Fig. 8.1
Palmer’s classification of TFCC injuries based on arthroscopic findings
Clinical Features
Clinical features vary with severity of the disease; the usual presenting symptom is chronic ulnar-sided wrist pain. The onset is usually insidious and progressive without any history of trauma. In early stages, pain is brought on or exacerbated with activity. Specifically, pain is exacerbated with movements that include power grip, ulnar deviation of the wrist and pronation and/or supination of the forearm. Some patients will complain of swelling over the ulnar side of the wrist and in advanced cases the pain is persistent and associated with decreased motion of the forearm and wrist.
Ulnar-sided tenderness to palpation can be elicited especially around the volar and dorsal aspects of the ulnar head, the lunate and triquetrum. A positive ulnar impaction test produces pain with passive full ulnar deviation of wrist. In order to differentiate ulnar impaction from other causes of ulnar-sided wrist pain it is necessary to provoke symptoms with physical maneuvers. Nakamura et al. described the ulnocarpal stress test in which the wrist is placed in maximal ulnar deviation, axially loaded and then the forearm is passively rotated through supination to pronation. If this causes pain then the test is positive [9]. Another test is the “press test” in which pain is reproduced by asking a seated patient to push off a chair using the affected wrist [10]. To test the lunatotriquetral ligament, the Regan shuck test or the Kleinman shear test should be performed [11].
Differential Diagnosis
It is important to differentiate ulnar abutment from other possible conditions. Pathology of the distal radioulnar joint such as arthritis or instability can be identified with pain on forearm rotation. Careful palpation and radiographic assessment is also needed to rule out other bony conditions such as pisotriquetral arthritis or hamate hook nonunions, soft tissue conditions like extensor carpi ulnar wrist tendonitis or subluxation, carpal ligamentous tears and traumatic TFCC tears also need to be taken into consideration. Lastly nerve pathology like neuritis of the dorsal cutaneous branch of the ulnar nerve must also be excluded.
Imaging
Standard posteroanterior (PA) and lateral radiographs of the wrist should be obtained. The shoulder should be abducted to 90°, the elbow flexed to 90° with the forearm pronated to obtain a neutral rotation wrist film. The PA of the wrist will show static positive ulnar variance if present. If standard films are negative, dynamic positive ulnar variance can be demonstrated with a pronated grip PA view of the wrist. A study of 22 patients with ulnar-sided wrist pain showed increase of ulnar variance of an average 2.5 mm with a pronated grip view [12]. In advanced cases, subchondral sclerosis and cystic changes are visualized within the ulnar side of the lunate, the triquetrum and the ulnar head. Radiographs must also be examined for widening of the lunotriquetral joint, carpal collapse and degenerative changes of the ulnocarpal or distal radioulnar joint.
Advanced imaging techniques may be helpful in some cases. Triple injection arthrogram is preferred over single injection to assess both the TFCC and lunatotriquetral ligaments. MR imaging with or without an arthrogram is beneficial for demonstrating integrity of the lunotriquetral ligament and TFCC. MR is particularly helpful in demonstration early stages of the disease with bony edema, cyst formation, and chondromalacia in the ulnocarpal joint [13].
Role of Arthroscopy
Arthroscopy allows confirmation of the diagnosis, staging of the disease, and the option to proceed with therapeutic procedures such as debridement or ulnar recession. Patients with a positive history, clinical exam and imaging that have failed nonoperative treatment of activity modification, NSAIDs, splinting and injection are candidates for intervention. Weiss et al. compared the effectiveness of triple injection arthrogram versus arthroscopy. They found that arthrography was 83 % specific, 56 % sensitive, and 60 % accurate when compared to arthroscopy [14]. Wrist arthroscopy has been shown to be more accurate in assessing the ligaments, articular surfaces and TFCC than arthrography [15].
Management of Ulnar Abutment
The goal of management is relief of symptoms and prevention of progression of ulnocarpal degeneration. Debridement of a degenerate TFCC will be helpful in the short term, but in the presence of uncorrected ulnocarpal loading is not likely to produce long-lasting relief [16]. Relieving the increased ulnar pressure is the essence of management and can be achieved by either shortening the ulna or recession of the distal articular surface of the ulna. The latter can be achieved arthroscopically. Debridement of the central portion of the TFCC and the resection of the distal ulna to subchondral bone can result in significant unloading of the ulnocarpal joint in a cadaver model [17].
Treatment of TFCC Wear and Perforation
In early stages of ulnar abutment, pathology is confined to the central avascular portion of the TFCC [18]. These lesions have no healing potential and should be treated with arthroscopic debridement rather than attempt to repair [19].
When debriding the TFCC, the defect should be enlarged until fresh borders of the tear are created. It is imperative to leave the dorsal and volar radioulnar ligaments intact. If not, this will alter the load bearing at the distal radioulnar joint and the stabilizing effect at the TFCC [20]. The precise mechanism of symptomatic relief achieved by enlarging the tear is not clear, and is likely by prevention of entrapment of flaps of the TFCC during impaction loading of the ulnocarpal joint.
Arthroscopic Technique
The 3-4 and 6-R arthroscopic portals are utilized for management of ulnocarpal impaction. The wrist is placed in traction with finger traps applied through the index and middle finger using an overhead boom or specialized traction device. The wrist joint is then insufflated with fluid. A routine diagnostic scope should be performed using the 3-4 portal with outflow through the 6R portal (Fig. 8.2). A probe is introduced by developing the 6R portal in order to probe the TFCC and determine the location and extent of the tear. It is not uncommon to encounter significant synovitis on the ulnar side of the joint requiring initial debridement with an arthroscopic shaver prior to examination with the probe. The articular surfaces of the lunate and triquetrum are examined carefully for any loose chondral flaps that should be debrided. The presence of a TFCC central tear with signs of chondromalacia of the lunate and possibly the ulnar head and triquetrum is classified as a Palmar IIC. If there is LTIL laxity with a TFCC tear this transitions the diagnosis to a Palmar IID or IIE.
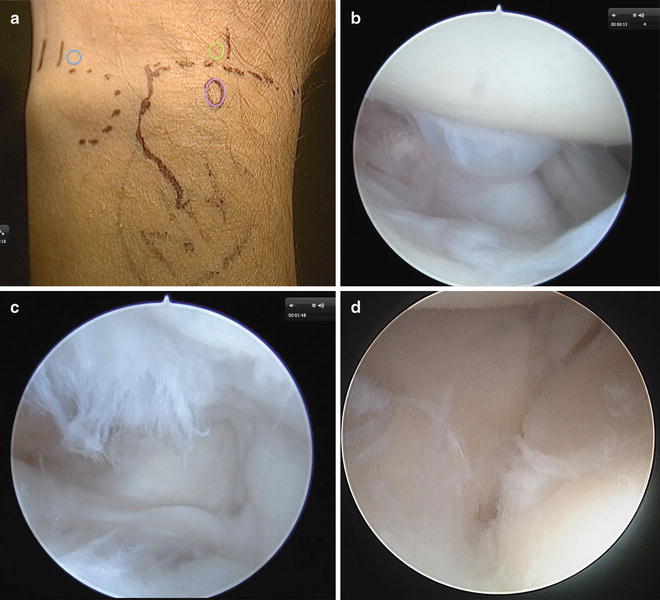
Fig. 8.2
Arthroscopic wafer procedure. (a) Portal placement for the wafer procedure mainly uses the 6R portal (blue circle) and 3/4 portal (green oval) with Listers tubercle denoted with a purple oval. (b) Once the scope has been introduced and a routine scope has been preformed, the radial side of the wrist will be normal without any signs of pathology pertaining to ulnar abutment. (c) The ulnar side of the radiocarpal joint shows a central tear and chondromalacia of the ulnar half of the lunate. (d) Midcarpal view shows lunotriquetral instability
Radial and ulnar midcarpal portals are then used to assess the stability of the lunotriquetral ligament. A shuck test should be used intraoperatively to test the lunatotriquetral laxity.
Once the disease has been staged, attention is turned to debridement of the ulnocarpal joint. Large flaps of the TFCC can be debrided with a curved punch and the edges of the tear are debrided and smoothened with a toothed powered resector inserted through the 6R portal.
Care is taken to leave the dorsal and palmar radioulnar ligament and the foveal attachment of the TFCC intact. Debridement of the central portion of the TFCC can provide temporary symptomatic relief but does not address the underlying problems of ulnocarpal abutment. Decompression of the ulnocarpal joint in the presence of ulnar positive variance is also of benefit in the management of acute traumatic TFCC tears (Palmer, type IA) as debridement alone in this scenario is associated with poorer results [21]. It is our recommendation that isolated debridement should be reserved for patients with Palmer IA tears without positive ulnar variance. It has been shown that TFCC defects, both acute and chronic that are addressed with debridement and arthroscopic wafer were satisfied with their outcome [16]. Also, Palmar reported a favorable results at 2-year follow-up with the arthroscopic wafer procedure performed in patients with Palmar IIC TFCC pathology [18].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








