Physical Examination
The neural examination includes:
Cognition. Cognitive function is essential to evaluation, management, and outcomes. For example, it may be difficult to determine pain in a cognitively impaired child with cerebral palsy.
Motor function. Assess strength manually and against body weight. In addition to individual muscle groups, a functional assessment is based upon standing and walking ability: standing for demonstration, standing to assist transfer, walking at home, and walking in the community. For walkers, determine total distance as a general measure of function. Assistive devices are not limiting but liberating.
Sensory function. Altered sensation may be direct, due to neural loss, for example, spina bifida, or indirect, due to cognitive loss.
Special signs, for example, a child using the hands to “walk up” the anterior legs and thighs in order to rise from a seated position in the setting of muscle weakness. Divide tone into normal, reduced (hypotone), or increased (hypertone).
Gait Evaluate by observation (cf. Lower Limb chapter). Gait is divided into stance and swing phases, which overlap for 20% of the normal cycle. Stability during single-limb stance can be limited by cognition, balance, proprioception, coordination, standing posture, bony deformity, contractures, and weakness. Without stability in stance, it is impossible to develop an effective gait pattern. Each swing phase requires clearance of the off-loaded foot to preposition that foot in terminal swing. Ankle equinus, weakness in dorsiflexors, and cospasticity are examples that will prevent clearance and prepositioning and lead to an ineffective gait, one with inadequate stride length, poor cadence, or otherwise biomechanically impaired and energy inefficient. Gait also may be assessed in a laboratory, including instrumented motion analysis, dynamic electromyography, pedobarography, and energy consumption test. Include walking and running, which as a stress test will amplify deficit, for example, asymmetry of the limbs in hemiplegia.
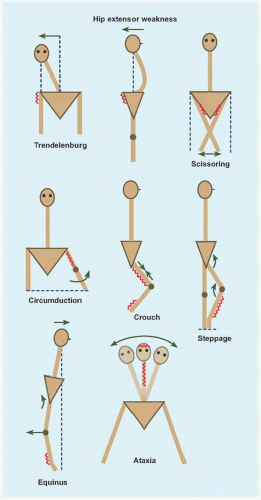
There are several morbid gaits [E].
HIP ABDUCTOR WEAKNESS This produces a Trendelenburg gait, which is characterized by shifting of the center of mass over the affected joint in stance to eliminate the moment arm. Because the patient has the tendency to fall away from the weak limb in stance, a compensatory mechanism is to raise the walking velocity, thereby reducing time for the effect of gravity, for example, advanced hip deformity.
HIP EXTENSION WEAKNESS Walking slows to reduce forward momentum. Lumbar lordosis increases to move center of mass posteriorward. Knee flexion decreases to limit hip flexion, for example, muscular dystrophy.
SCISSORING Adductor spasticity slows walking velocity and narrows the base of stability, for example, diplegic cerebral palsy.
QUADRICEPS WEAKNESS This reduces knee control and is the principal determinant of walking. Body weight flexes the knee, which is counteracted by hip extension, plantar flexion, and locking of the knee in extension. Additionally, the limb may be rotated lateralward to move the force vector medialward away from the sagittal plane, for example, spina bifida.
CIRCUMDUCTION GAIT Hamstring weakness, or quadriceps contracture or spasticity, reduces knee flexion, which is a major hindrance during swing. The limb is functionally lengthened, necessitating that it be swung outward for the foot to clear the ground.
CROUCHED GAIT This may be compensatory to reduced hip extension, due to knee flexion contracture, or a result of triceps suræ weakness. The gait cycle is shortened, there is forward trunk lean to reduce demand on quadriceps, and energy consumption increases, for example, overlengthening of tendo Achillis.
STEPPAGE GAIT Anterior crural muscle weakness is compensated for by increasing hip and knee flexion for swing phase toe clearance.
EQUINUS GAIT Reduced ankle flexion leads to a toe-toe gait, concentrating force at the forefoot during stance. There is reduced flexion or extreme hyperextension of the knee. In the neuromuscular patient, with compromised proximal muscle strength and control, forward translation of the center of mass reduces the effective base of support, thereby reducing stride length, for example, muscular dystrophy.
HINDFOOT VARUS This concentrates force over the lateral border of the foot during stance, for example, Charcot-Marie-Tooth disease.
ATAXIC GAIT Greek (α-: “not,” τα§ιζ: “precise arrangement”). This is a sign of central nervous disease, for example, in the cerebellum. It is characterized by a broad base, short stride, and titubation due to impaired balance.
The neuromuscular patient must balance benefits against energy consumption of walking. Speed declines first, to maintain energy cost per time. However, energy cost per distance increases: most patients will select a wheelchair for mobility once this exceeds thrice the normal.
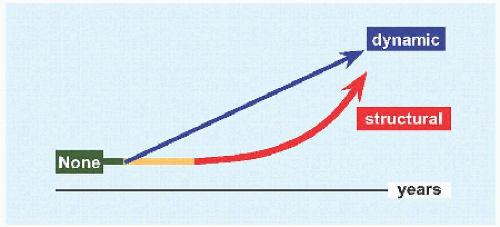
Deformity Deformity may be dynamic or static.
DYNAMIC This reflects errant neural signaling. It may vary by position, for example, upright posture increases tone that accentuates dynamic deformity. Surgical correction is compensatory and less predictable.
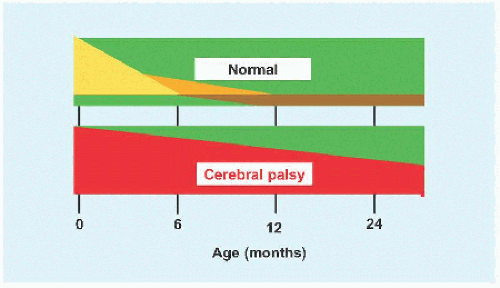
STRUCTURAL Dynamic deformity may become fixed or structural with time [F], such as due to spasticity or positioning in wheelchair. Manual interventions before structural deformity sets in, such as stretching and bracing, may delay onset. Sites of contracture include the skin, muscle, and joint capsule or ligaments. Surgical correction is direct, but may be limited by concomitant contracture of neurovascular structures, which would be intolerant of stretch, for example, popliteal artery and tibial nerve behind a flexed knee. With more time, fixed contractures lead to joint deformity and instability, for example, flattening of the head of the femur subluxated against the rim of acetabulum in cerebral palsy.
Deformity may develop even in the setting of hypotonia, for example, scoliosis. Contracture matters when compensatory mechanisms are overwhelmed, thereby interfering with function. Titrate expectations and interventions according to function. For example, a child in a wheelchair has less demand than does an ambulatory child; by contrast, a plantigrade foot is a universal goal.
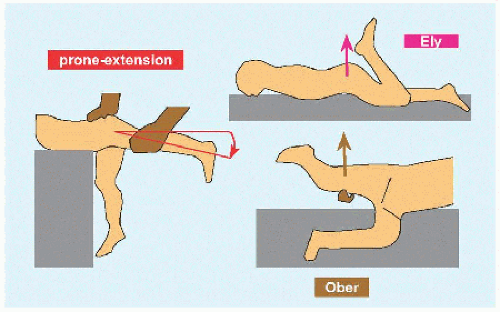
HIP FLEXION This tips the trunk forward, which is compensated for by lumbar hyperlordosis or knee flexion into a crouched gait. Assess this by the prone extension test [G] or by extending the affected hip in the supine position with the opposite hip maximally flexed to eliminate compensatory lumbar lordosis (Thomas). 30 degrees is a guide to release.
HIP ABDUCTION Hip abduction is important for perineal access and care. While limitation of abduction <45 degrees is a guide to release, let function be the ultimate guide.
ILIOTIBIAL TRACT The patient lies decubitus with affected limb up and with opposite hip and knee flexed. Flex, abduct, and extend the affected hip to bring tract over the trochanter major, where it will be tensioned to prevent the ipsilateral knee from adducting beyond midline under gravity (Ober).
GRACILIS In the prone position, abduct the hip with the knee flexed: tensioning the biarticular gracilis by extending the knee causes hip adduction (Phelps).
RECTUS FEMORIS This biarticular muscle flexes the hip and extends the knee. In the prone position, flexion of the knee tensions the muscle: contracture is revealed by the elevation of the buttock as the hip is obligatorily flexed (Duncan-Ely). Rectus femoris contracture also may limit knee extension and draw the patella proximalward (alta).
KNEE FLEXION Measure this by the popliteal angle. Hip flexion to 90 degrees tensions the hamstrings, thereby exposing contracture as the knee is extended.
KNEE EXTENSION Genu recurvatum is abnormal. It may be a direct result or a compensatory mechanism for weakness at the knee.
EQUINUS Invert the hindfoot to lock the subtalar joint. Flex and extend the ankle in knee flexion (gastrocnemius relaxed) and knee extension (gastrocnemius tensioned). 10 degrees of flexion allows heel-toe gait.
0 degree allows a plantigrade foot in the nonambulatory. >30 degrees risks crouch gait in the setting of weakness.
ROTATIONAL PROFILE This often is abnormal in neuromuscular patients. Medial femoral torsion is a characteristic of cerebral palsy. Lateral tibial torsion is a characteristic of spina bifida.
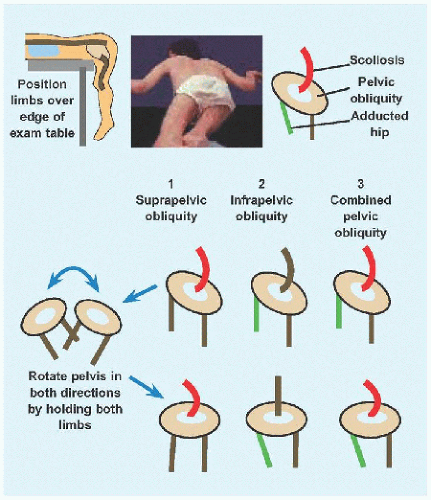
PELVIC OBLIQUITY This may be suprapelvic, originating in the spine, or pelvic, due to hip deformity [H].
SPINE Deformity is common in neuromuscular disease. Assess this in the unweighted prone position, upright, and with traction. Pay attention to the skin for signs of decompensation, such as sore, due to limited movement, and for surgical incisions, for example, spina bifida repair.
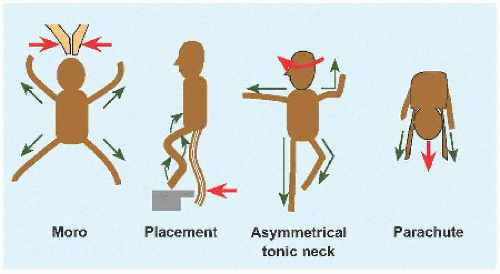
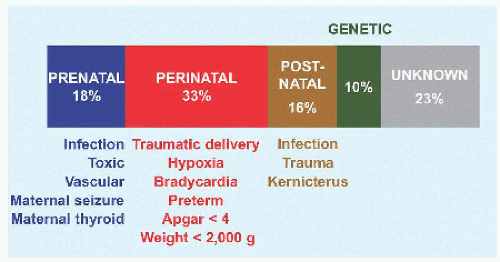
Reflexes Knowledge of reflexes, reactions, and signs is essential to understanding normal and delayed development [I].
MORO A startled baby, for example, simulated fall or clapping, abducts and extends all limbs and spine, which may be followed by opposite movement into an embrace [J]. The reflex is lost by 6 months. This aids differentiation of neonatal paralysis, for example, brachial plexopathy, from pseudoparalysis, for example, due to clavicle fracture.
PLACING REACTION In the vertical suspension position, the anterior leg is brought into contact with an edge: the normal infant flexes hip, knee, and ankle to surmount the edge and spontaneously extends the lower limb when the sole is planted. The reflex also may be elicited in the upper limb with the dorsal forearm as initial point of contact. This is normal up to 12 months.
ASYMMETRIC TONIC NECK Supine and neutral neck. Turn head in one direction then the other: the limbs toward which the head is turned extend while the opposite flex, assuming a “fencer position.” This is lost by 6 months.
PARACHUTE Suspend the baby prone by holding the waist. Simulated fall elicits extension of the upper limbs toward and to protect the head. This appears at 6 months and remains.
EXTENSOR THRUST In the vertical suspension position, pressing the soles down against a flat surface elicits hip and knee extension for support. This reflex is lost by 6 months. Persistence will interfere with normal reciprocal hip and knee flexion during swing phase.
VERTICAL SUSPENSION A baby suspended vertically by the axillæ with examiner’s thumbs supporting the neck flexes the hips and knees until 6 months. Extension and scissoring are signs of spasticity.
PALMAR GRASP The digits contract to receive an object inserted into the palm, and tone in the entire limb increases as the object is withdrawn. This reflex is lost by 6 months.
BABINSKI Plantar stimulation results in extension of the hallux and fanning out of the lesser toes. This reflex is lost by 2 years.
TONIC LABYRINTHINE In the supine position, tilting the head backward produces opisthotonos. This reflex is lost by 6 months.
DEEP TENDON Corticospinal reflex to acute muscle stretch. Hyperreflexia, including clonus >5 beats, indicates upper motor neuron disease.
While primitive reflexes aid diagnosis of developmental delay, they also are prognostic: loss of these reflexes by 2 years is predictive of independent walking.
Imaging
MRI This is the modality of choice for evaluation of the brain. It shows congenital malformations, such as polymicrogyria, heterotopia, and schizencephaly. Other findings in developmental delay include intracranial hæmorrhage or ischæmia, periventricular leukomalacia, cystic encephalomalacia and ventriculomegaly. It also allows determination of whether myelination is appropriate for age.
Laboratory analysis The diagnosis of neuromuscular disease is typically not dependent upon laboratory analysis.
CYTOGENETICS Chromosomal analysis for a genetic disorder.
INFECTION Because of the high prevalence in this patient population, tests such as urinalysis often are indicated. Infectious workup also screens the mother for in utero exposure.
NUTRITION Preoperative assessment may reduce infection rate after major operation, for example, spine fusion for cerebral palsy [K].
PULMONARY FUNCTION Preoperative testing estimates risk of prolonged ventilator dependence after spine fusion in muscular dystrophy.
ELECTROENCEPHALOGRAPHY Diagnosis and evaluation of seizure.
ELECTROMYOGRAPHY AND NERVE CONDUCTION Diagnosis of muscular dystrophy and neuropathy.