Class IA
Tears or perforations of the horizontal portion of the triangular fibrocartilage complex (TFCC)
Usually 1–2 mm wide
Dorsal palmar slit located 2–3 mm medial to the radial attachment of the sigmoid notch
Class IB
Traumatic avulsion of TFCC from insertion into the distal ulna
May be accompanied by a fracture of the ulnar styloid at its base
Usually associated with distal radiocarpal joint instability
Class IC
Tears of TFCC that result in ulnocarpal instability, such as avulsion of the TFCC from the distal attachment of the lunate or triquetrum
Class ID
Traumatic avulsions of the TFCC from the attachment at the distal sigmoid notch
Table 6.2
Classifications of degenerative lesions class II
Class IIA | Wear of the horizontal portion of the TFCC distally, proximally, or both; with no perforation |
Possible ulnar plus syndrome | |
Class IIB | Wear of the horizontal portion of the TFCC and chondromalacia of lunate and/or ulna |
Class IIC | TFCC perforation and chondromalacia of the lunate and/or ulna |
Class IID | TFCC perforation and chondromalacia of the lunate and/or ulna |
Perforation of the lunotriquetrum ligament | |
Class IIE | TFCC perforation and chondromalacia of the lunate and/or ulna |
Perforation of the lunotriquetrum ligament | |
Ulnocarpal arthritis |
Class I injuries are true traumatic tears and are subdivided into four basic types based on the pattern of injury. Type IA lesions involve the central avascular portion of the articular disk and are not suitable for suture repair. Arthroscopic management includes the debridement of a central tear to remove any symptomatic flaps. Type IB (ulnar avulsion) injuries occur when the ulnar side of the articular disk is avulsed from its insertion. These injuries may or may not be associated with a fracture to the ulnar styloid. Because these tears occur over in the region of a documented vascular supply, they are very amenable to arthroscopic repair by a number of techniques. Type IC injuries involve rupture of the volar attachment of the triangular fibrocartilage complex over the ulnar carpal ligaments. Type ID involves a tear of the radial attachment of the articular disk as well as the radioulnar ligament separate from the radius with or without a fracture of the radial sigmoid notch.
Class II lesions are considered degenerative tears of the triangular fibrocartilage complex and involve a central portion of the articular disk. These are stage A through E depending on the presence or absence of perforation to the triangular fibrocartilage complex, ulnar head and lunate chondromalacia, perforation of the lunotriquetral interosseous ligament, and degenerative arthritis of the radial ulnar joint. These lesions generally arise from ulna impaction and surgical management mostly consists of a variety of procedures to decrease the load across the ulnar side of the wrist, either arthroscopic or open management.
Diagnosis
Injuries to the triangular fibrocartilage complex commonly occur with extension and pronation of an axially loaded carpus. The most common mechanism occurs with a fall on an outstretched hand. Peripheral tears of the articular disk are frequently common athletic injuries, which occur in sports and require rapid twisting and loading of the ulnar side of the wrist such as golf or racket sports. Peripheral ulnar-sided tears of the articular disk may also be a common work injury. Patients often describe a mechanism of traction and torsion of the forearm which may occur with the use of a drill motor when the drill bit suddenly binds resulting in a twisting injury to the wrist.
Patients with symptoms of peripheral tears of the triangular fibrocartilage complex complain of a deep diffused aching across the ulnar side of the wrist. They may complain of pain with firm gripping as well as a clicking sensation with rotation of the forearm. They frequently complain of pain with resistance to forearm rotation such as twisting lids off jars or twisting a doorknob. Frequently, they may complain of generalized wrist weakness.
Patients with an ulnar-sided peripheral tear of the articular disk frequently describe point tenderness right at the prestyloid recess and point to that location. This pain may be accentuated by hypo-pronation or supination of the forearm. This pain may be further aggravated by passive anterior/posterior translation of the ulna in relation to the radius with the wrist in pronation and supination. Dorsal subluxation of the ulnar head in relation to the radius may be seen particularly if a large peripheral tear is present involving both the superficial and deep layers of the articular disk.
Several tests have been described that are used for the diagnosis of ulnar-sided wrist pain. The TFCC compression test is considered positive with axial loading of the articular disk with the wrist in ulnar deviation and results in significant pain. Araujo described the ulna impaction test which is considered to be positive when the wrist is positioned in ulnar deviation, hyperextension and axial load reproduces the ulnar-sided wrist pain. The piano key sign is frequently described for instability of the distal radioulnar joint, which can be seen with a peripheral tear of the articular disk. The test is positive if the distal ulna can be pressed volarly by dorsal thumb pressure in a pronated wrist as compared to the opposite side. In general, patients with a central tear of the articular disk hurt more over the ulnar head while patients with a peripheral tear present complaining about the prestyloid recess region.
Diagnostic Modalities
Patients who present with acute or chronic ulnar-sided wrist pain should be evaluated initially with standard anterior/posterior, lateral, and oblique radiographs of the wrist. It is important in the AP view to take the radiograph in neutral position to evaluate for ulnar variance. It is frequently helpful to take a fist compression view to evaluate for possible ulnar impaction which should be in the differential diagnosis. Radiographic signs of ulnar impaction include cystic changes on the medial side of the lunate (kissing lesion). These changes are indicated by excessive loading to the ulnar side of the wrist, which may require an ulnar shortening procedure. The distal radioulnar joint should also be evaluated for signs of radioulnar impingement, which must be differentiated from pain related to the triangular fibrocartilage complex. In addition, signs of acute or chronic injury to the ulnar styloid may be assessed on plain radiographs. Plain radiographs also are helpful to evaluate for signs of ulnar styloid abutment.
Triple injection arthrography was the gold standard in the past in diagnosing pathology of the triangular fibrocartilage complex [6]. However, ulnar-sided peripheral tears of the articular disk may be frequently missed by arthrography particularly in the chronic setting. This is secondary to chronic synovitis that develops over the peripheral tear blocking the flow of dye between the radial carpal and distal radial ulnar joint.
Several studies have evaluated the use of magnetic resonance imaging in diagnosing TFCC injuries [7–9]. Golimbu et al. and Skahen et al. both reported that the use of magnetic resonance imaging for detection of central and radial detachment of the articular disk with an accuracy of 95 % [7, 8]. Corso et al. in their study of ulnar-sided tears of the triangular fibrocartilage complex found sensitivity in only 76 % with magnetic resonance imaging [9]. Bednar reported his results of MR imaging and noted the sensitivity was 44 % with specificity set at 5 % for TFCC tears [5]. Fulcher and Poehling recommended the use of arthroscopy for definitive diagnosis and felt that MRI overstates some injuries of the TFCC while understating other TFCC pathology [10].
Studies comparing wrist arthroscopy with arthrography confirm that arthroscopy is the gold standard in detecting injuries to the triangular fibrocartilage complex [9]. Pederzini et al. compared MRI, arthrography, and arthroscopy on 11 patients with tears to the triangular fibrocartilage complex [9]. Utilizing arthroscopy as the gold standard, he reported 1 % sensitivity with MRI and arthrography and 80 % sensitivity for arthrography and 82 % sensitivity for MRI evaluation alone. Arthroscopy has a clear advantage of visualization of the articular disk under bright light and magnified conditions. The tension of the disk may be assessed by palpation with a probe. In most instances, a loss of tension will be detected to the articular disk when a peripheral tear is present. Frequently, synovitis has formed over the peripheral ulnar tear marking the site of pathology. Once the synovitis is debrided, the peripheral tear would be well visualized. Wrist arthroscopy is a useful adjunct and not only has the advantage of being sensitive and accurate to make the diagnosis but at the same sitting proceeding with definitive management.
Management
Indications
Patients who present with acute ulnar-sided wrist pain with normal radiographs and tenderness over the periphery of the TFCC, initial immobilization is a rule of thumb. Potentially small ulnar peripheral tears of the articular disk may heal from immobilization due to the vascular blood supply. Further diagnostic modalities are initiated after 2 or 3 months of immobilization when patients continue to be symptomatic or when an early diagnosis is important to the patient (professional athlete). MRI evaluation is certainly a common option, but the author prefers to proceed directly to wrist arthroscopy when the history and physical examination are classic for an injury to the triangular fibrocartilage complex and the patient does not improve with immobilization.
Indications for surgical intervention include persistent ulnar-sided wrist pain not relieved by conservative management for at least 3 months. Additional indications include symptomatic distal radial ulnar joint instability not improved by immobilization. It is also felt that a subluxation to the extensor carpi ulnaris tendon is usually associated with a peripheral tear to the articular disk.
Contraindications for surgical management are in those patients who are minimally symptomatic despite radiographic findings and patients with low physical demand who are medically not healthy enough for surgery. In addition, patients with significant degenerative changes either to the radial carpal or radial ulnar joint may be better managed by addressing the arthritic symptoms rather than an arthroscopic procedure.
Arthroscopic Technique
The wrist is suspended with 10 lb of traction in a traction tower (Fig. 6.1). The volar forearm and arm are well padded with towels so the skin does not come into contact with the tower itself. This will help prevent any potential burns from heat of the tower if it has been recently sterilized. The skin is incised with the tip of an 11 blade at the 3-4 portal and blunt dissection is continued with a hemostat to the level of the joint capsule. The arthroscope with a blunt trocar is introduced into the 3-4 portal and a working portal is made in the standard 6-R portal. Inflow may be provided through the 1-2 portal if a tear of the triangular fibrocartilage complex is suspected. In this manner, the inflow is out of the way during the arthroscopic repair to the TFCC complex. Alternatively, inflow may be provided through the arthroscope itself or through the needle in the 6-U portal.


Fig. 6.1
The wrist is suspended in a wrist traction tower (Acumed, Hillsboro, OR). The wrist is suspended in approximately 10–20° of flexion to allow easier entry of instrumentation into the radiocarpal space
It is always important to identify the exact location of the 6-R portal just distal to the articular disk with an 18-gauge needle inserted into the radial carpal space. The needle is viewed arthroscopically as it is being inserted. If ideal placement is confirmed, then the skin is incised and the 6-R portal is made. In this manner, there is no potential damage to the articular disk when making the 6-R portal. Cooney described the trampoline test in which there should be good tension to the articular disk when palpated with a probe inserted through the 6-R portal [11]. The articular disk will be lax to palpation and has a sunken appearance when a peripheral ulnar tear of the articular disk is present. Synovitis is frequently present marking the location of the peripheral tear which is debrided out to further expose the injury (Fig. 6.2).
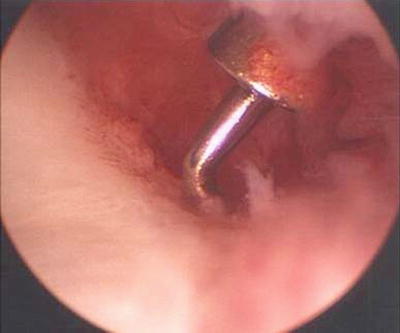
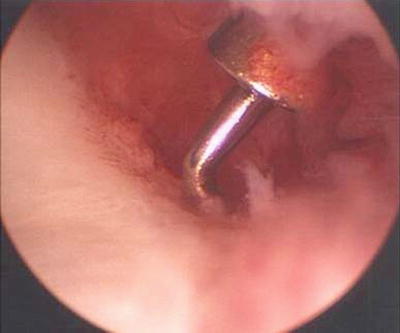
Fig. 6.2
Arthroscopic view with the arthroscope in the 3-4 portal showing a peripheral tear to the articular disk of the TFC in a right wrist. Note the proliferative synovitis about the tear
There are several arthroscopic techniques for repair of peripheral ulnar-sided tears of the articular disk. Indications for which type of repair varies from author to author. Each technique has its advantages and disadvantages. It is thought when a greater degree of instability of the distal radioulnar joint is present, arthroscopic repair back to bone will provide greater stability as compared to soft tissue repair alone.
Whipple Technique
Whipple et al. described the outside-in technique to reattach the articular disk back to the floor of the sixth compartment [12]. This is ideal for peripheral tears of the articular disk that arise dorsally. The advantage of this technique is that it is relatively simple and does not require any special instrumentation. It is particularly indicated in those patients that are point tender about the prestyloid recess area and have a minimal amount of instability to the distal radioulnar joint. The disadvantage of this procedure is that it does require an incision around the extensor carpi ulnaris tendon sheath, which has to be closed after the procedure. Potentially, there would be a risk for subluxation or instability to the extensor carpi ulnaris if the sheath is not fully closed or does not heal. In addition, patients may complain about irritation of the ECU tendon secondary to the suture knots.
In this technique, the arthroscope is introduced in the standard 3-4 portal. The 6-R portal is elongated approximately 12–15 mm in length along the radial border of the extensor carpi ulnaris tendon. The extensor retinaculum is sharply released along its radial side and the extensor carpi ulnaris tendon is retracted volarly. It is important to protect the articular branch of the dorsal sensory branch of the ulnar nerve as it crosses the incision in an attempt to decrease the risk of sympathetic dystrophy. A curved or straight 18-gauge needle is inserted through the floor of the extensor carpi ulnaris tendon sheath through the peripheral tear as visualized with the arthroscope in the radiocarpal space. Once the needle is identified, it is pulled back and then perforates through the articular disk (Fig. 6.3). It is important to insert the needle as perpendicular as possible to the articular disk. The suture may potentially pull through or shred the disk if it is placed too horizontal or shallow. A 2.0 monofilament suture is placed through the needle into the joint (Fig. 6.4). One trick to help get the suture started into the needle is to cut the plastic off the needle as close as possible. This makes it easier to thread the suture into the needle and into the joint. It is sometimes frustrating to fight the pressure of the fluid being injected through the needle as one is trying to insert the suture. Following insertion of the suture through the needle into the joint, a suture retriever is inserted through the floor of the extensor carpi ulnaris tendon sheath distal to the articular disk to grab the suture (Fig. 6.5). If a suture retriever is not available, a standard wrist arthroscopy grasper may work. Two or three sutures are placed in vertical fashion to close the tear (Figs. 6.6 and 6.7) The wrist is then taken out of traction, and the sutures are tied with the wrist in neutral position. A trick is to tie an arthroscopic slip knot to help slide the suture down against the tendon sheath of the extensor carpi ulnaris with tension. It is frequently difficult to slide the knot with the surgeon’s finger down into such a small hole and maintain good tension to the repair. It is very important to use dissolvable sutures so the knots of the sutures do not continue to irritate the tendon of the extensor carpi ulnaris. It is important to close the sheath of the extensor carpi ulnaris to limit the risk of instability to the tendon.










