids and Liver Function Tests | ||
| Total bilirubin (mg/dl) | 1.0 | 1.0 |
| Direct bilirubin (mg/dl) | 0.4 | 0.4 |
| Alkaline phosphatase (international units/ml) | 13-35 | 25-80 |
| SGOT (international units/ml) | 10-40 | 10-40 |
| Total protein (g/dl) | 6.0-8.4 | 5.5-7.5 |
| Albumin (g/dl) | 3.5-5.0 | 3.0-4.5 |
| Globulin (g/dl) | 2.3-3.5 | 3.0-4.0 |
| Total lipids (mg/dl) | 460-1,000 | 1,040 |
| Total cholesterol (mg/dl) | 120-220 | 250 |
| Triglycerides (mg/dl) | 45-150 | 230 |
| Free fatty acid (g/L) | 770 | 1,226 |
| Phospholipids (mg/dl) | 256 | 350 |
| Hematologic Laboratory Values | ||
| Complete blood cell count: | ||
| Hematocrit (%) | 37-48 | 32-42 |
| Hemoglobin (g/dl) | 12-16 | 10-14 |
| Leukocytes (count/mm3) | 4,300-10,800 | 5,000-15,000 |
| Polymorphonuclear cells (%) | 54-62 | 60-85 |
| Lymphocytes (%) | 38-46 | 15-40 |
| Fibrinogen | 250-400 | 600 |
| Platelets | 150,000-350,000 | Normal or slightly decreased |
| Serum iron (g) | 75-150 | 65-120 |
| Iron-binding capacity (g) | 250-410 | 300-500 |
| Iron saturation (%) | 30-40 | 15-30 |
| Ferritin (ng/ml) | 35 | 10-12 |
| Erythrocyte sedimentation (mm/hr) | <20 | 30-90 |
SGOT, Aspartate aminotransferase.
Modified from Elrad H, Gleicher N: Physiologic changes in normal pregnancy. In Gleicher N, editor: Principles of medical therapy in pregnancy, pp 51-52, New York, 1985, Plenum.
As the pregnancy progresses, there is an increased minute ventilation, which is caused by a rise in tidal volume. This increased tidal volume leads to a decreased functional residual capacity (FRC) by up to 20% at times. A reduced FRC lowers the closing alveolar pressure, which predisposes the pregnant woman to alveolar collapse, atelectasis, and decreased oxygen reserve. Therefore, the airway and breathing of a pregnant trauma patient must be monitored carefully and supported as necessary to prevent maternal and subsequent fetal hypoxia. Supplemental oxygen should be given to all pregnant trauma patients, and pulse oximetry should be monitored continuously. If the patient is intubated, capnography is useful.
Cardiovascular Considerations
Cardiovascular changes are perhaps the most profound physiologic alterations that occur during pregnancy and the most critical to interpret when the pregnant trauma patient is assessed. The pregnant woman is normally hypervolemic. Blood volume during pregnancy begins to increase by the tenth week of gestation; by the thirty-fourth week of gestation, a pregnant woman’s circulatory volume can increase by as much as 50%. This increase can mask a 30% gradual loss of maternal blood volume or a 10% to 15% acute blood loss. When this occurs, although the maternal vital signs may remain unchanged, the fetus can be at risk because of a decrease in uterine perfusion; the woman’s risk is also increased because these stable vital signs may change precipitously. Because the uterus cannot autoregulate its blood flow, perfusion is directly related to the pressure it receives from maternal circulation.
The electrocardiogram can be altered during pregnancy as well. As the uterus enlarges and elevates the diaphragm, the heart is pushed upward and rotated, causing a shift of the electrical axis by 15 degrees. This may precipitate changes such as T-wave flattening or inversion in lead III; or Q waves in lead III and the augmented V lead, which are considered normal in pregnancy.47
Hematologic Considerations
Although erythrocyte production increases during pregnancy, adequate levels cannot be maintained as plasma volume increases; therefore, the pregnant woman is physiologically anemic.48 A normal prepregnancy hematocrit of 40% to 41% may drop to 31% to 34% in late pregnancy.
The coagulation profile of the pregnant woman is also altered because fibrinogen and concentrations of factors VII, VIII, and IX are increased during pregnancy. Bleeding time, clotting time, and prothrombin time should remain unchanged during pregnancy. The increase in fibrinogen and other factors, coupled with a decrease in circulating plasminogen activator, can actually benefit the pregnant patient if hemorrhage occurs. These same changes, however, pose a potential problem. The risk of venous thromboembolism is five times higher in a pregnant woman than in a nonpregnant woman of similar age. Immobility after a traumatic event puts the pregnant patient at even greater risk.46,49
The leukocyte count is normally elevated in pregnancy to approximately 5,000 to 15,000/mm3 and becomes even further elevated during labor and delivery. Except for an increase in phagocytes and a decrease in lymphocytes during pregnancy, the differential remains unchanged. Other laboratory study adjustments for pregnant women are listed in Table 28-5.
A 5-year retrospective study of trauma patients with a placental abruption found that a white blood cell (WBC) count of >20,000/mm3 on admission was strongly predictive of placental abruption (p = .005). The study also suggested that a WBC count of <20,000/mm3 rules out placental abruption (negative predictive value, 100%).50 It should be remembered, however, that abruptions are dynamic events that can evolve over time. Therefore, the nurse should remain vigilant for clinical signs such as contractions, abdominal pain, or changes in fetal status.38
Hemodynamic Considerations
The most dramatic hemodynamic change that occurs during pregnancy is supine hypotension, also known as vena cava syndrome. After 16 to 20 weeks’ gestation, when the patient assumes the supine position, the enlarging uterus compresses the vena cava and aorta, impeding venous return and decreasing blood pressure and cardiac output. Hypotension therefore can occur normally in a pregnant woman in a supine position. When this occurs, the patient becomes uncomfortable or nauseated until she is repositioned and blood pressure increases. Therefore, the pregnant trauma patient should never be placed in the supine position. Traditionally the pregnant woman is placed in the left lateral position, which displaces the uterus and decreases compression of the major abdominal vessels (Figure 28-4). During prehospital transport and until spinal injuries are ruled out, the supine position can be avoided by tilting the backboard 30 degrees to the left side, simulating the left lateral position44,45 (Figure 28-5). Turning the pregnant patient to the left lateral position can markedly increase cardiac output and should always be considered as a resuscitative measure. Care must be taken to stabilize the neck and maintain the spine in proper alignment when repositioning the patient. The right-sided tilt can be equally effective if left-sided injuries make that position difficult. If the patient’s injuries or resuscitation procedures prohibit this position change, the uterus can be displaced manually. The vital signs should be monitored closely for indications of shock throughout the resuscitation phase so that aggressive volume replacement can be initiated as necessary.
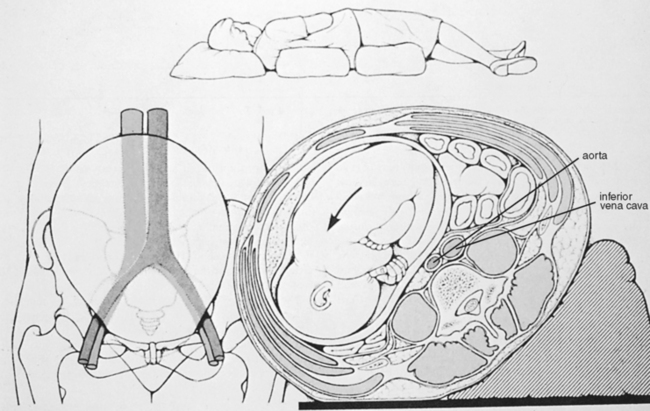
FIGURE 28-4 Left lateral positioning displaces the uterus and decreases compression of major abdominal vessels.
Hypertension is not normal during pregnancy; it should be resolved as to whether the hypertension existed before pregnancy or is indicative of pregnancy-induced hypertension. During pregnancy, the heart rate increases approximately 10 to 20 beats/min above prepregnancy levels. Clark et al51 assessed the central hemodynamic status of ten healthy pregnant patients who were screened carefully both in the third trimester and post partum. In late pregnancy, the patients had a 43% increase in cardiac output (4.3 to 6.2 L/min). Other significant findings included a 21% decline in systemic vascular resistance, a 34% reduction in pulmonary vascular resistance, and a 28% decrease in the colloid oncotic pressure-pulmonary capillary wedge pressure gradient. There was no significant difference in mean arterial pressure, central venous pressure, or pulmonary capillary wedge pressure during late pregnancy compared with the nonpregnant state (Table 28-6).
TABLE 28-6 Central Hemodynamic Changes
| Nonpregnant | Pregnant | |
|---|---|---|
| Cardiac output (L/min) | 4.3 ± 0.9 | 6.2 ± 1.0 |
| Heart rate (beats/min) | 71 ± 10.0 | 83 ± 10.0 |
| Systemic vascular resistance (dyne cm sec−5) | 1530 ± 520 | 1210 ± 266 |
| Pulmonary vascular resistance (dyne cm sec−5) | 119 ± 47.0 | 78 ± 22 |
| Colloid oncotic pressure (mm Hg) | 20.8 ± 1.0 | 18.0 ± 1.5 |
| Colloid oncotic pressure–pulmonary capillary wedge pressure (mm Hg) | 14.5 ± 2.5 | 10.5 ± 2.7 |
| Mean arterial pressure (mm Hg) | 86.4 ± 7.5 | 90.3 ± 5.8 |
| Pulmonary capillary wedge pressure (mm Hg) | 6.3 ± 2.1 | 7.5 ± 1.8 |
| Central venous pressure (mm Hg) | 3.7 ± 2.6 | 3.6 ± 2.5 |
| Left ventricular stroke work index (g-m/m−2) | 41 ± 8 | 48 ± 6 |
From Clark S, Cotton O, Lee W et al: Central hemodynamic assessment of normal term pregnancy, Am J Obstet Gynecol 161:1439-1442, 1989.
The hemodynamic changes that occur normally during pregnancy can cause confusion as the resuscitation team assesses the patient’s condition. Tachycardia and hypotension that occur when the pregnant trauma patient is in a supine position may not be indicative of a shock state but may instead represent normal changes. Caution must be exercised, however, because the pregnant trauma patient, as previously stated, can mask a 15% to 30% blood loss without evidence of shock while uterine perfusion decreases, risking fetal hypoxia. Changes in laboratory values, including decreased hematocrit and increased leukocyte count, further confuse the clinical picture. Laboratory value trends must be monitored closely as well and compared with normal pregnancy values (see Table 28-5).
Gastrointestinal Considerations
Injuries to the liver and spleen commonly cause shock during pregnancy. The patient’s abdomen should be assessed carefully for pain, guarding, and rebound tenderness. If clinically indicated, an orogastric tube may be inserted early during the resuscitation phase of care. The patient should be prepared for abdominal tests to detect injury and the source of hemorrhage. She may perceive the procedure as harmful to her baby and should be encouraged to verbalize her fears. Reinforcing the value of the procedure as a diagnostic tool that is not harmful to the baby may ease some of the mother’s fears.52 Preparation for surgical intervention is indicated if abdominal exploration is deemed necessary.
Genitourinary Considerations
Genitourinary changes include an increase in urination frequency throughout pregnancy. The increase in frequency during the first trimester is the result of a rise in the glomerular filtration rate (GFR) by approximately 30% of prepregnancy values.53 During the third trimester the further increased frequency is a result of compression of the bladder by the enlarging uterus, in addition to an increased GFR.
With blunt trauma to the abdomen during late pregnancy, the bladder is more likely to empty spontaneously or rupture because the bladder may be elevated and outside the protective pelvic ring. If a stable condition allows, the patient should be encouraged to void. If she is unable to void spontaneously and bladder trauma is plausible given the mechanism of injury, the patient should be catheterized by use of strict aseptic technique. Glucosuria is common during pregnancy, but the presence of frank or microscopic blood suggests genitourinary trauma. Diagnostic tests may be performed, including cystography, intravenous (IV) pyelography, and cystoscopy. Physiologic dilation of the renal calyces, renal pelves, and ureters (particularly on the right side) may be evident. These conditions are present from approximately the tenth week of pregnancy until after delivery and are believed to be caused by ureteral obstruction from the ovarian vein plexuses, dextrotorsion of the uterus, and increased progesterone concentrations.53
Metabolic Considerations
As a normal change of pregnancy, the pituitary gland nearly doubles in weight. Shock in the pregnant patient can precipitate a sudden drop in pituitary blood flow, leading to necrosis54 (known as Sheehan’s syndrome). During pregnancy, calcium, phosphate, magnesium, creatinine, and blood urea nitrogen (BUN) levels fall. There is also an increased risk of glucose intolerance.
OBSTETRIC AND FETAL CONSIDERATIONS
Obstetric Assessment
Gestational Age.
Accurate assessment of gestational age or the estimated date of delivery (EDD) is important during the initial resuscitation to determine whether the fetus is viable. An ultrasonography performed in the first trimester of pregnancy provides the most accurate estimate of gestational age.34–36 An ultrasonographic scan performed at weeks 6 to 11 of a pregnancy is accurate within 5 to 7 days and when performed in the twelfth to twentieth week of pregnancy is accurate within 10 days.55 Many times information from previous scans may not be available. However, if the patient or a reliable historian is available, the EDD from an early ultrasonographic scan can provide a means of calculating gestational age. Barring this, ultrasonography performed in the emergency setting will give a reasonable means of assessing gestational age and has become a routine assessment tool for obstetricians, trauma surgeons, and emergency physicians.45,46,56,57
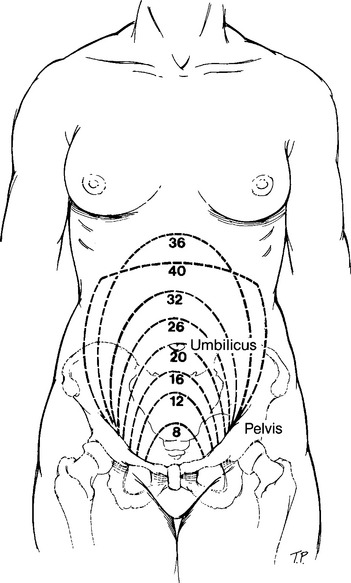
For a rapid assessment (including prehospital assessment), fundal height provides another means of estimating gestational age. This technique may be subject to several misleading variables such as aminotic fluid level, obesity, and macrosomia. Fundal height is the distance from the symphysis pubis to the top of the fundus. From 16 to 32 weeks, this measurement approximates the weeks of gestation (Figure 28-6).
Determination of the gestational age of the fetus is also helpful in identifying possible injuries to both the mother and fetus. During the first 12 to 14 weeks (early pregnancy), the uterus is well protected in the pelvic confines. Cases of uterine and fetal injury during this period have been documented, but they are rare. After the first trimester (12 to 14 weeks), the uterus becomes an abdominal organ and is no longer protected by the pelvis. The uterus and fetus may therefore absorb the impact of traumatic forces and consequently sustain unique injuries.
Fetal Assessment
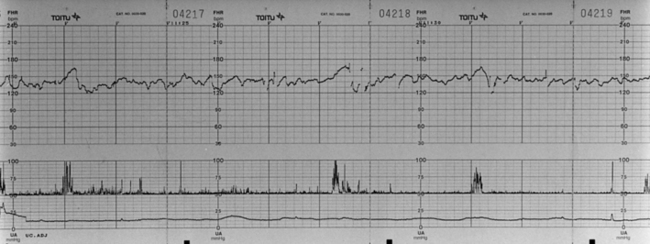
Continuous fetal assessment is essential because the mother can mask signs of shock and the fetus can be the first to show evidence of compromise. The fetal condition is easiest to evaluate by assessing the fetal heart rate. The normal fetal heart rate is 120 to 160 beats/min and can be detected with an ultrasound device (Doppler) by 10 to 12 weeks of gestation. If the fetus is viable, its heart rate should be monitored continuously with an electronic fetal monitor (EFM) once the mother’s condition has been stabilized. The variability of the fetal heart tones (FHT) and the rate should be evaluated by a clinician experienced in fetal monitoring (see Figure 28-7). Fetuses that are 24 weeks or older are considered viable if neonatal resources are available. If an EFM is not available, only a Doppler device designed for obstetric evaluation should be used because its frequency is adjusted to assess FHTs. A Doppler device of higher frequency used for adults, such as those used for vascular studies, may not have sufficient range so that nothing is heard although the fetus is viable, thereby confusing the clinical picture. In many instances, fetal compromise as suggested by prolonged fetal bradycardia may be reflective of fetal hypoxemia. If the mother is stable and the fetus considered viable, immediate delivery should be considered on behalf of the fetus.
The length of time a pregnant patient requires electronic fetal monitoring has been debated. Recent studies suggest that within 4 to 6 hours of minor trauma, if there is no labor or fetal distress, monitoring can be safely discontinued.10,58,59 It is fairly clear that in patients who do not have contractions and who have good variability in FHTs the need for additional monitoring is slight. Patients having contractions clearly require additional monitoring. Once the decision has been made to continue obstetric monitoring, the collaborative team of trauma and obstetric professionals must identify the appropriate nursing unit in which the patient will receive care and diligent fetal monitoring.
Additional diagnostic procedures that can aid in assessing the condition of the fetus include ultrasonography and amniocentesis. Real-time ultrasonography can identify fetal cardiac movement, detect FHTs, and determine fetal death. Fetal biophysical assessment by ultrasound is a method used to aid in determining and quantifying the fetal status. Fetal biophysical profile scoring (BPS) is based on five biophysical variables, four of which are monitored simultaneously by dynamic ultrasound imaging. The variables are fetal breathing movement, gross body movement, fetal tone, qualitative amniotic fluid volume, and reactive fetal heart rate.60 The fifth parameter of the BPS is a fetal heart rate tracing, which is “scored” as reactive or nonreactive. Each parameter is coded as present or absent according to set criteria and given a rating of 2 (present) or 0 (absent) with a maximum score of 10.
On the basis of the BPS, a management protocol is recommended.61 A biophysical score of 2 out of 10 can be indicative of severe fetal compromise, including asphyxia. However, in the acute setting the impact of medications such as narcotics, sedatives, or anesthetics must be considered when score results are analyzed. In the emergency setting, biophysical profile scoring may be helpful, but the test may require up to a 30-minute ultrasound observation period, which may not be appropriate during initial trauma resuscitation. The scoring and observation can be done after maternal resuscitation.
Amniocentesis can test for fetal maturity. Maturity of the fetal lungs is determined by the lecithin/sphingomyelin ratio and the presence of phosphatidyl glycerol in the amniotic fluid. It is difficult to imagine, however, how this information would be obtained and used in an acute care setting. If it is important to consider an early delivery, gestational age assessment, as outlined above, provides sufficient knowledge about the risks of prematurity and associated morbidity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree