Fig. 5.1
The periphery of the TFCC is well vascularized, and thus capable of healing. The central disc is avascular and thus has poor healing potential. (Courtesy of Michael Bednar, MD)
Type 1B tears involve avulsion of the TFCC from the ulnar fovea or an avulsion fracture through the base of the ulnar styloid, and the fibrocartilaginous disc may also be torn from the dorsal wrist capsule. DRUJ instability is often, but not always, associated. Tears in which the disc pulls away from the ulnar capsule with intact deep insertional fibers to the ulna are seen with ulnar sided wrist pain in the absence of DRUJ instability [15]. As 1B tears are through the vascularized periphery and may heal, surgical repair is preferred either directly to bone or to the ulnar capsule depending on whether DRUJ instability is or is not present respectively [15–20]. Type 1C tears occur along the volar margin and are associated with disruption of the ulnolunate, ulnotriquetral, or ulnocapitate ligaments of the wrist. These are typically high-energy injuries, often associated with ulnocarpal instability and volar translation of the ulnar carpus. Open repair is the most common surgical treatment to restore stability [21]. Type 1D lesions result from detachment of the TFCC from the ulnar radius, either via rupture of the radioulnar ligaments or an avulsion fracture of the radius at the sigmoid notch. If the radius and radioulnar ligaments are intact, the lesion is treated as a Type 1A tear and can be debrided [9, 22]. If DRUJ instability is present or the origin of one or more radioulnar ligaments disrupted, repair is preferred [23–25].
Type II lesions represent degeneration of the TFCC and surrounding structures due to chronic ulnar positive variance and consequent ulnocarpal impaction syndrome. Even small changes in ulnar variance can dramatically affect load-sharing, with 2.5 mm of ulnar positivity causing 42 % of load to be borne through the ulnocarpal joint vs. 18 % in an ulnar-neutral wrist [26]. In contrast to Type I tears, which represent distinct traumatic injuries, Type II lesions represent a spectrum of progressive pathology. Type 2A lesions involve wear of the proximal side of the TFCC only, without perforation or associated pathology. Type 2B lesions demonstrate the same degree of TFCC wear but in association with chondromalacia of the lunate or ulnar head. Type 2C lesions involve a perforation of the fibrocarilaginous disc, but unlike Type 1A tears they are typically ovoid in shape and more ulnar within the substance of the disc. Type 2D lesions involve both the TFCC perforations, lunate and ulnar head chondromalacia, and lunotriquetral ligament disruption. Finally, Type 2E lesions show frank degenerative arthritis of the ulnocarpal joint, lunotriquetral ligament disruption, and may also be associated with ulnar lunate collapse or DRUJ arthritis [1, 27]. Treatment for Type II TFCC lesions centers around correcting positive ulnar variance, with ulnar shortening osteotomy or arthroscopic debridement and ulna wafer resection being the most common treatments [28, 29]. For advanced pathology or failed primary surgery, either a distal ulna resection or Sauve-Kapandji procedure along with lunotriquetral pinning may be necessary.
Imaging
Standard posterior–anterior (PA), lateral, and oblique radiographs are the first-line imaging study to assess the TFCC, DRUJ, and wrist joint. Acute injury to the TFCC can be inferred by examining the integrity and alignment of the distal radius and ulna relative to the carpal bones. Widening of the DRUJ on a PA radiograph or anterior/posterior displacement of the ulna on a lateral radiograph suggests injury and instability; however, given anatomic variability it is important to compare to the unaffected extremity. Soft tissue Type 1B, 1C, and 1D injuries may still be associated with instability, however, and the presence of normal radiographs cannot exclude injury [30]. Ulnar variance should also be assessed on radiographs, including a power-grip PA in pronation if dynamic ulnocarpal impaction is suspected. Computed tomography (CT) can also be used to further clarify bony anatomy, and can compare DRUJ alignment side to side in positions of neutral, supination, and pronation to help detect subtle instability. CT scan is also more sensitive for detecting degenerative change within the DRUJ, distal ulna, or carpus associated with chronic pathology [8].
Magnetic resonance imaging (MRI) and arthrography (MRA) have largely replaced traditional arthrography as imaging modalities of choice, given the poor correlation of traditional arthrography with arthroscopic findings [31, 32]. To improve diagnostic accuracy, MRI should ideally be performed with the use of a microscopy wrist coil and at least a 1.5-T magnet [33]; newer 3.0-T magnets are significantly more accurate at imaging the TFCC, but are also more costly and less widely available [34]. Golimbu has also recommended imaging with 3 mm-thick sections and with the wrist in radial deviation to stretch ulnar tissues as techniques to improve accuracy, but no comparative studies have been performed regarding the effect of wrist position [35]. Systematic review of MRA vs. MRI by Smith demonstrated MRA to be superior to MRI for the detection of TFCC pathology, with pooled sensitivity of 84 % and specificity of 95 % for MRA vs. 75 and 81 % for noncontrast MRI [36]. Given these findings, they concluded that MRA should be the study of choice for evaluating ulnar-sided wrist pain despite the invasiveness of the procedure. Diagnostic accuracy may vary depending on location of the TFCC injury, however, as some authors report superior results at detection of central and radial tears versus those involving the radioulnar ligaments [33]. MRI or MRA findings should always be considered in the context of the history and physical exam, however, as the rate of TFCC abnormalities on MRI in asymptomatic adults has been reported as 33.7 % in those under 50, 62.5 % in those 50–59, and 100 % in those over 60 [37].
Treatment of Type 1A TFCC Tears
In the absence of DRUJ instability most acute TFCC injuries can initially be managed nonoperatively, with up to 57 % of patients symptom-free after 1 month [38]. Temporary splinting or casting of the wrist for up to 2–6 weeks along with oral analgesics and anti-inflammatory medications relieves pain and may allow peripheral tears to heal without surgery. While Type IA tears do not have a good intrinsic ability to heal, they are typically not structurally significant for wrist biomechanics and corticosteroid injections to the ulnocarpal joint can eliminate inflammation surrounding the tear, thus eliminating pain and avoiding surgical intervention in many cases [22]. Cortisone injection should not be undertaken within the first 6 weeks after symptom onset so as not to interfere with the normal biologic processes of healing. Patients with persistent pain despite nonoperative treatment or with instability of the DRUJ are indicated for surgery. High-performance athletes with confirmed TFCC tears on imaging can also be considered for early operative intervention [39, 40]. Arthroscopy is considered the gold-standard diagnostic modality to evaluate the TFCC, and the majority of tears can be treated with this approach.
Arthroscopic Evaluation
The patient’s wrist is positioned, traction applied, and arthroscopic access established as described in Chap. 1. Initial evaluation is typically performed with the arthroscope placed in the 3,4 portal and instrumentation in the 6-R portal. Inflow pressure should be minimized in order to allow the TFCC to assume a more normal position within the ulnocarpal joint and minimize blanching, which allows for easier identification of inflamed soft tissue. Visual examination for obvious signs of injury or tears is performed, and associated synovitis or chondromalacia is also noted (Fig. 5.2a). Pronation and supination may aid in visualization of the entire TFCC, and stability of the DRUJ can be assessed with manual stress testing. If necessary, the arthroscope may also be moved to the 6-R portal to better view the radial and ulnar attachments of the disc. A probe is used to assess the integrity of the fibrocartilage by palpating the disc for intrasubstance tears, and when depressed it should readily spring back into its normal position (Fig. 5.2b). Loss of this so-called trampoline effect can indicate either peripheral or foveal detachment [41]. The hook and drag tests use the probe to apply traction along the periphery of the TFCC, and displacement vertically or in the direction of traction similarly indicates either a peripheral tear or foveal injury [6]. If a reparable tear is identified, its full extension must be explored in order to determine whether the repair should be to the subsheath only or, in the case of deep fiber involvement, directly to the ulna [15].
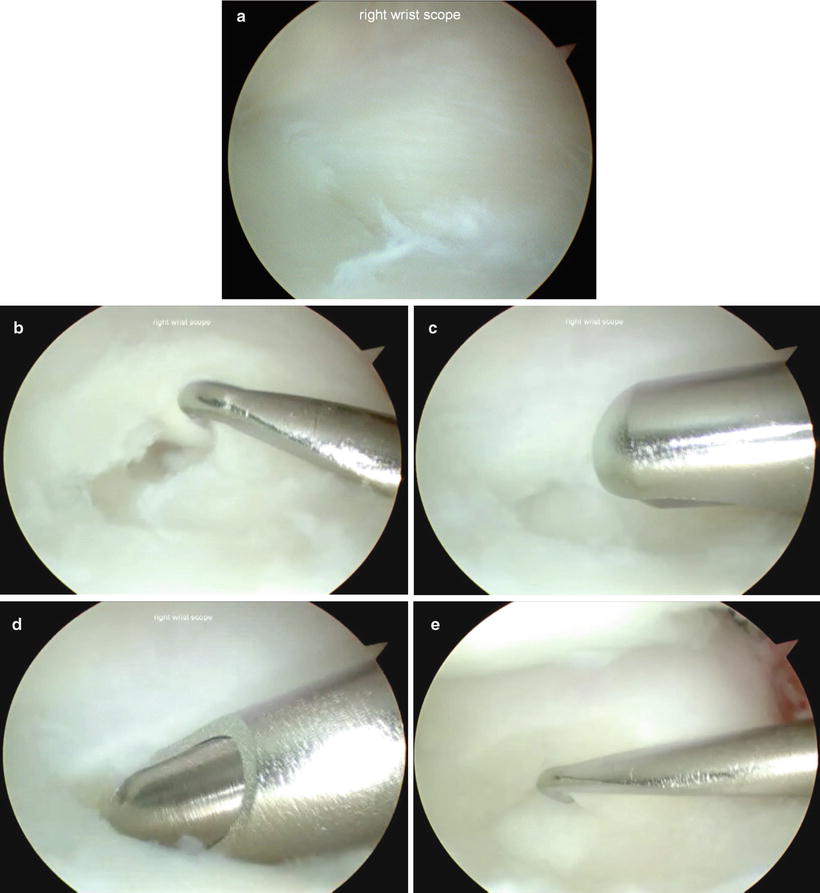
Fig. 5.2
(a) Demonstrates the arthroscopic appearance of a Type 1A TFCC tear, the extent and margins of which are defined with the aid of a probe (b). An arthroscopic shaver or other instrument is used to debride the unstable flaps of the tear back to stable edges, taking care to avoid the volar and dorsal radioulnar ligaments (c, d). The margins are then rechecked with the probe to confirm the adequacy of resection (e)
Arthroscopic Debridement of Type 1A Tears
Once the diagnosis of a Type 1A tear is made, arthroscopic debridement is the treatment of choice given the central disc’s poor vascularity and inability to heal. Detailed management of tears amenable to repair will be covered in subsequent chapters. The goal of the procedure is to debride unstable flaps of the central fibrocartilage that are likely to catch on surrounding tissue back to a stable rim. Biomechanical studies demonstrate that up to 2/3 of the central region can safely be resected without destabilizing the DRUJ; more important is to avoid damage to the peripheral 2 mm of the TFCC as this tissue contains the dorsal and volar radioulnar ligaments [14, 42] (Video 5.1). Debridement techniques have been described with multiple instruments including scalpels, banana blades, shavers, radiofrequency probes, and lasers [43–45]. Each has its own advantages and disadvantages, and the ideal instrument is ultimately the surgeon’s preference. Ours is to use a banana blade or arthroscopic shaver to perform the bulk of resection followed by radiofrequency ablation, if necessary, to stabilize the borders of the resection (Fig. 5.2c, d). As with arthroscopic evaluation, debridement is started with the arthroscope in the 3,4 portal and instrumentation is introduced via the 6-R portal. The radial side of the torn fibrocartilaginous disc is outlined and resected with the blade, then removed with an arthroscopic grasper. The arthroscope is then moved to the 6-R portal, and with instrumentation through the 3,4 portal the same procedure is performed on the ulnar side of the tear. The TFCC is then reexamined to ensure the absence of any further unstable tissue and the integrity of the peripheral ligaments (Fig. 5.2e). The LT ligament and articular surfaces should also be examined and repair or debridement performed as indicated. In most cases, acute IA tears should not have significant carpal chondromalacia or LT ligament insufficiency as these are more often seen with chronic Type II patterns.
In the case of a patient with a Type 1A tear and concomitant positive ulnar variance, most authors argue for the addition of a primary ulnocarpal decompression along with TFCC debridement [8, 22, 28, 29, 46, 47]. The ulnar-shortening osteotomy [46] and ulnar wafer procedure [47] have both been proposed as treatment options that can be combined with arthroscopic debridement. In an early report of arthroscopic TFCC debridement Osterman noted some patients with positive ulnar variance to have degenerative chondromalacia of the ulnar head despite traumatic mechanisms, suggesting some tears may be acute-on-chronic injuries [48]. Minami subsequently reported that patients with positive ulnar variance have inferior outcomes compared to those with neutral or negative variance after debridement alone, and argued for primary ulnar-shortening osteotomy for these patients [46, 49]. Ulnar-shortening osteotomy is also a successful secondary procedure for persistent pain after primary debridement regardless of preoperative ulnar variance [50], suggesting dynamic positive ulnar variance may contribute to failure even if routine X-rays are normal [51]. In comparing primary ulnar wafer resection to ulnar-shortening osteotomy, when combined with debridement both show equivalent postoperative pain relief and function. Higher rates of tendinitis and reoperation (for hardware removal) have been reported with ulnar-shortening osteotomy, however [28, 52].
As previously discussed, if only the central region of the TFCC is debrided and the periphery remains intact, the biomechanics and stability of the wrist will not be affected. Further, as there is no repair to protect, postoperative immobilization is unnecessary and patients are able to begin rehabilitation immediately, including unrestricted active and passive motion and light progressive strengthening once pain is diminished [42]. If an ulnar-shortening osteotomy or ulnar wafer resection is performed a splint is used for 6 weeks to protect the osteotomy or allow a clot (and subsequently fibrocartilage) to form over the distal ulna, respectively. Strengthening exercises are delayed until the osteotomy is healed radiographically in the setting of an ulnar shortening (typically 6–8 weeks)
Results
Arthroscopic debridement has become the treatment of choice and standard of care for Type 1A TFCC tears, offering superior visualization of the TFCC with a less invasive approach and superior outcomes when compared to open procedures. In separate studies, Osterman and Roth both described the initial technique of arthroscopic TFCC debridement [48, 53]. Osterman also reported on 52 patients prospectively followed after arthroscopic debridement with either a motorized shaver or pituitary rongeur for traumatic or degenerative TFCC tears. At an average follow-up of 23 months, 73 % were pain-free and 12 % further were improved; amongst the five patients who failed treatment no relationship to ulnar variance was identified [48]. Subsequent studies have found similar results. Comparing arthroscopic debridement in 11 posttraumatic vs. 5 degenerative cases, Minami found a posttraumatic etiology to be associated in all cases with an excellent recovery based on superior patient satisfaction, pain relief, and function [49]. Using Minami’s criteria, Miwa also found good or excellent results in 9/10 patients undergoing debridement for Type 1A tears [54]. Using the modified Mayo Wrist Score, Husby and Haugstvedt reviewed 32 patients at a median of 39 months after arthroscopic debridement and found 27 good or excellent results vs. 4 fair and 1 poor result; all but 2 patients in their study would have had surgery performed again [55].
Amongst patients failing debridement alone, Hulsizer found a subsequent ulnar shortening osteotomy resulted in complete relief of pain for 12/13 patients regardless of preoperative ulnar variance [50]. In cases of positive ulnar variance, failure rates of up to 25 % have been described for debridement alone [49], and primary procedures to decompress the ulnocarpal joint should be considered in addition. Outcomes after debridement with ulnar-shortening osteotomy or an ulnar wafer procedure are equal or superior to those published for debridement alone. However, rates of reoperation, most commonly removal of osteotomy hardware, as well as ulnar-sided tendinitis are higher with ulnar-shortening osteotomy, leading some authors to favor the wafer procedure [28, 52]. Animal models also suggest that the clot formed by bleeding from the distal ulna may allow for fibrous reconstitution of the debrided central TFCC, but this has yet to be shown in humans [56].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








