21 MAXILLOFACIAL TRAUMA
INTRODUCTION
The treatment of maxillofacial trauma is one of the oldest healing arts. In Hippocrates’ time, skin grafts were used for facial reconstruction. The nineteenth and twentieth centuries saw major research-and-development breakthroughs in the diagnosis and treatment of facial trauma.1 Effective management of maxillofacial injuries remains complex and challenges virtually every member of the multidisciplinary health care team. Management of these injuries requires a profound appreciation of the functional components of the orbit, nose, and oral cavity, as well as of the subtle interrelationships between skeletal and soft tissue components that define the individual’s physical identity. The patient with facial injuries in conjunction with multisystem injuries requires integrated and coordinated assessment and management by multiple health care team members.
ETIOLOGY AND MECHANISM OF INJURY
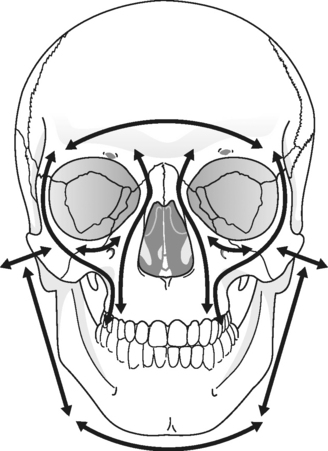
Despite mandatory seatbelt laws, lower speed limits, and airbag systems, the incidence of facial injuries remains high following motor vehicle crashes due to the fact that the face is exposed and vulnerable to forces associated with rapid deceleration.2,3 The magnitude of maxillofacial injury is directly proportionate to the velocity at impact when the face makes contact with an object. In low and mid-velocity mechanisms of injury, such as assaults, athletic incidences, falls, and low-speed motor vehicle crashes, the source of injury is usually a single-vector force and the injuries are minor, limited to soft tissue contusions, abrasions, and lacerations. However, as the velocity of single-vector injuries increases, there is greater dissipation of energy along with increased soft tissue disruption, and the underlying bone structures begin to fracture along predictable fault lines, as described by Le Fort4 (Figures 21-1 and 21-2).
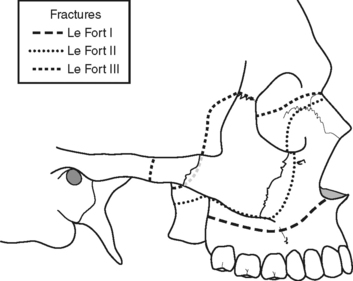
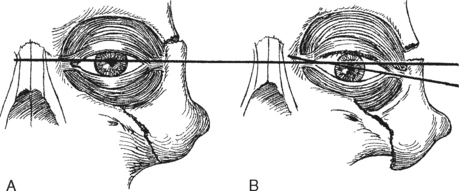
FIGURE 21-1 .Le Fort lines of fracture.
(From Cohen SR: Craniofacial trauma. In Ruberg RL, Smith DJ [eds]: A Core Curriculum Plastic Surgery, St. Louis, 1994, Mosby-Yearbook, p. 323.)
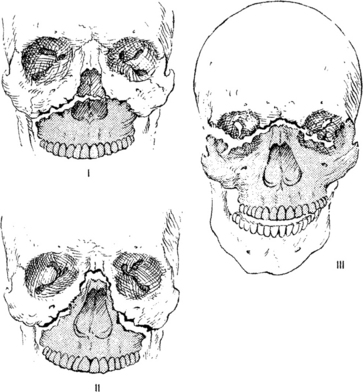
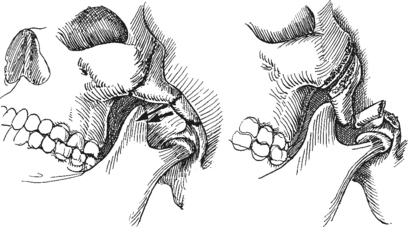
FIGURE 21-2 .Le Fort classification of maxillary fractures.
(From Schultz RC: Maxillofacial injuries. In Barrett BM [ed]: Patient Care in Plastic Surgery, ed 2, St. Louis, 1996, Mosby-Yearbook, p. 319.)
Less common facial injuries are penetrating wounds that may result from shootings or avulsions caused by high-speed motorcycle crashes. These represent a unique subset of injuries that do not follow Le Fort’s pattern of fractures and have a high potential for tissue devascularization and progressive necrosis. Patients with these injuries frequently require multiple surgeries during the early phase of hospitalization to debride necrotic tissues, followed by bone and soft tissue reconstruction performed before infection and wound contracture develop.5,6
ASSESSMENT OF MAXILLOFACIAL INJURIES WITH CORRELATIVE FACIAL ANATOMY
Comprehensive management evolves from an initial, thorough clinical examination, which then directs further diagnostic studies and culminates with development of a multidisciplinary plan of care for the patient. Maxillofacial injuries can be horrific; however, these injuries must not distract the trauma team from first stabilizing the patient’s airway, breathing, and circulation. Only then will the health care provider complete a thorough maxillofacial evaluation as well as a comprehensive assessment of other body systems to rule out associated injuries.7,8 Comprehensive maxillofacial evaluation starts with a thorough assessment of soft tissue injury followed by examination of the underlying bony elements and evaluation of possible functional disruption. Knowledge of the anatomic location and function of maxillofacial structures provides rationale for strategies used to assess facial injuries and allows appropriate interpretation of assessment findings.
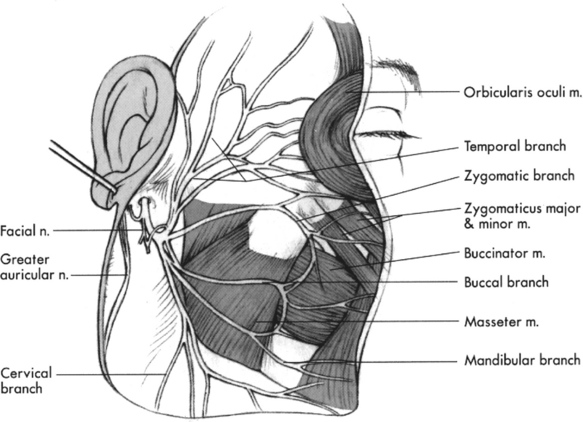
A generalized inspection for contusions, abrasions, and disruptive lacerations provides cues to direct a more thorough assessment of the underlying bony skeleton and functional elements. The ear canal, nose, oral cavity, and pharynx should be thoroughly assessed to identify any occult lacerations. An intraoral examination should account for all teeth and consider the possibility that a tooth is displaced into the alveolar bone (intrusion) or dislodged into the respiratory tract.9 A seemingly simple abrasion and laceration of the lateral cheek from a low-impact injury may have penetrated deep to injure the parotid gland and its duct, or may have injured the facial nerve, affecting facial animation10 (Figure 21-3). A spectacle hematoma of the orbit is indicative of an anterior cranial base fracture with bleeding into the intracoronal fat compartment of the orbit and mandates a thorough and serial assessment of both ocular and neurological function.
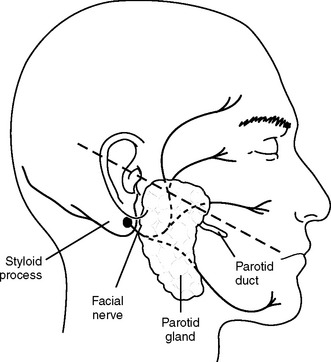
FIGURE 21-3 .Lateral cheek injury and topical landmarks for localizing the parotid gland and duct and the facial nerve.
Facial bones are relatively thin and arranged to allow deformation and displacement away from the associated functional elements of the orbit, airway, and brain. Surrounding each of the craniofacial functional units are dense bony struts organized in a system of vertical, transverse, and horizontal buttresses (Figure 21-4). These buttresses determine the three-dimensional structure of the face and act as energy-absorbing shields around the vital craniofacial structures. When the transmitted energy exceeds the absorptive capacity of these buttresses, facial fractures occur. As Le Fort described in the early 1900s, this excess force results in predictable fractures at the junction of one buttress system with another.4
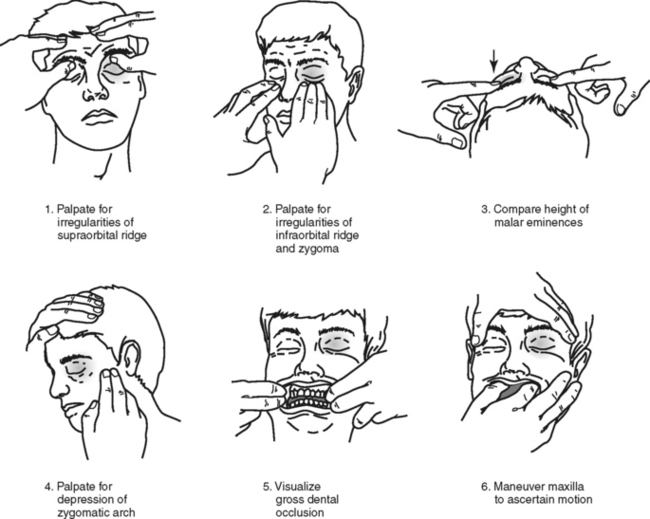
Skeletal structures should be inspected for symmetry, irregularity of bone continuity, and functional imbalance. Palpation should also be performed to identify the abnormal presence of crepitus, tenderness, or bony irregularity. Clinical evaluation techniques are shown in Figure 21-5.
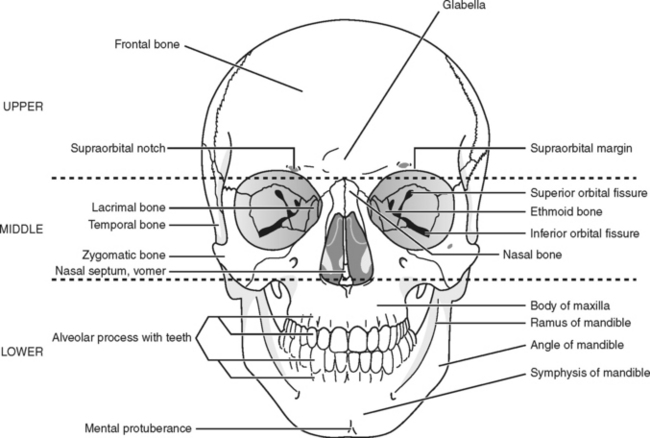
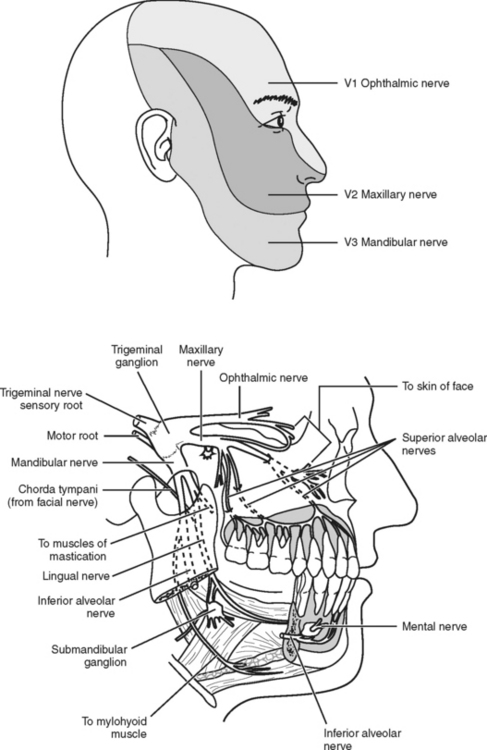
Functionally, the face is most easily divided into thirds (Figure 21-6).11 The upper third of the face includes the lower portion of the frontal bone, supraorbital ridge, nasal glabellar region, and frontal sinus. In this region, the frontal sinus, being an air cell with thin surrounding bone, is most vulnerable to injury and is referred to as a “crumple zone.”12 Fractures typically pass through its anatomic boundary. As a result, most patients present with epistaxis, absent or abnormal smell, and possible cerebral spinal fluid (CSF) drainage from the nose (rhinorrhea). If the fracture communicates more laterally through the supraorbital ridge, the patient may have decreased sensation in the upper face/forehead region, resulting from disruption of the trigeminal nerve branch (V1) innervating this area10 (Figure 21-7). If the supraorbital ridge is depressed, this fragment may impinge on the orbit, causing inferior displacement (vertical dystopia) and double vision (diplopia). A severe fracture of the orbital roof may communicate posteriorly with the superior orbital fissure (fissure between the greater and lesser sphenoid wings through which branches of cranial nerves III, IV, V, and VI traverse to the orbit), producing an associated superior orbital fissure syndrome (SOFS). Patients with this syndrome present with absent V1 sensation, pupillary fixation and dilation, loss of extraocular eye muscle movement, a down-and-out positioning of the eye, and upper eyelid ptosis (drooping).13,14 Finally, patients with injuries of this region often have associated injuries of the intracranial vault and an abnormal neurological assessment. Any abnormal neurological assessment mandates a complete neurosurgery consultation.
The middle facial third (midface) includes the orbits, maxillary sinuses, nose, zygoma bones, and basal bone of the maxilla. In this region, from a functional standpoint, fractures involve the orbit, nose, or both. The nasal bones are the most prominent structures of the midface, and therefore are the facial bones most commonly fractured. They constitute the third most commonly fractured bones in the body. Clinically, a nasal fracture presents with contour deformity and deviation, epistaxis, subcutaneous emphysema, airway obstruction, and absent or abnormal smell. In all instances, the nasal septum should be examined to rule out the presence of a nasal septal hematoma. A nasal septal hematoma must be evacuated to prevent avascular necrosis of the nasal septum and subsequent saddle-nose deformity (nasal bridge is significantly depressed) or septal perforation.15 Sense of smell provided by the olfactory nerve (cranial nerve I) is evaluated simply by determining if the patient can smell an alcohol wipe held approximately 8 inches from the nares.
In his classic paper, Le Fort described three basic patterns of midface maxillary fractures, each of which has unique clinical findings4 (Figures 21-1 and 21-2). A Le Fort I fracture is the transverse disarticulation of the maxillary dentoalveolar process from the remaining basal bone of the maxilla and midface. Clinically, this fracture presents with mobility of the maxillary dentition, but stability of the nose, orbit, and midface. A Le Fort II fracture is a pyramidal fracture involving the entire maxilla and nasal complex. Clinically, this fracture presents with unified mobility of the maxillary teeth along with the nose, but stability of the orbit and remaining midface. A Le Fort III fracture is a complete craniofacial-midface disassociation. Here there is unified mobility of the maxillary dentition, nose, and orbits. Other subtle clinical findings with a fracture of midface structures include an alteration of the horizontal orbital plane resulting from downward displacement of the zygoma or contour deformity of the malar eminence and nasal bony pyramid.
Most remaining midfacial fractures communicate through the orbit; therefore, a complete ocular assessment is mandatory. The eyes are assessed for obvious signs of trauma, such as conjunctival hemorrhage or ruptured globe. Vision and visual acuity should be evaluated. Movement of the eyes through the fields of gaze evaluates the ability of the extraocular muscles to move the eyes freely and the integrity of cranial nerves III, IV, and VI, which innervate the extraocular muscles. The patient should be observed closely for conjugate gaze in the horizontal, vertical, and sagittal eye positions. Impaired eye movement may result from edema restricting ocular movement; hemorrhage; direct injury to cranial nerves III, IV, or VI; contusion of the extraocular muscles, or an orbital fracture that causes extraocular muscle entrapment. Diplopia may result from dysconjugate gaze.16
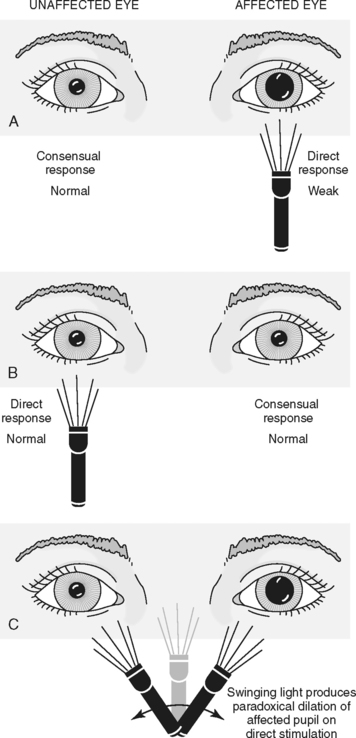
All patients with facial fractures, in particular those with periorbital ecchymosis, should have frequent assessment of the pupillary response to light. Assessment of the pupillary light reflex evaluates cranial nerve II (optic nerve), which enables the patient to perceive incoming light stimuli, and cranial nerve III (oculomotor nerve), which causes the pupil to constrict in response to the light stimulus. The Marcus-Gunn pupil test (swinging light test) should be performed on all patients17(Figure 21-8). When the healthy eye is illuminated with a bright light, the pupils constrict bilaterally; however, when the light is moved quickly to the diseased eye, the pupil dilates. This test can be performed even in the unconscious patient and is the single most sensitive test for injury of the visual track between the retina and optic chiasm.17 An ophthalmology consult is indicated whenever ocular injury is suspected by evidence of diplopia, restricted eye movement, altered forehead (V1) or cheek (V2) sensation, hyphema (anterior chamber ocular hemorrhage), ptosis, or periocular fractures.17,18 In a retrospective case review Cook found that of 365 patients with orbital fractures examined by an ophthalmologist, 22% also had ocular injuries and 24% of these patients required immediate interventions to prevent further ocular damage.18 Any abnormality in the visual assessment should be regarded as emergent and warrants an immediate ophthalmology consult.16
The lower third of the face includes the maxillary and mandibular teeth-bearing bone and the basal bone of the mandible. The posterior/superior aspect of the mandible includes the temporomandibular joint and its associated condyle and meniscus. The position of the mandible and its functional relationship with the maxilla are directed by the muscles of mastication as they function through the temporomandibular joint. Therefore, a functional assessment of the lower facial structures involves an evaluation of the muscles of mastication and their movement of the mandible through the temporomandibular joint. The patient should be asked to open and close the mandible and move it in all directions. Any fracture of the mandible or maxilla will upset the balance of this musculoskeletal system and manifest with muscular pain, splinting, and an altered bite (malocclusion). An altered bite is often subtle and perceived only by the patient; nonetheless, any objective or subjective irregularity of the bite is always abnormal and should alert the practitioner that the maxilla, mandible, or both have been fractured.19
Other subtle clinical findings associated with facial fractures in any of the three facial regions include altered facial sensation and/or motor function. Facial sensation should be assessed over the areas of distribution for each of the three branches of the trigeminal nerve (cranial nerve V) (Figure 21-7). The ophthalmic or V1 division innervates the upper face; the maxillary or V2 division innervates the midface; and the mandibular or V3 division provides sensation to the lower face. Abnormal sensation in any one of these regions may indicate an associated fracture coursing through the cranial nerve skeletal foramen. In addition to supraorbital ridge fractures, which can alter V1 sensation, orbital floor, zygoma, and Le Fort II fractures typically are associated with altered V2 sensation, and a mandible fracture may manifest with diminished V3 sensation.
Any abnormality of facial animation indicates injury to the facial nerve (cranial nerve VII), which innervates the muscles of facial expression and conveys taste for the anterior two thirds of the tongue (Figure 21-9). Facial movement can be assessed by having the patient puff out his or her cheeks, smile, show the teeth, frown, raise the eyebrows, and tightly close the eyes. In the absence of a direct laceration to one of the branches of the facial nerve, a thorough neurologic evaluation should be performed to further evaluate for possible traumatic brain injury.7 If only the lower portion of the face is paretic and the upper face is spared, an upper motor neuron lesion involving the central nervous system should be suspected. If the entire half of the face is paretic, a peripheral nerve injury involving the facial nerve is indicated.19 When the injury is believed to be proximal to the mastoid foramen, a neurosurgery consult should be obtained in conjunction with a temporal bone and intracranial computed tomography (CT) scan. Even in the comatose patient, the motor function of the facial nerve and the sensory function of the trigeminal nerve can be assessed by testing the corneal reflex. Normally, light touch with a wisp of cotton on the cornea stimulates the trigeminal nerve, which triggers the facial nerve to cause the eye to blink.
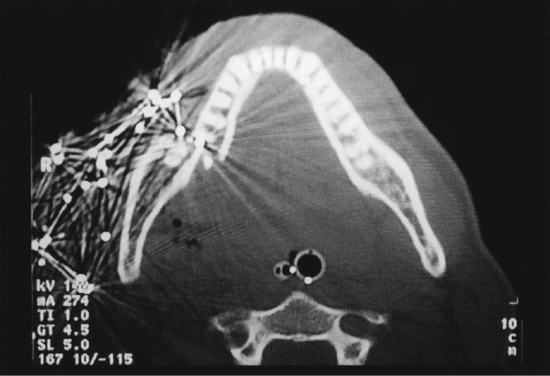
Comprehensive assessment then directs specific radiological examination. A detailed discussion of the indications for specific radiographs is beyond this review, but in general, the most effective method for a quick and thorough radiographic assessment of the maxillofacial structures is axial and coronal CT. The advantages of CT assessment over plain radiographs is the ability to evaluate more accurately the complexity of maxillofacial fractures, their comminuted parts, and the relationship of the fractures with the surrounding soft tissue12 (Figure 21-10). In the absence of obtaining true coronal CT scans, a reconstructed version can be substituted.
Twelve percent of trauma patients requiring head CTs have some type of facial fracture.20,21 Soft tissue injuries of the face can act as markers to aid clinicians in deciding if a diagnostic study should be performed to assess for facial injuries. Holmgren and Dierks propose that the acronym LIPS-N (Lip laceration, Intraoral laceration, Periorbital contusion, Subconjunctival hemorrhage, and Nasal laceration) be used during physical examination of trauma patients to indicate assessment findings that should prompt the practitioner to obtain a CT scan of the face in addition to a brain CT scan.21
SPECIFIC TYPES OF MAXILLOFACIAL INJURIES
SOFT TISSUE WOUNDS
All open facial soft tissue wounds have the potential for contamination; therefore, the patient’s tetanus immunization status should be verified. If a patient has not been immunized, it is recommended that 250 units of tetanus immune globulin (Hyper-Tet) be administered and, with a different syringe at a different intramuscular injection site, 0.5 ml of tetanus toxoid be given. Two additional tetanus toxoid boosters should be given at 1 and 12 months after the initial dose to complete the immunization. In general, tetanus toxoid is given to individuals who have been immunized previously to ensure sufficient immunization.22,23
Contusions, abrasions, and lacerations are usually not life threatening, and the timing of their treatment depends on the patient’s status and the ability to establish a surgically clean wound. Tissue that is obviously contaminated and crushed is susceptible to infection and should be excised, followed by delayed primary closure or primary repair with serial reexamination (“second-look procedure”). Multiple second-look procedures may be required every 24 to 36 hours for further debridement of progressive necrosis. This latter form of soft tissue management is most common for facial gunshot wounds and massive avulsive injuries.24
Rapid-absorbing gut suture, octylcyanoacrylate Dermabond, or nylon suture may be used for closure of facial lacerations. A comparison study of these three materials for the treatment of facial lacerations failed to show any clinically significant differences in the patient’s cosmetic outcomes at 9 and 12 months.25 Rapid-absorbing gut-suture or octylcyanoacrylate Dermabond may be preferred to eliminate follow-up visits solely for suture removal.
All wounds should be examined carefully for the presence of foreign material. The presence of foreign material increases the likelihood of infection. Meticulous hemostasis will reduce the potential for hematoma formation (a perfect medium for bacterial growth) and hence reduce the potential for infection. The use of drains may be indicated in lacerations of the parotid gland or in extensive injuries in which fluid may accumulate and produce a dead space, which fosters bacterial colonization and potentiates infection.19
More complex soft tissue injury may require skin grafts or local or remote tissue flaps. The reader is referred to Chapter 16 for more in-depth discussion about soft tissue injury.
NASAL FRACTURES
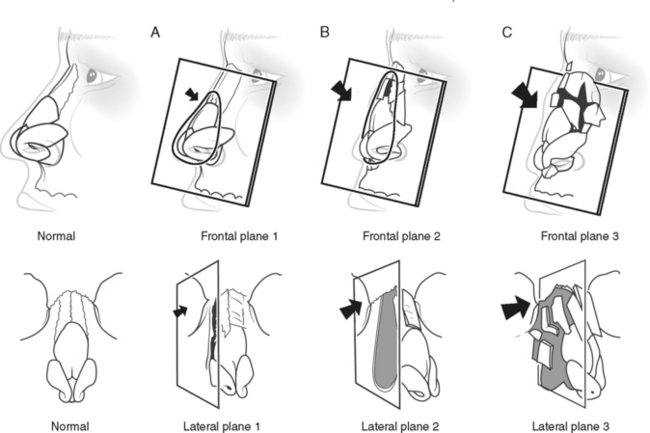
Stranc and Robertson classified nasal fractures according to their anteroposterior displacement and lateral deviation (Figure 21-11).26 In this classification, a plane 1 nasal fracture involves only the end of the nasal bony pyramid, and there is little deformity. This type of nasal fracture usually can be managed with internal reduction and nasal packing. A plane 2 nasal fracture is more extensive, involving the base of the nasal bony pyramid and nasal septum. Typically, patients with this type of injury present with a flattened nasal dorsum, obstruction of the nasal passage, and absence of smell. Treatment may require, in addition to internal reduction, some degree of external splinting and bone grafting. A plane 3 nasal fracture is in reality a nasoethmoidal-orbital fracture. This type of fracture commonly requires wide clinical exposure, bone graft reconstruction, and internal fixation techniques.
ZYGOMA AND ORBITAL FRACTURES
The zygoma is a major buttress of the midface, and its eminence gives prominence to the cheek. Additionally, it forms the lateral portion of the orbit. The zygoma is the second most frequently fractured bone in the craniofacial skeleton.4,7 Almost all fractures of the zygoma involve the orbital floor and the V2 division of the trigeminal nerve. Clinically, patients with this type of injury often have an abnormal ocular examination with periorbital ecchymosis, double vision (diplopia), and ocular proptosis secondary to edema. With extreme comminuted fractures, there may be acute enophthalmos (ocular recession within the orbit) secondary to severe loss of skeletal support. The eyes should be assessed for restriction of extraocular eye muscle movement. If there is restriction in any visual field, one must assume there is bony entrapment of the muscle requiring decompression as soon as possible.27 Additional findings specific for zygomatic fractures are depression of the malar eminence and zygomatic arch (see Figure 21-5) and downward displacement of the lateral canthus. In most instances, the zygoma is depressed and displaced downward; hence, the lateral canthus of the eye follows with the lateral orbital rim (Figure 21-12). Occasionally, the zygomatic arch can be displaced inward and impinge upon the mandibular coronoid process, thereby creating a mechanical block to mandibular opening (Figure 21-13).
Surgical management of zygomatic and orbital floor fractures is directed by the presence of functional ocular impairment (e.g., reduced eye movement caused by entrapment of extraocular muscle, diplopia, enophthalmos), depressed zygoma with deformity, altered V2 sensation, and impingement on maxillary and mandibular musculoskeletal function. The primary goal of treating the orbital floor component is to decompress any entrapped ocular tissue and simultaneously restore proper orbital volume to minimize the potential for secondary diplopia and enophthalmos.28 With respect to the zygoma itself, the goal is to anatomically reposition the zygoma for proper facial midface projection and width dimension (Figure 21-14). For accurate anatomic reduction and stabilization of the quadrangular zygoma bone, three points of fixation typically are required: the frontozygomatic buttress, infraorbital rim, and zygomaticomaxillary buttress (Figure 21-15). Access to these buttresses can be obtained through a lower eyelid incision and an intraoral maxillary buccal sulcus incision. Severe high-velocity comminuted zygomatic fractures may also require a posterior approach to reconstruct the zygomatic arch.29 The orbital floor component is explored and reconstructed through the eyelid incision using an alloplastic implant.27
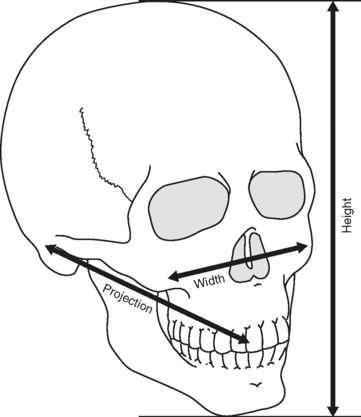
FIGURE 21-14 .The goal in midface fracture repair is to reestablish normal facial width, height, and projection.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree