Fig. 4.1
The larger radius of curvature of the sigmoid notch compared to the ulnar head can be seen. With minimal bony restraints the stability of this joint is dependent on soft tissue structures. The fovea (F) of the ulnar head where the deep portion of the volar and dorsal radioulnar ligaments is seen along with the ulnar styloid (US) where the superficial portions of the radioulnar ligaments attach. (Specimens provided by the Anatomical Gifts Program at the University of Mississippi Medical Center)
The thin capsule of the DRUJ attaches distally from the sigmoid notch of the radius to the volar and dorsal aspects of the radioulnar ligaments of the TFCC before inserting on the base of the ulnar styloid. Due to these attachments, the tip of the ulnar styloid is extra-articular in relation to this joint [4]. Clinically peripheral detachments are more common dorsally, as the volar attachment of the capsule to the TFCC is stronger [5].
During normal forearm supination and pronation, a sliding movement occurs in addition to a rotational movement. In neutral rotation, the principal axis of load bearing of the DRUJ is centrally in the sigmoid notch, with approximately 60 % of cartilage surface contact. With pronation, the principal axis of load bearing of the DRUJ moves distally and dorsally in the sigmoid notch, leaving a small portion, approximately 10 % of the cartilage surface of the notch, in contact with the ulna. In supination, the reverse is true with the principal axis of load bearing moving proximally and palmarly in the sigmoid notch [2, 6, 7].
To maintain stability of this inherently unstable joint, the function of the DRUJ is intricately related to soft tissue structural support. Both extrinsic and intrinsic structures are present, with the intrinsic stabilizers playing a greater role in rotational stability [1]. Extrinsic stabilizing structures that will not be described in detail in this chapter include the extensor carpi ulnaris tendon, the sixth dorsal compartment, the pronator quadratus, and the interosseous ligament of the forearm [1, 3]. The TFCC is the primary intrinsic stabilizer of the DRUJ, with the volar and dorsal radioulnar ligaments providing the majority of the support the TFCC imparts to the DRUJ.
Ulnar Variance
As ulnar variance plays a role in TFCC pathology and in the treatment options for ulnar-sided wrist pain, an understanding of the biomechanics of this relationship is needed. As the radius rotates around the fixed ulna, the variance changes with position, being relatively ulnar positive in pronation and ulnar negative in supination (Fig. 4.2a, b). The differences in load transmission through the ulnocarpal joint with differing degrees of ulnar variance or wrist position can be significant. The force transmitted through the ulna has also been found to increase with pronation, extension, and ulnar deviation as this shifts the load medially compared to supination, flexion, and radial deviation [1, 8]. In addition, forced grip has been found to increase ulnar variance an average of 1.95 mm, which will increase load transmission through the TFCC and ulna [9].
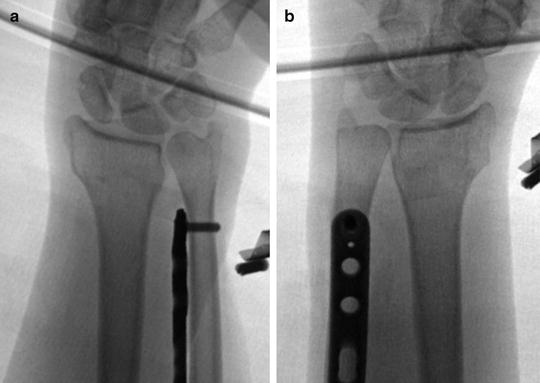
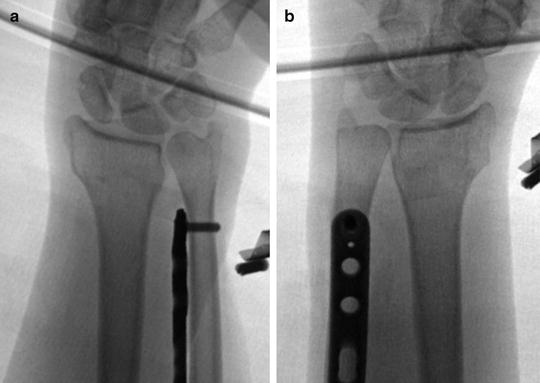
Fig. 4.2
(a and b) Flouroscopic images showing the positional changes in ulnar variance with pronation (a) and supination (b). In pronation the wrist is found to be significantly ulnar positive, while in supination the wrist is minimally positive in these images
In a patient with neutral variance, approximately 80 % of the load of the carpus will be transmitted through the radius and 20 % through the TFCC and ulna. If the variance increases by 2.5 mm, the load borne by the ulna will increase to approximately 40 %, while a decrease in variance of 2.5 mm will decrease the load borne by the ulna to approximately 4 % [10]. In addition to the increased load transmitted through the articular disc with increased variance, the space available for the TFCC is diminished, leading to a decreased thickness of the disc [11]. This increased load borne through the TFCC with increased ulnar variance helps explain the association with TFCC injuries, as greater loads and stresses are placed on this structure that already has a decreased thickness [1, 11]. In Palmer and Werner’s cadaveric study, they found TFCC perforations in 17 % of ulnar minus wrists compared with 73 % in ulnar plus or neutral wrists [12].
Radiographic Evaluation
For a complete evaluation of the wrist, an accurate PA and lateral radiograph should be obtained to evaluate carpal and DRUJ pathology, variance, and carpal malalignment. Due to the positional difference in the relationship of the distal radius and ulna, the recommended positioning when taking X-rays to assess for variance is that the forearm be in the zero or neutral rotation position for accurate measurements. A reliable way to obtain this view is with the shoulder abducted 90° and the elbow flexed 90° with the hand flat so that accurate reproducible results can be obtained in subsequent imaging studies [13]. When viewing the radiograph, the ulnar styloid should be at the greatest distance possible from the radius, and if it is not in this position, then the wrist is either pronated or supinated [13]. Another reliable method for obtaining acceptable radiographs is with the arm adducted to the side and the elbow flexed to 90° with the hand in neutral rotation and the thumb towards the ceiling. In this fixed position the X-ray beam can be rotated 90° to obtain a true PA and lateral radiograph.
Triangular Fibrocartilage Complex
The TFCC is a critical and complex structure that is integral to the normal kinematics and function of the wrist. Palmer and Werner, in their anatomic and biomechanical testing, described the anatomy of the TFCC as being composed of the articular disc, the meniscus homologue, the ulnar collateral ligament, the sheath of the extensor carpi ulnaris, and the dorsal and volar radioulnar ligaments (Fig. 4.3) [12]. The TFCC originates on the sigmoid notch before inserting on the ulna fovea and styloid, and distally it joins with the ulnar collateral ligament before inserting on the triquetrum, hamate, and base of the fifth metacarpal [12]. While not initially described as part of the TFCC by Palmer, the ulnocarpal wrist ligaments have since been included as components and are important stabilizers of the ulnocarpal joint [14].
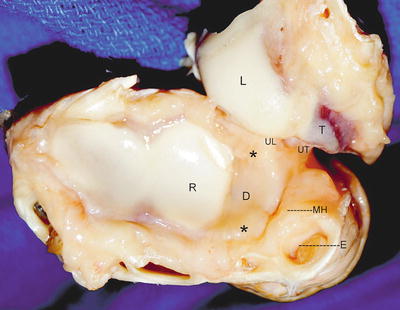
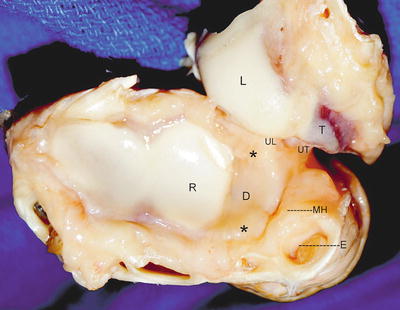
Fig. 4.3
Specimen demonstrating the different components of the ulnar side of the wrist and TFCC. L lunate, T triquetrum, R lunate facet of radius, UT ulnotriquetral ligament, UL ulnolunate ligament, D articular disc, asterisk volar and dorsal radioulnar ligaments, MH meniscus Homologue, E extensor carpi ulnaris subsheath
These structures forming the TFCC are important in load transmission through the ulnar side of the wrist and are intrinsic stabilizers of the distal radioulnar and the ulnocarpal joints. The TFCC enlarges the contact area between the carpal bones and the ulna and transmits load between these structures. The wide but slim radial attachment is subjected to large amounts of stress during motion and is often a site of tears [15]. The importance of the TFCC in force transmission is demonstrated with resection of the articular disc, which unloads the ulnar column and decreases the load transferred through the ulna from 18 % to approximately 6 % [16]. The ulnocarpal ligament components of the TFCC contribute very little to DRUJ stability, but are significant in their contribution to ulnocarpal stability. Due to the very limited inherent bony stability of the DRUJ, the major stabilizer of this joint is the TFCC, with the palmar and dorsal radioulnar ligaments playing the most vital role in this process.
Ulnocarpal Ligaments
The ulnocarpal ligaments serve an important role in stabilizing the ulnar carpus and helping prevent supination and volar translocation of the carpus on the distal radius and ulna [17]. Stuart et al. found in their biomechanical study testing the relative contributions to stability of the DRUJ that the ulnocarpal ligament complex was not a significant contributor [3]. Although not always included as a part of the TFCC, the ulnocapitate ligament originates from the palmar aspect of the fovea, where it blends with the palmar radioulnar ligament and then runs superficial to the other ulnocarpal ligaments before inserting onto the capitate [18]. The ulnotriquetral ligament arises from the palmar aspect of the fovea and the meniscus homologue and the palmar radioulnar ligament before inserting on the triquetrum. The pisotriquetral orifice may be seen in the distal aspect of this ligament during arthroscopy. The ulnolunate ligament originates from the palmar aspect of the fovea and the articular disc, with a few fibers from the radius, and is intertwined with the palmar radioulnar ligament before inserting distally on the lunate (Fig. 4.4) [14, 19].
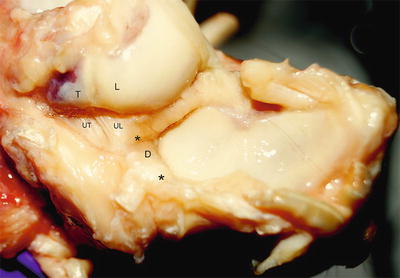
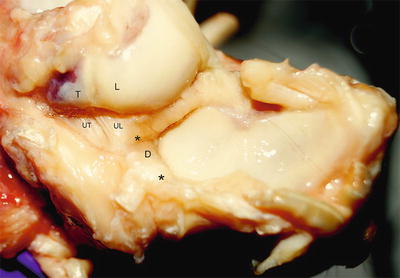
Fig. 4.4
The ulnolunate and ulnotriquetral ligament can be seen arising from the volar distal radioulnar ligament before inserting distally on the lunate and ulna, respectively. The ulnocapitate ligament is not seen as it runs volar to the other ulnar carpal ligaments. The volar and dorsal radioulnar ligaments appear as thickenings of the peripheral articular disc. L lunate, T triquetrum, UT ulnotriquetral ligament, UL ulnolunate ligament, D articular disc, asterisk volar and dorsal radioulnar ligaments
Moritomo et al. found that the length of the ulnotriquetral and ulnocapitate ligaments increased the greatest amount with wrist radial extension, whereas the ulnolunate increased the most with wrist extension, while the palmar radioulnar ligament had minimal change in length with any motion. This stress imparted through the ligaments might explain how a fall on an outstretched hand could lead to a foveal tear of the TFCC from excessive traction imparted through the ulnocarpal ligaments. Morimoto goes on to say, however, that pure wrist hyper-radial extension or hyperextension would not be adequate by itself to cause these injuries and that additional forces would be required to initiate a tear [19].
Meniscus Homologue
The meniscus homologue is a C-shaped vascular tissue located between the superficial portion of the radioulnar ligaments, the capsule, and the triquetrum in the ulnar aspect of the radiocarpal joint. Some debate has occurred over whether this is a true component of the TFCC, as it differs histologically by being composed of loose connective tissue instead of dense collagen and also by being lined by synovial cells on its inner surface [18]. Ishii et al. found in their study that the meniscus homologue, which they classified into three types as related to the prestyloid recess, was not identifiable as the separate structure that was previously described by Bowers and Taleisnik [14, 20, 21].
Prestyloid Recess
The prestyloid recess is a pouch often found anterior to the ulnar styloid where the meniscus homologue does not cover the ulnar styloid, and should not be confused with a tear of the TFCC [18]. It can be found at the apex of radioulnar ligaments and is typically lined with synovial villi (Fig. 4.5) [22]. Ishii described three different variations in the prestyloid recess: narrow, wide, and no-opening types [14]. The narrow opening type was found in 74 % of specimens and consisted of the meniscus homologue being attached to the ulnar styloid proximal to its radial, dorsal, and palmar aspects and distal to the ulnar styloid tip circumferential surface [14]. The prestyloid recess was found to communicate with the ulnocarpal space by a long narrow tunnel from the palmar aspect of the styloid [14]. The wide opening type was found in 11 % and consisted of the attachments similar to the narrow opening, but without attachment to the tip of the styloid [14]. A short, wide opening was found between the prestyloid recess and the ulnocarpal space [14]. The no-opening type was found in 15 % of patients, and the prestyloid recess was found to come from the radial aspect of the styloid and to communicate with the distal radioulnar joint instead of the ulnocarpal space [14]. The ligamentum subcruentum, as it was originally described, was not found in this type, but was identified in the narrow and wide opening variations [14].
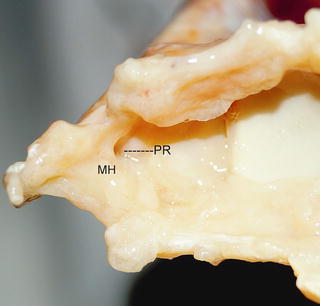
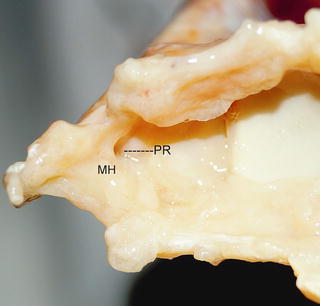
Fig. 4.5
The prestyloid recess is seen and is often found anterior to the ulnar styloid and is the area where the styloid is not covered by the meniscus homologue. The meniscus homologue (MH) composed of loose connective tissue located in the ulnar aspect of the radiocarpal joint and is seen to the left and inferior to the prestyloid recess (PR) in this image
Radioulnar Ligaments
The dorsal and palmar radioulnar ligaments are intracapsular intrinsic stabilizers that measure 4–5 mm in thickness and impart the majority of stability to the DRUJ in pronation and supination as translational motion occurs [1–3, 12]. The histologic makeup of these ligaments demonstrates longitudinally-oriented parallel fibers, which suggest a tissue that experiences tensile loads, a premise which supports their role as stabilizing structures [23]. The palmar radioulnar ligament forms the proximal attachment of the ulnocarpal ligaments, while the dorsal radioulnar ligmanent splits ulnarly to form the subretinacular sheath of the extensor carpi ulnaris [15]. These ligaments have both a superficial and deep portion with the insertions on the ulnar styloid and fovea, respectively (Fig. 4.6) [1, 24]. At their broad radial attachment at the distal rim of the sigmoid notch, the radioulnar ligaments are conjoined, but then split prior to reaching the ulnar styloid or fovea into a superficial and a deep portion (Fig. 4.7) [2, 14]. The insertion of the deep portion, commonly called the ligamentum subcruentum, is more lateral and proximal into the fovea compared to the more central and distal insertion of the superficial ligament. The palmar and dorsal portions of the deep ligament converge and intertwine as they insert into the fovea (Fig. 4.8) [15]. The original description of the ligamentum subcruentum was of a vascularized space separating the proximal deep and distal superficial portions of the TFCC, but this term has changed over time to describe the insertion of the deep component of the ligaments [1, 24]. Ishii, in a cadaveric study, found that the deep portion inserts on the fovea, but that there was not a clearly distinct insertion site of the superficial ligament on the styloid [14].
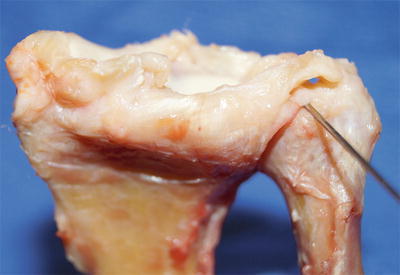
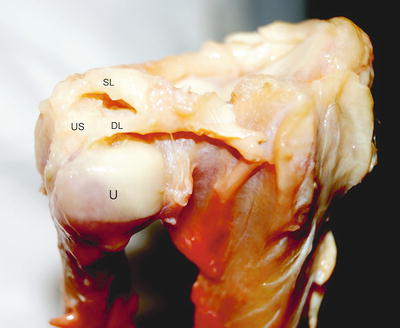
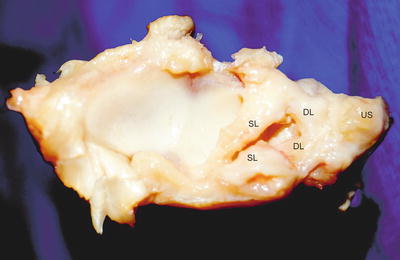
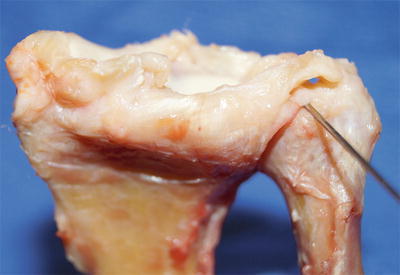
Fig. 4.6
Specimen demonstrating both the superficial and deep volar radioulnar ligaments. The superficial ligament can be seen inserting on the styloid, and the deep ligament (located superior to the needle) can be seen inserting into the fovea
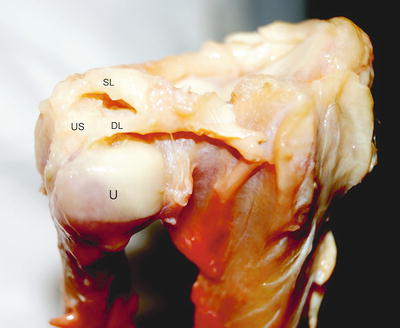
Fig. 4.7
The conjoined deep (DL) and superficial (SL) dorsal radioulnar ligament can be seen prior to splitting and inserting into their respective sites onto the fovea and the ulnar styloid (US). U ulnar head
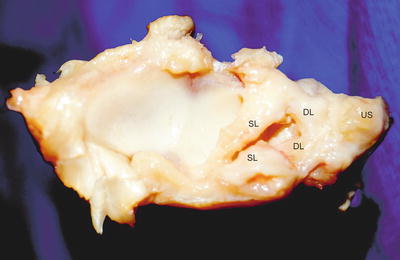
Fig. 4.8
A specimen showing the deep portion of the volar and dorsal radioulnar ligaments (DL) converging prior to inserting into the fovea. The articular disc has been resected and the superficial radioulnar ligaments (SL) have been released from the ulnar styloid (US) and retracted
The insertion of the deep component of the ligament provides a better mechanical advantage for controlling rotation as its angle of insertion is less acute than that of the superficial ligament [1]. To demonstrate this concept, Kleinman uses the analogy of a team of horses, a buckboard, and a driver, in which the radius is the team of horses, the ulna is the buckboard, and the different angles of the reins going to the driver represent the deep and superficial ligaments [1]. This analogy shows how the less-acute angle of the reins, which represents the deep ligament, is more advantageous in controlling the rotation of the horses, which represents the radius [1]. The radioulnar ligaments have a spiral configuration as they insert onto the ulnar head, and this rotational insertion, along with the differing locations of insertion of the deep and superficial ligaments, allows continuous shifts in tension and compression and is the core of DRUJ stability [7].
The superficial radioulnar ligaments also provide stability to the DRUJ, but their action is the opposite of the deep ligaments, with the dorsal fibers giving stability in pronation and the palmar fibers providing stability in supination. While the superficial fibers do provide stability, they have a more acute angle of insertion and thus less mechanical advantage for rotational control. The second reason the superficial ligaments play a lesser role is that in maximum pronation or supination, the majority of the ulna has escaped out from under the superficial fibers, rendering them ineffective in these extremes of motion (Fig. 4.9a, b). In this position, the deep portion of the radioulnar ligament provides stability by providing a tethering action, thus preventing dislocation of the DRUJ [1, 2].
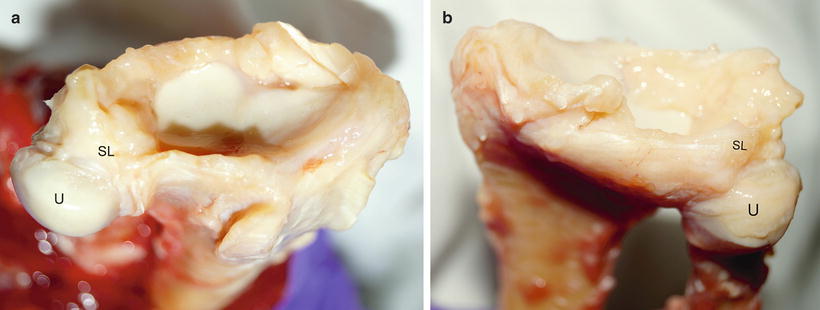
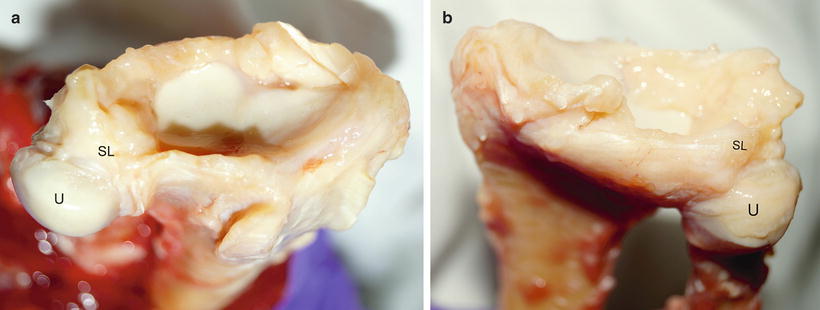
Fig. 4.9




(a and b) The ulnar head can be seen escaping from underneath the superficial fibers of the dorsal radioulnar ligament in maximum pronation (a), and the volar radioulnar ligament in maximum supination. This demonstrates how the superficial fibers have a diminished role in the stability of the DRUJ in the extremes of motion, and the majority of the stability is provided by the tethering role of the deep portion of the radioulnar ligaments. SL superficial portion of the radioulnar ligament, U ulnar head
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








