Lower Limb
ANATOMY
The lower limb spans the head of the femur to the toes. The leg lies between knee joint and ankle joint. Structures of the thigh are referred to as “femoral,” from Latin femur: “thigh,” such as fascia lata femoris: “broad fascia of the thigh,” and os femoris: “bone of the thigh,” or simply “femur.” Because two bones occupy the leg, its structures are referred to as “crural,” from Latin crus: “shank, leg,” such as crural fascia.
Unlike the hip, which commands its own treatise, the knee is difficult to extricate from the lower limb, save by an arthroscope (cf. Sports chapter).
The patella is conferred autonomy due to its size and functional importance. Hence, the term “ligamentum patellæ” when convention dictates “quadriceps tendon,” since the patella is lodged in this muscle as a sesamoid. The patella has a proximal base and a distal apex, referred to as superior and inferior poles. The anatomic terms aid understanding why children complain of pain rarely at the broad end (base) but frequently at the pointed end (apex), at which stress is concentrated. Anatomic terminology similarly aids remembering that the site of attachment of the lateral collateral ligament, known as fibular collateral ligament, differs from that of the medial collateral ligament, known as tibial collateral ligament.
Like the femur at the knee, the tibia has two condyles, which by being less rounded are less distinct. The raised space surrendered between the condyles for the cruciate ligaments is the “intercondylar eminence,” commonly referred to as “tibial spine” due to its sharp terminus. Like the proximal femur, with its trochanters, the proximal tibia has an apophysis termed “tubercle.” Unlike the femur, tibial apophysitis is common during growth.
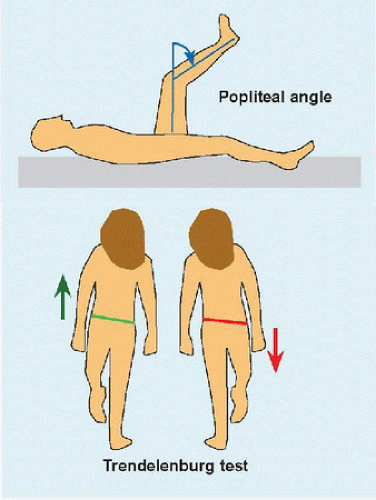
Knee angle is defined between thigh and leg, or between femur and tibia. Popliteal angle (Latin poples: “ham, hollow of the knee”) specifies the angle subtended by the leg relative to thigh in the sagittal plane [C], where it is a measure of “hamstring” tension. Full extension is defined as 0 degree, while hyperextension is defined as negative.
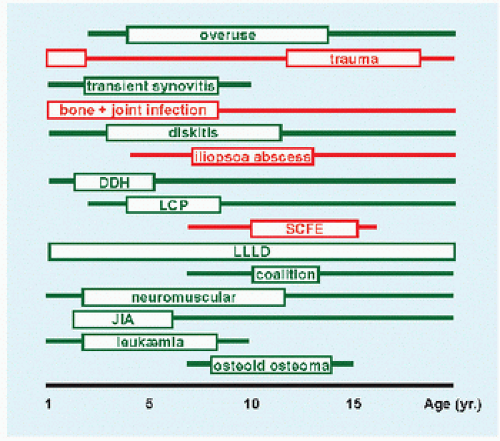
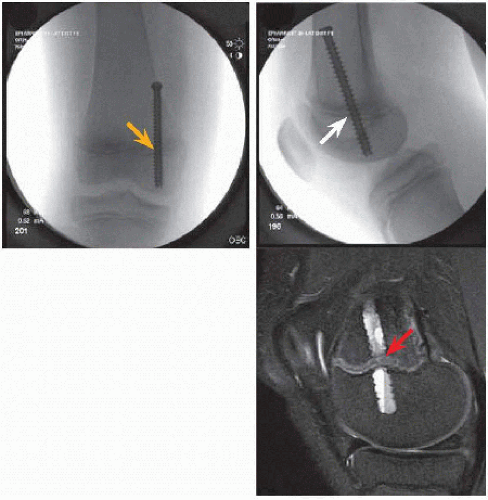
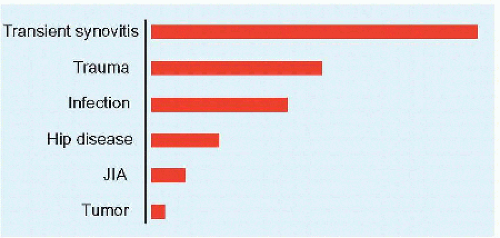 A Causes of limp by frequency Infection includes bone and joint, abscess, and diskitis. Hip disease excludes infection. |
LIMP
A limp signifies abnormal gait, which may be due to pain (conscious or subconscious), deformity, or neuromuscular imbalance. The limping child need not be a diagnostic “black box.” It requires a thorough history and physical examination, which may be supplemented by laboratory and imaging studies. Transient synovitis is the most common cause [A]. The condition may be divided according to age and urgency. Different causes occur with different frequencies in different age groups [B]. Some are characteristic of certain ages (e.g., slipped capital femoral epiphysis circa puberty), while others are broadly distributed (e.g., lower limb length discrepancy). The varying causes may be divided into those that require urgent treatment (e.g., hip pyarthritis) and those that may be managed electively (e.g., developmental dysplasia of the hip). The hip dominates anatomically [D].
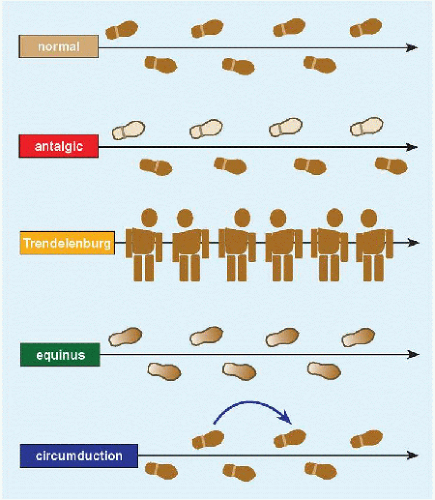
Gait Antalgic gait is defined by a shortened stance phase, of which the extreme is a refusal to walk [E]. A common theme in hip deformities producing limp is a Trendelenburg gait [C]. This results from a shift of the body over the affected hip in order to reduce the moment arm exerted on weak abductor muscles, which aids them in maintaining a horizontal pelvis during stance phase. In milder deformities, the gait may be apparent only after several cycles and may give way to pain as the hip abductors increasingly fatigue. This may be distinguished by its more lateral location from painful hip disorders, in which the pain is anterior in the region of the groin. Neuromuscular patients may exhibit an equinus gait, such as a hemiplegic who walks toe-toe. Equinus may drive the knee into recurvatum to plant the foot flat. Circumduction gait is characterized by incomplete knee flexion, actively (e.g., due to pain) or passively (e.g., due to contracture), which functionally lengthens the limb requiring swinging around the direction of walking to clear the ground.
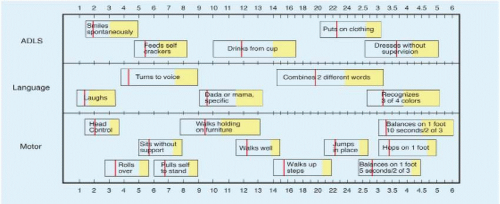
Evaluation Age is the single most important discriminator of disease. Obtain a complete history. Is this acute, intermittent, or chronic? Are there associated symptoms (e.g., bruisability on leukæmia)? Is the limp local or a manifestation of a generalized condition (e.g., preceding illness)? Ask about milestones: delay may be an early tip-off of subtle neuromuscular disease [F]. Does the child complain of the limp? Long-standing, intermittent, milder pain may be suppressed in a child’s consciousness producing the so-called “painless” limp (e.g., established Legg-Calvé-Perthes disease).
Look at the whole child. Does she or he seem in distress (which may differentiate synovitis from infection), suggesting an urgent presentation? Are the upper limbs (e.g., hemiplegia) or back (e.g., diskitis) affected? Before examining where it hurts, go to the other side to gain the child’s confidence. The physical examination should be performed in both supine and prone positions. The supine position may show hip obligate lateral rotation with flexion as seen in slipped capital femoral epiphysis. The prone position has the distinct advantage of allowing uncoupling of the knee from the hip, which may masquerade one for the other. The knee may be ranged from extension to flexion without moving the hip. In the supine position, moving the knee requires flexion of the hip, making it difficult at times to tell which joint is the offender. In addition, as in examination for torsion, the prone position allows simultaneous comparison of hip rotation (especially medial), which is the most sensitive to disease. Finally, the prone position will reveal a hip flexion contracture that may be concealed by lumbar hyperlordosis without the physician manipulating the child. No room is big enough to evaluate gait in detail. In addition, running amplifies gait disturbances and impedes compensatory mechanisms.
Management This is in accordance with condition, of which the different types are discussed independently elsewhere. Röntgenogrammes are readily available, low morbidity, inexpensive, and useful for general screening. Ultrasonography is noninvasive. By contrast, needle aspiration is invasive and stressful to child and parent; however, it is of high diagnostic value. Do not let timidity or logistics delay or dissuade—the emergency setting offers the best opportunity. Specialized imaging focuses and elucidates, such as scintigraphy in radio negative case where occult fracture is
suspected. Obtain laboratory tests judiciously. C-reactive protein is more specific and sensitive for infection than is leukocyte count. Observation is an acceptable and prudent form of management. Before requesting a complex test, which may require anæsthesia or may be expensive, evaluate the child on another day if the presentation is not urgent. A final diagnosis may elude the most thorough investigator in up to 25% of cases.
suspected. Obtain laboratory tests judiciously. C-reactive protein is more specific and sensitive for infection than is leukocyte count. Observation is an acceptable and prudent form of management. Before requesting a complex test, which may require anæsthesia or may be expensive, evaluate the child on another day if the presentation is not urgent. A final diagnosis may elude the most thorough investigator in up to 25% of cases.
LEG ACHES
Leg aches are “growing pains.” This may be explained as overuse in a child who lacks judgment to avoid repetitive injury and lacks consequence when injured (due to rapid recovery). Other mechanisms implicated include rapid, episodic skeletal growth stretching surrounding soft tissues, increasing body weight, participation in sports at higher levels with escalating expectations, and developing body mechanics. One-third of children experience leg aches, in addition to headaches and stomach aches. All of these may be stressful to the family but are physiologically benign, resolving without sequelæ. Extensive evaluation, including MRI of the brain, gastrointestinal contrast study, and multiple röntgenogrammes of the lower limbs, is negative. Recognize and reassure.
Evaluation Leg aches usually affect both legs, though one side may predominate [A]. If they produce limp, it is intermittent. They are worst at the end of a busy day or at night, interfering with falling asleep but not awakening from sleep. Long duration presents a paradox: while trying for a family, this lowers the physician’s concern (bad things do not linger without causing further trouble). They are not associated with other symptoms. They are poorly localized and may migrate from part to part within a limb or from side to side. This is consistent with benignity, but also calls for a broad physical examination. There are no “hard” objective signs, such as deformity, stiffness, swelling, discoloration.
Management Establish this diagnosis of exclusion, in order not to request unnecessary tests or tests that yield equivocal results, which may alarm a family and trigger further testing.
TORSION
This presents the greatest disparity between familial concern and disease.
Nomenclature
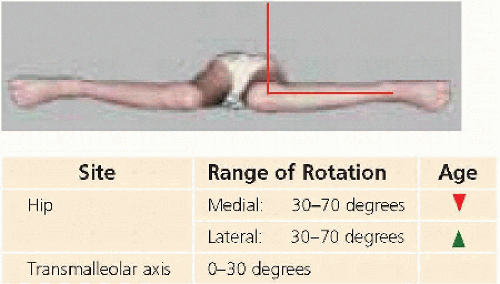
Version refers to normal axial rotation of a long bone. In the femur, this is the angle subtended between the neck and condyles, normally anteriorward 30 degrees at birth declining to 12 degrees at maturity. In the tibia, it is measured as the transmalleolar axis, with the knee as a neutral
reference: normal is 5 degrees at birth increasing to 15 degrees lateralward at maturity.
reference: normal is 5 degrees at birth increasing to 15 degrees lateralward at maturity.
| ||||||||||||||||||||||||||||||
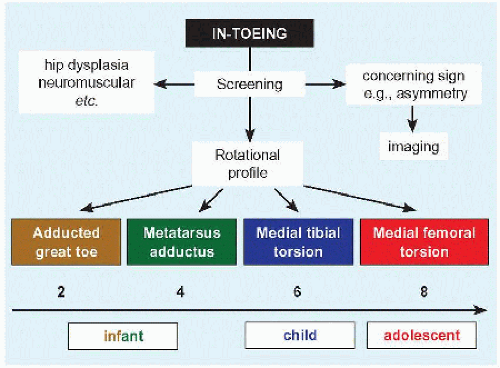 F Algorithm for in-toeing Numbers indicate age in years by which component of in-toeing resolves spontaneously in most cases. Boxes below abscissa indicated period of treatment if indicated. |
Torsion refers to abnormal version, > or < 2 standard deviations from the mean. For example, in the proximal femur, “antetorsion” is preferable to “excessive anteversion.” “Retrotorsion” signifies neck inclination 15 degrees to 0 degree. Retroversion is abnormal per se.
Rotation may be described as medial and lateral, or internal and external. The latter distinguishes rotation as a movement.
Development
In the fetus, the lower limb rotates medialward to bring the apex of the knee anterior and the hallux medial. With growth, the lower limb unwinds lateralward, with declining femoral anteversion and increasing transmalleolar axis. Thus, in-toeing tends to resolve with growth, whereas out-toeing may worsen.
Evaluation
History This is essential to acknowledge the concerns of the family.
Physical examination Determine the rotational profile, which has the following components.
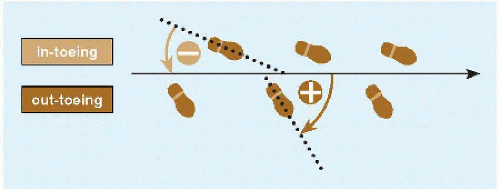
FOOT PROGRESSION ANGLE This is the angular difference between the axis of the foot and line of progression walking [A].
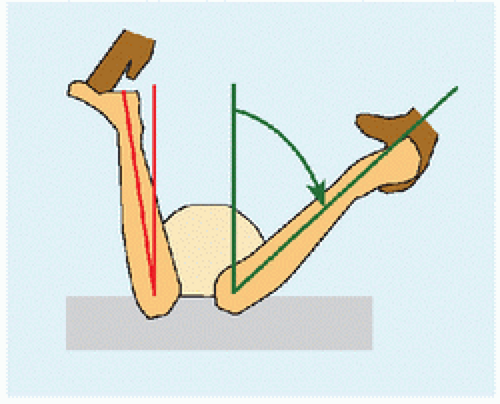
FEMORAL VERSION Measure hip rotation prone [B]. Significant asymmetry may be a sign of focal disease (e.g., slipped capital femoral epiphysis). Identify the midpoint between medial and lateral rotation, a measure of resting rotation. Normal medial rotation is <70 degrees; >90 degrees, which requires moving the limb off the side of the table, is considered severe [C]. A child with femoral antetorsion sits in a W position. The patellæ “squint” or “kiss” in the standing position. Running is characterized by an “eggbeater” pattern, as the legs flip out during swing phase.
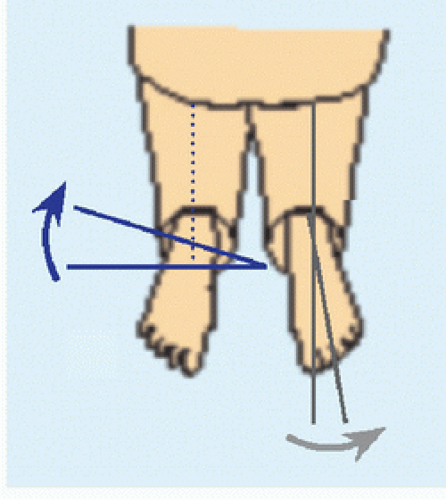
ANGLE OF TIBIAL ROTATION This may be determined by thigh-foot angle or transmalleolar axis [D]. Thigh-foot angle is a measure of both leg (ankle) and foot (subtalar) rotation, whereas transmalleolar axis isolates the leg. In an infant, thigh-foot angle has wide variation due to ligamentous laxity: minimize this by guiding the foot to its neutral position rather than manipulating it into position. In an older child, it may be compared with transmalleolar axis to estimate contribution of hind foot rotation.
Foot Examine the lateral border of the foot. This may be convex in metatarsus adductus, thereby producing in-toeing. It may be concave in forefoot abductus, as in flatfoot or overcorrected clubfoot. An adducted hallux, dynamic or static, may give the appearance of in-toeing.
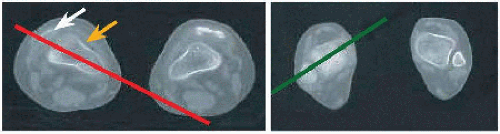
Imaging Consider imaging for concerning sign, such as asymmetry of hip rotation, or as part of operative planning. For the former, start with screening röntgenogrammes. For the latter, CT measures rotation [E].
Management The natural history of torsion is unaffected by manipulative therapy or bracing. Sitting in the W position is OK. Twister cables are not OK. Each component of torsion resolves spontaneously in the majority of patients with growth over the first decade [F]. In the young child, it is difficult to determine the functional impact of torsion, for example, frequent falling is more likely due to judgment and development of gait mechanics than to torsion, unless severe. In fact, medial torsion may be advantageous in rectifying the course of tibialis posterior and poising the subtalar joint to lock, thereby expediting push-off. Conversely, increasing lateral rotation reduces lever arm of the foot, thereby weakening push-off. Appearance is determined by the family and often is a significant cause for consultation.
There is no evidence that persistent femoral antetorsion accounts for long-term morbidity such as osteoarthritis. Femoral retroversion is abnormal and is associated with slipped capital femoral epiphysis and femoroacetabular impingement.
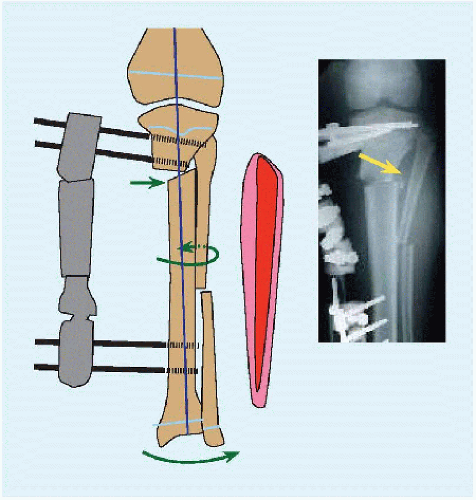
Only operation can change long bone torsion. This is indicated in < 1% of patients, and after 8 years of age. Torsion must be severe, clearly a cause of dysfunction, and natural history must be allowed to complete
its course. This is most likely in opposing or “miserable” malalignment [E], which is deleterious to the patellofemoral articulation, accounting for pain and patellar instability.
its course. This is most likely in opposing or “miserable” malalignment [E], which is deleterious to the patellofemoral articulation, accounting for pain and patellar instability.
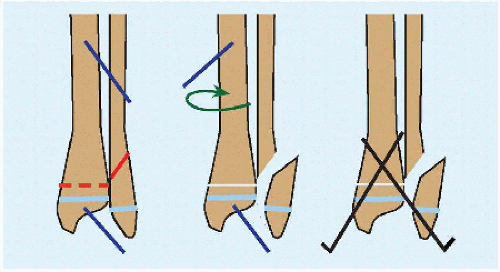
FEMORAL OSTEOTOMY This may be performed proximal or distal. Proximal incision may be covered more readily by clothing. Intertrochanteric osteotomy allows level proximal to trochanter minor, which heals readily and takes advantage of iliopsoas to add compression. Operation in the prone position, while requiring familiarity (“upside down”), allows comparison of both lower limbs for symmetry. Use a high angle plate (120 to 130 degrees) with longest blade into the head of the femur. This will provide an internal strut in the neck as protection against future osteoporosis.
TIBIAL OSTEOTOMY This is performed proximal to the tibial tubercle to correct patellofemoral malalignment. Distal metaphysial osteotomy is easier [G]. Cut the fibula for severe deformity. Add fasciotomy of the anterior crural muscle compartment to reduce risk of compartment syndrome. Plate fixation forgoes cast. Wire fixation allows more distal osteotomy for healing, and implant removal in clinic.
GENU VALGUM AND GENU VARUM
Anatomic description of angulation at a joint or fracture addresses the distal skeletal element. Genu valgum refers to pointing of the leg away from the midline, or apex medial angulation of the knee, in the coronal plane. Genu varum is the opposite. Genu valgum is known as “knockknee,” due to overlap of the joints during walking. Genu varum is known as “bowlegs,” after the arc formed by the lower limb.
Evaluation
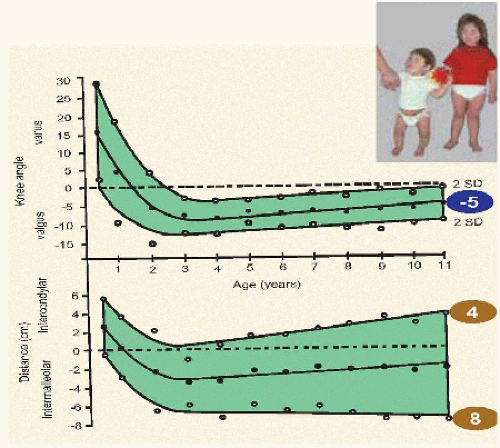
There is a normal evolution with age, and a normal range, of knee shape [A]. Knee shape may be measured as an angle or indirectly by distance between the ankles (genu valgum) or knees (genu varum).
History Is this acute (e.g., after fracture) or chronic (e.g., in rickets)? Does it disturb the child, such as pain or limp, or is it primarily a parental concern?
Physical examination Look at the entire child: is this focal, regional, or part of a generalized condition [B]? Short stature is common in rickets and various syndromes, which also may be characterized by other deformities, cutaneous stigmata, or dysmorphic features. Is it symmetric? Asymmetric deformity is likely morbid and not a physiologic variant. Determine the rotational profile, and neutralize this to isolate the coronal plane. Measure knee angulation with the patellæ pointing straight forward, by turning the hips as necessary. Most infants referred for genu varum have medial tibial torsion instead. In order to compensate for in-toeing, such children rotate the hips lateralward, presenting an oblique view of the knee. This will display a normal bend as the knee flexes during walking, which is interpreted as bowing by an observer who assumes an anteroposterior view of the knee. A goniometer aids angular measurement. Intermalleolar and intercondylar distance may be an easier measurement. Obesity influences measurements. Examine the child supine (static), as well as standing and walking (dynamic), which may expose soft tissue laxity.
Laboratory analysis This is indicated for a metabolic disorder, such as rickets.
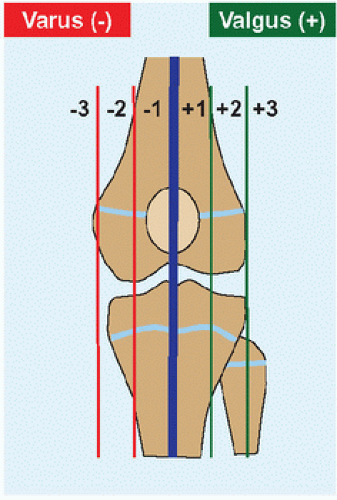
Imaging Röntgenogrammes are indicated if disease is suspected. Weight-bearing views simulate the functional position. Educate the technician to obtain a relaxed view with the feet or knees together. Do not distort the image by forcing the limbs together. Include hips to ankles, in order to view mechanical as well as anatomic axes [C]. Mechanical axis identifies deformity: in genu valgum, the axis passes lateral to the knee or medial to the ankle, and genu varum is characterized by the reverse. Anatomic axis identifies site of deformity, for
example, hypoplasia of lateral condyle of the femur producing genu valgum, or growth disturbance of medial condyle of the tibia producing genu varum. Coronal deformity also may be assessed by noting through which zone of the knee the mechanical axis travels [D]. Eliminate anisomelia, so that the child does not bend the knee, by a block under the foot of the short limb. What is the quality of bone? Is deformity diffuse or focal? Are the physis normal? Is there evidence of previous injury or disease? Focus the assessment with CT or MRI as indicated, to provide greater detail and for operative planning. Consider obtaining serial photographs.
example, hypoplasia of lateral condyle of the femur producing genu valgum, or growth disturbance of medial condyle of the tibia producing genu varum. Coronal deformity also may be assessed by noting through which zone of the knee the mechanical axis travels [D]. Eliminate anisomelia, so that the child does not bend the knee, by a block under the foot of the short limb. What is the quality of bone? Is deformity diffuse or focal? Are the physis normal? Is there evidence of previous injury or disease? Focus the assessment with CT or MRI as indicated, to provide greater detail and for operative planning. Consider obtaining serial photographs.
| |||||||||||||||||||||
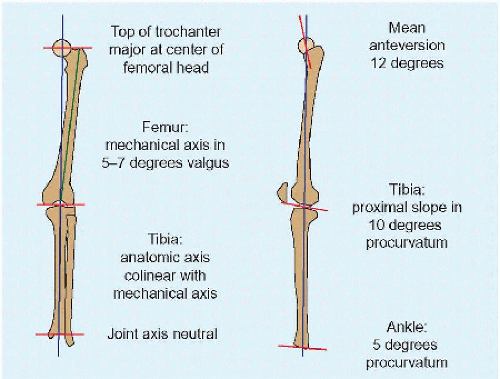 C Mechanical and anatomic axes of the lower limb Mechanical axis passes through joint centers, a measure of bones in combination. Anatomic axis is bone centered. |
Management
Treat the primary disorder first in generalized conditions, for example, vitamin D for rickets (cf. Syndromes chapter). Treat the primary musculoskeletal cause of knee deformity as indicated, for example, Blount disease (q.v.). For physiologic knee (mal)alignment, consider natural history during growth. Because children are maximally knock-kneed at 3 years and stabilize to mild knock-knees toward the end of the first decade, that is the time to intervene. Management earlier consists of education and reassurance. Because children become maximally knock-kneed at 3 years never to return to bowlegs, bowlegs at this age are abnormal and should be treated.
Like torsion, nothing influences natural history of genu valgum or genu varum except surgery. Determine the site of deformity by complete imaging. Harness the physis to guide growth: tether the medial physis in genu valgum and the lateral in genu varum, until correction, at which point remove the tether. Temporary hemiphysiodesis may be achieved by staples, plate, or transphysial screw [E]. Staples are the original. Early bending failure under force of growth has been addressed by corner reinforcement. They may dislodge due to smoothness of the tines. Plate and screws are more stable than staples, and span the physis. Screws may be placed percutaneously, are most stable, but are transphysial; however, removal after correction has not been associated with permanent growth disturbance. This approach is low morbidity, ambulatory, and predictable. For angular correction, remove implants within 2 years, before a physis gives up growth completely.
Deformity in the mature child, in whom growth modulation is not possible, or deformity that is not focal or uniplanar, occurring in the setting of broader complex deformity such as limb length discrepancy, requires more powerful reconstruction. Plan an osteotomy, including making cutouts or with graphics that allow operative simulation. The closer the osteotomy to the site of deformity, the less the requirement for translation to compensate for distance away from the center of rotation. Be prepared to perform an osteotomy at more than one level. Primary bone disease can deform the entire structure. Plan the fixation, internal or external, and location. External fixators are more potent in allowing three-dimensional correction. They enable gradual correction, which reduces the need for reconstruction of, and injury to, surrounding soft tissues. They are more forgiving because they may be manipulated after operation.
BLOUNT DISEASE
Blount called this “tibia vara.” It represents a growth disturbance of the posteromedial proximal physis of the tibia. The growing tibia spirals into varus (medial tether) as well as medial rotation and procurvatum (posterior tether), thereby forming a complex multiplanar deformity. While the condition originates in the tibia, where signs are most striking, it also may involve the distal femur.
Cause
Familial clustering suggests a genetic predisposition. Race is confusing: it has been reported most in Black Americans [A] and Scandinavians, with a worse prognosis in the former. A mechanical cause is suggested by association with early walking and obesity: a heavy child whose physiologic genu varum is greater the earlier is walking and who does not fully extend the knees during gait concentrates load at the posteromedial physis of the proximal tibia. Compression retards or arrests growth according to the Hueter-Volkmann principle. Wide gait due to obesity increases the varus moment at the knee, squeezing the medial physis. Asymmetric or unilateral disease suggests that other, local factors may play a rôle.
Evaluation
Classification Like idiopathic scoliosis, Blount disease may be divided by age into infantile (<4 years), juvenile (4 to 10 years), and adolescent (>10 years). Severity is inversely proportional to age of onset.
The condition also has been classified according to progressive physial irregularity [B]. However, this system has high interobserver variability, in part due to variable ossification over a wide age range and to segmentation of a continuous process. As a result, it may be simplified into I-III and IV-VI, based upon likelihood of spontaneous recovery and bridge formation, which impacts operation and outcomes.
Natural history The most important predictor of severity and poor outcomes is age of onset: early in growth, the more cartilaginous proximal tibia is more fragile. Knee degeneration is proportional to severity of deformity. Body weight is an independent predictor of outcome, with body mass index >40 kg/m2 being a critical value for severity.
History Ask about walking age. Also enquire about nutrition and exercise, as well as efforts at weight reduction.
Physical examination It often is difficult to distinguish physiologic varus from Blount disease before 2 years of age: bring such patients back at 3 years of age. Calculate body mass index. Measure the intercondylar distance standing. Examine the knee dynamically: is there lateral thrust at the knee during walking? The lateral soft tissue become so attenuated over time that they are unable to support fully the knee during stance phase, allowing the tibia to be displaced lateralward. The deformity may be exaggerated, associated with a clunk, by varus stress of the attenuated lateral soft tissues. Determine the rotational profile of the tibia, which produces in-toeing and must be addressed by osteotomy.
Imaging Obtain röntgenogrammes standing with the ankles together and the patellæ forward to obtain orthogonal views of the knees. Alert the technician to allow the feet to turn inward as much as necessary. Projection is critical to isolating the coronal plane. Röntgenogrammes may be challenging in the adolescent due to obesity and size, including getting
the width of the knees on a single view. The earliest sign is varus with metaphysial beaking [A]. Growth disturbance of the proximal physis of the tibia may be characterized according to the Langenskiöld classification. In long-standing disease, a significant (i.e., worthy of inclusion as part of surgical correction) proportion of the coronal deformity in adolescent presentation arises from the distal femur.
the width of the knees on a single view. The earliest sign is varus with metaphysial beaking [A]. Growth disturbance of the proximal physis of the tibia may be characterized according to the Langenskiöld classification. In long-standing disease, a significant (i.e., worthy of inclusion as part of surgical correction) proportion of the coronal deformity in adolescent presentation arises from the distal femur.
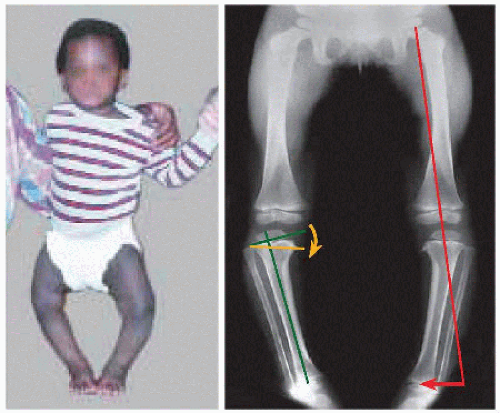 A Infantile tibia vara Mechanical axis misses the ankle laterally (red). Beaking of medial metaphysis indicates growth disturbance. Its effect is measured as the metaphysial-diaphysial angle. |
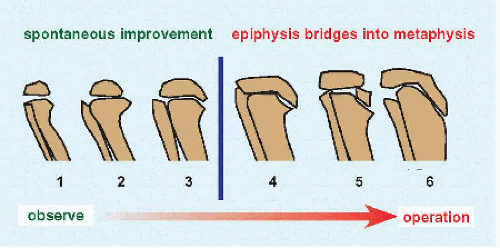 B Langenskiöld classification of Blount disease This classification is commonly used but sometimes difficult to apply. |
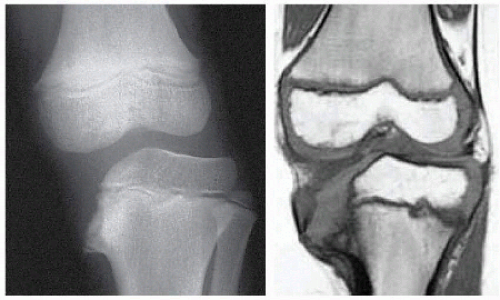 C MRI in Blount disease The medial condyle, absent on röntgenogramme, is visible on MRI, where depression explains medial subluxation of the femur. |
METAPHYSIAL-DIAPHYSIAL ANGLE This is the most established and useful measurement, formed by a line drawn through the metaphysis and one drawn orthogonal to the anatomic axis of the tibia in the coronal plane [A]. Substitute the axis of the fibula if the tibia is too deformed. In the incompletely ossified skeleton, a critical value is >15 degrees.
Arthrography outlines articular surfaces, often showing development of the medial condyle of the tibia invisible to röntgenogrammes because of a delay in ossification. MRI gives details of delayed ossification and deformation; articular changes, such as medial meniscal hypertrophy; and physial changes, such as bridge formation [C].
Management
Do not forget the child: make sure a specialist is in charge of weight control. Orthopædic management is observation or surgical. Initially observe Langenskiöld I-III, as many improve spontaneously.
Osteotomy (infantile) Consider realignment osteotomy of the proximal tibia at 3 years of age [D]. Include osteotomy of the fibula distal to its proximal third to reduce risk of common fibular nerve injury. Factors associated with recurrence of deformity after operation include the following:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree