Posttrauma
Postsurgery
1.Fracture
1.Dorsal wrist ganglia
2.Fracture-dislocation
2.Treatment of scaphoid fractures or nonunion
3.Dislocation
3.Inter-carpal arthrodeses
4.Ligament injuries
4.Ligament reconstruction
5.Proximal row carpectomy
•Prolonged immobilization
Conservative treatment with physiotherapy and splinting is the treatment of choice. Surgery is reserved for those cases refractory to conservative treatment. Arthroscopic treatment of arthrofibrosis of the knee, shoulder, and elbow is well established and commonly used.
Frequently, incorrect or incomplete reduction of a distal radius fracture is the cause of a stiff and painful wrist. Intra-articular and extra-articular malunions need to be corrected with osteotomies to restore normal anatomy and alignment of the articular surface of the distal radius [3]. Following distal radius fractures, two main conditions can contribute to painful limitation of ROM: (1) capsular contracture with intra-articular adhesions (most commonly), and (2) radiocarpal impingement caused by either malunion of fractures involving the dorsal rim of the distal radius (Figs. 14.1 and 14.2) or an increase in volar tilt of the distal radius articular surface. The two conditions can sometimes coexist and must be treated at the same time. It is important to note the rehabilitation protocol for the various surgical procedures that may need to be performed. Any procedure that would involve postoperative immobilization such as ligament reconstructions must be avoided. Immediate mobilization following surgery is mandatory.
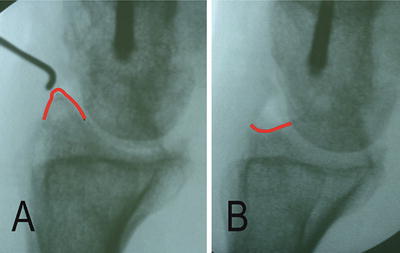
Fig. 14.1
Drawing showing malunion of the dorsal rim of the distal radius following fracture (a). Note the impingement between the dorsal rim and the carpus (b)
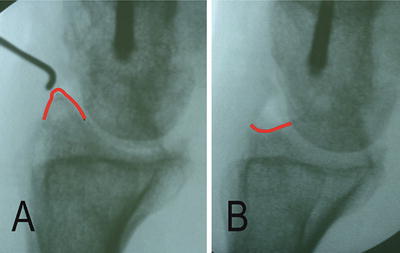
Fig. 14.2
Lateral radiograph of a wrist showing dorsal impingement (arrow) of the distal radius following malunion of a fracture. (a) Before and (b) after arthroscopic debridement of dorsal rim [Courtesy of Francisco del Piñal]
Other potential causes of wrist pain and stiffness include neuroma of the posterior interosseous nerve (PIN), extensor and/or flexor tendons adhesions, and chronic regional pain syndrome (CRPS).
Traditionally, wrist manipulation under anesthesia (MUA) is commonly used when the rehabilitation regime has failed to improve wrist ROM. However, this procedure can be detrimental by causing traumatic ligamentous injuries, chondral or osteochondral damage (especially in cases with dorsal radiocarpal (RC) impingement) or even fractures. Surgical arthrolysis is a gentler and more controlled option that can be performed via open or arthroscopy surgery [4, 5]. This is already a successful treatment option in other joints [6–8].
Arthroscopic arthrolysis of the wrist allows the surgeon to treat the RC and intercarpal joints, whilst minimizing the risk of secondary damage to other articulations, and at the same time permitting immediate postoperative mobilization [9–15].
Technique
Traditional RC portals are used for arthroscopic arthrolysis of the wrist. Two volar portals (radial and ulnar) may also be used for the RC and ulno-carpal (UC) joint [6]. The distal radioulnar joint (DRUJ) may also be involved in the pathological process, and may also be debrided arthroscopically. The midcarpal (MC) joint is rarely involved; however, if it is affected, traditional MC portals are used.
Arthrolysis may be performed using a variety of instruments (Table 14.2). Dry arthroscopy is utilized more frequently for this condition as it has the benefit of avoiding fluid extravasation into the soft tissues [16, 17].
Table 14.2
Instruments for arthroscopic arthrolysis
Motor powered |
•Full radius blade |
•Cutter Blade/Incisor |
•Razor cut blade |
•Barrel abrader |
Suction punch |
Mini-scalpel (banana blade) |
Laser |
Radiofrequency |
Dissector and scalpel |
Articular distraction is obtained using the traditional vertical position with counter-traction at the elbow of about 3 kg. Occasionally the articular distraction is not sufficient enough to permit the use of a 2.7 mm scope even when more traction weight is applied. In these cases a 1.9 mm scope is recommended.
Although arthroscopy starts at the level of the RC joint, the MC joint should always be assessed. When there is a loss of pronation and supination, arthrolysis of the DRUJ should also be performed.
In the most difficult cases, it is impossible to recognize the normal arthroscopic anatomy of the wrist due to the presence of fibrosis that completely encloses the joint space. Difficulties could be encountered in performing triangulation with the instruments. Synovitis, fibrosis, and adhesions that obstruct the visual field, must be resected with caution, ensuring that no damage occurs to the surrounding structures. Obviously, the surgeon’s surgical ability is of utmost importance here.
Radiocarpal Joint
All the portals (1-2, 3-4, 4-5, 6R, and 6U) may be used, including the volar ones, if needed. Inflow is permitted through the scope. Outflow by 6U portal or none. When dry arthroscopy is used, the trocar inflow portal is left open permitting the entrance of air as the shaver is used with constant aspiration. This allows removal of synovial fluid, blood, and debris. Furthermore, a 5 cc syringe can be used to inject fluid in order to wash the joint debris and blood, which is then removed by the suction of the shaver. Only when the radiofrequency instrument is used, does fluid become necessary. Once the radiofrequency is no longer required, it is possible to return to dry arthroscopy by using the shaver to aspirate fluid and debris in the joint.
The procedure is divided into two steps to permit a better understanding of the technique.
Step One: Fibrosis and Fibrotic Band Resection
Arthroscopic arthrolysis always starts from the radial side of the RC joint (Fig. 14.3). The starting portal is usually the 3-4 and the 1-2 is used as a working portal, however, portals are switched frequently.
Fig. 14.3
Drawing showing the division of the radiocarpal joint into three parts. The proper radiocarpal joint is divided into two parts by a longitudinal line passing through the scapholunate joint. The ulnocarpal joint is separated from the radiocarpal joint by a longitudinal line through the medial border of the radius at the sigmoid notch. The ulnocarpal joint is rarely involved. In this drawing fibrosis is located in the radiocarpal joint, the DRUJ and under the TFCC ligament
Adhesions are initially removed from the radial side of the joint using the shaver (full radius: 2.9 mm, aggressive or incisor: 3.2 mm) and radiofrequency instruments. However, not infrequently, difficulties are encountered in triangulation due to intense intra-articular fibrosis. In these circumstances, it is better to switch the scope from the 3-4 portal to the 1-2 portal and use the 3-4 portal as the working portal. The 1-2 portal is established with an outside-in technique using a needle. A longitudinal skin incision is made and blunt dissection with a mosquito forceps is performed to gain access to the joint. Shaving should only be started after ensuring that the full radius is turned towards the scope and not to the articular surface. As the intra-articular vision improves, the resection of fibrosis becomes easier.
Once fibrosis is completely removed from the radial side of the RC joint, the arthroscopic procedure is shifted to the ulnar side (Fig. 14.4). The scope is introduced through the 3-4 portal and the shaver through the 6R. Visualization of the shaver is frequently limited by the presence of the fibrotic band. Traditionally the fibrotic band [14] is localized between the scapho-lunate (SL) ligament and the ridge between the scaphoid and lunate facet of the distal radius (Figs. 14.5 and 14.6). It may be partial or complete. When it is complete, it divides the radio-carpal joint into two separate spaces. The fibrotic band may be incised using a small dissector introduced via the 6R portal in the direction of the scope. The band is carefully detached from the articular surface using the dissector. The fibrotic band may then be resected using a basket forceps or a shaver from the 6R portal (Fig. 14.7). To obtain a complete resection of the band, instruments must be switched from the 6R to 3-4 portal and scope from 3-4 to 6R. Radiofrequency instruments may also be used to resect the fibrotic bands. Multiple fibrotic bands may be encountered in a joint with osteochondral damage to the articular surface of the distal radius (Fig. 14.8), with all of them originating from the defect.
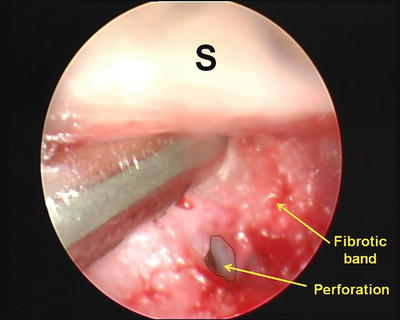
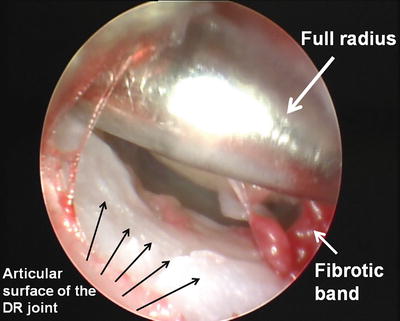
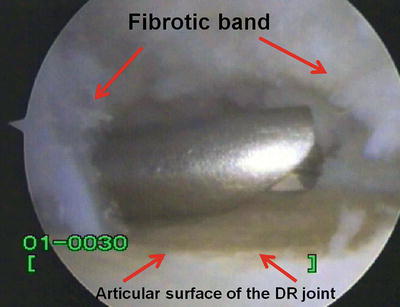
Fig. 14.4
Drawing showing division of the radiocarpal joint into three parts, where fibrosis in the radial side has been removed (step 1)
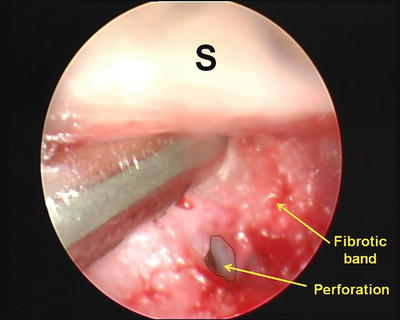
Fig. 14.5
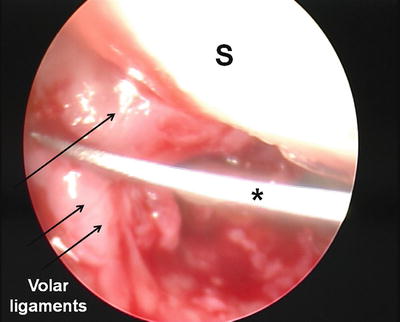
Arthroscopic view of the fibrotic band that has resulted in a virtually complete separation of the radiocarpal joint in two compartments. A shaver is being used to excise the fibrotic band (S—scaphoid)
Fig. 14.6
Drawing showing the location of the fibrotic band
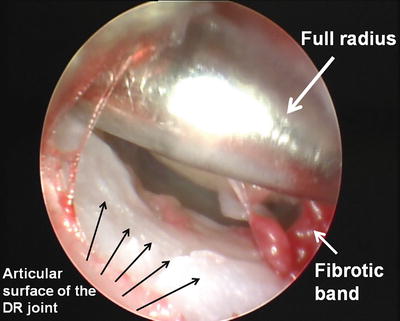
Fig. 14.7
Arthroscopic view of the wrist joint after fibrotic band resection. Note the irregularity of the articular surface of the distal radius due to a previous fracture
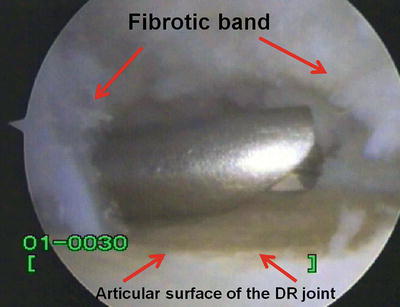
Fig. 14.8
Cartilage damage to the articular surface of the distal radius becomes evident after resection of the fibrosis
Resection of this intra-articular fibrosis is often sufficient to improve passive wrist ROM. However, on occasion this fibrosis may be much more complex making arthrolysis much more difficult. Rarely these bands may ossify and form an osteofibrotic band, and with progression may result in an ankylosis of the RC joint (Fig. 14.9). In this situation it is very difficult to remove the band and may sometimes be impossible. Resection of these osteofibrotic bands may not be indicated if it will cause an osteochondral defect that would then result in persistence of pain and recurrent formation of the bands.


Fig. 14.9
X-ray of a wrist showing an ankylosis of the radio-lunate joint due to progression of an osteofibrotic band
When fibrosis in the ulnar side of the RC joint has been completely excised, the procedure continues into the ulno-carpal joint (Fig. 14.10). This part of the wrist joint is rarely affected by fibrosis, and arthroscopy is often diagnostic only. Occasionally, peripheral TFCC tears may be found, however, the treatment these should be limited to a debridement in order to avoid the need for postoperative immobilization.
Fig. 14.10
Drawing showing complete resection of fibrosis in the radiocarpal joint
Before moving to the second step of the procedure, it is mandatory to evaluate the wrist ROM (Fig. 14.11). This should be performed out of traction.
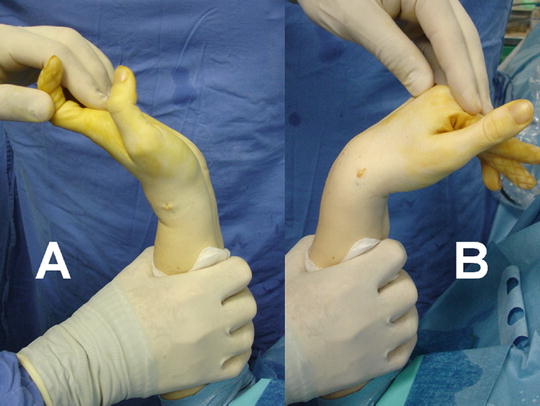
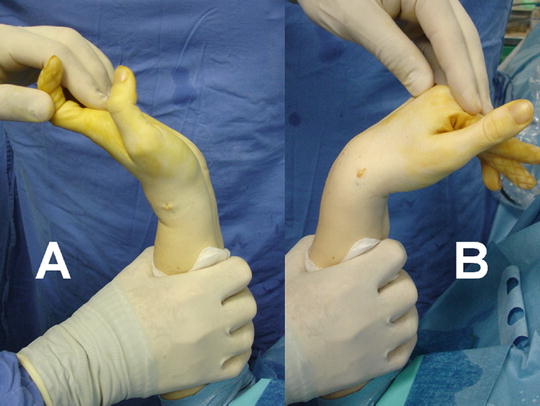
Fig. 14.11
Wrist ROM evaluation after step one of the arthroscopic arthrolysis procedure
Step Two: Volar and Dorsal Capsule Resection
Depending on the ROM obtained after step one, the volar and/or dorsal capsule and RC ligaments may need to be released. A mini-scalpel, such as a banana blade for peripheral nerve surgery, or micro-scalpel for ocular surgery is used. Radiofrequency instruments may also be used. Volar capsulotomy is easier than dorsal because the structures are immediately in the field of vision when viewing from the dorsal arthroscopy portals. Initially, the shaver is used to debride the intra-articular portion of the volar ligaments in order to see the entrance point of the mini-scalpel. Once inside the joint the surgeon addresses each affected ligament (Fig. 14.12). Often this is made difficult by articular incongruity, making it impossible to reach all areas of the capsule. This may be made easier by smoothing off the articular steps using a shaver (burr) that helps in reaching the volar capsule. It is much easier to cut the radial side of the capsule from the 1-2 portal with the scope in the 3-4 portal.