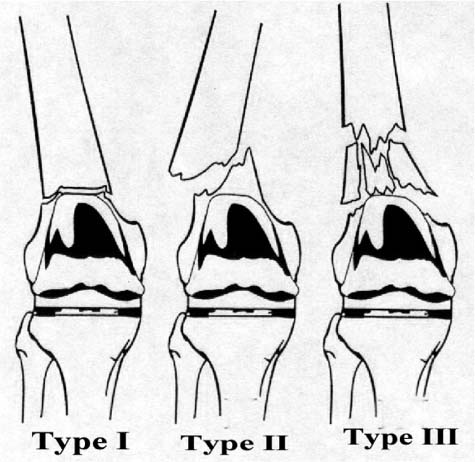
Chapter 25 It is currently estimated that over 200,000 primary total knee arthroplasties (TKAs) are performed each year in the United States. With widening indications, increasing surgeon familiarity with the procedure, and the aging of the U.S. population, this number is expected to increase dramatically over the next decade. TKA continues to be one of the most cost-effective and successful of all operative procedures performed. There has been much mention in the literature of complications such as patellofemoral malalignment, infection, and thromboembolic disease. One of the more rare complications of TKA is periprosthetic fracture. The reported incidence of periprosthetic supracondylar femur fracture is between 0.5 and 2.6%.1 Even though this complication is rare, as the rate of TKA increases over the next few years this will become a relatively common problem. Controversy still exists over the appropriate management of these fractures as the complication rate with both open and closed treatment approaches 20 to 30%.2 Three major factors complicate the treatment of these fractures: (1) typically there is a very small distal fragment with little room for placement of fixation devices, (2) loosening of the femoral component may be hard to assess, and (3) the bone is typically osteoporotic. In addition to the more conventional plating and intramedullary devices used in supracondylar femur fractures, there is currently a great deal of interest in minimally invasive osteosynthesis, which minimizes periosteal stripping and soft tissue dissection. Leaving fracture fragments undisturbed theoretically allows for shorter time to union and greater union rates. This can be vitally important in caring for fractures when one is essentially trying to “win the race” in achieving bony union before failure of fixation. There is also a need for devices to provide adequate purchase in a distal fragment that is typically deficient in both the quality and quantity of bone. One device that combines the concept of minimally invasive osteosynthesis and the concept of a locked internal fixator is the Less Invasive Stabilization System (LISS) developed by the AO Group and produced by Synthes. The possible role of this device in solving some of the more common problems encountered with distal femoral periprosthetic fractures shows great promise. Periprosthetic supracondylar femur fractures typically occur in well-defined patient groups. Osteoporosis seems to be an important risk factor. This is attested to by the fact that supracondylar femur fractures in younger patients without a prosthesis are usually the result of high-energy trauma. However, with periprosthetic fractures the history usually involves low-energy trauma such as a fall from standing height. In a series reported by Cain et al,3 12 of 14 fractures resulted from a simple fall. There is a significant preponderance for the fractures to occur in women in nearly every series reported. The Mayo Clinic joint registry shows that 129 of a reported 161 cases of femur fractures around total knee prostheses were in women.4 Other risk factors for periprosthetic supracondylar femur fractures include any factors that impair mobility or lead to decreased bone stock. Among these would be neurologic conditions such as seizure disorders, ataxia, Parkinson’s disease, or disability secondary to cerebrovascular accident. Disorders that affect bone stock such as rheumatoid arthritis, prolonged use of corticosteroids, or osteolysis also leave the patient at an increased risk for fracture. These factors also tend to make fixation of the fracture more difficult, as adequate purchase in the osteoporotic bone is difficult to obtain. Another risk factor that is more controversial is notching of the anterior femoral cortex. Because of the multifactorial nature of these fractures and their relative rarity, it is difficult to establish the causative nature of notching the anterior femoral cortex in periprosthetic fractures. A recent biomechanical study by Lesh et al5 noted that notching the anterior femoral cortex reduces bending strength by 18% and torsional strength by 39.2%. This provides excellent evidence that notching reduces the strength of cortical bone and may leave the patient at increased risk for supracondylar fracture. The most common classification scheme referenced by most authors is the modified Neer classification.6 In this classification a type I fracture is an extraarticular fracture that is nondisplaced or minimally displaced. Type II fractures are extraarticular fractures that are displaced. Typically types I and II are associated with stable components if there are no subjective or objective signs of loosening of the femoral component prior to the fracture. Type III fractures involve comminution at the fracture site and often are associated with a loose prosthesis. Figure 25–1 shows a modified classification based on the three fracture types as described by Neer.7 FIGURE 25–1 Neer classification of periprosthetic supracondylar femur fractures. (Reprinted from Mabrey JD, Wirth MA. Periprosthetic fractures. In: Rockwood CA, Green DP, Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults. 4th ed. Philadelphia: Lippincott-Raven; 1996:587. With permission from © Lippincott Williams & Wilkins.) A great deal of controversy still exists regarding appropriate treatment of periprosthetic supracondylar femur fractures. Even as operative treatment of supracondylar femur fractures not associated with a prosthesis has been demonstrated to be superior to nonoperative treatment, the same is not true for periprosthetic fractures. Nonoperative treatment remains a viable option. Long leg casting, cast braces, and traction have all been reported with good results, especially with type I fractures.2 Other authors point out that a TKA has no hope of surviving long term without optimal alignment.8,9 They would argue this optimal alignment is difficult if not impossible to achieve with closed treatment. Conventional open treatment options available to the orthopaedic surgeon include 95-degree blade plates, dynamic condylar screws, lateral buttress plates, and external fixation. Each of these options has its own set of pros and cons, with no one method showing itself clearly superior in the literature. Closed treatment remains a viable option in many patients with periprosthetic supracondylar femur fractures. Chen et al2 reviewed the literature on periprosthetic supracondylar femur fractures in 1994 and found 83% of patients with type I fractures (i.e., those that are minimally displaced or nondisplaced) did well with nonoperative treatment. In this study they included casting, cast bracing, traction, and any combination of these in their category of nonoperative treatment. Results were based on final range of motion, patient satisfaction, and achieving bony union. When type II fractures were investigated this rate of satisfactory results fell to 67%. In their discussion they point out the high complication rate with operative treatment (approaching 30%) in some series and note that most studies show no statistical difference between open reduction and internal fixation (ORIF) and closed treatment. McLaren et al10 in a series of 223 cases showed satisfactory results in 56.8% of patients treated closed and in 66.7% of those treated with ORIF using intramedullary rod fixation. This difference was not statistically significant. Chen et al2 concluded that closed treatment was satisfactory for most type I fractures and many type II fractures. They came up with six criteria for open reduction and internal fixation: (1) patient cannot tolerate bed rest, (2) good bone quality, (3) surgeon is technically capable of performing ORIF, (4) patient has multiple fractures, (5) acceptable alignment cannot be achieved by closed means, and (6) no increased risk factors for infection. It is also interesting to note that their rate of major complications was nearly the same in patients treated nonoperatively as those treated operatively, approximately 30% in both groups. The goals of treatment of periprosthetic supracondylar femur fractures as stated by Rorabeck and Taylor8 are: (1) to achieve union of the fracture, (2) to achieve early mobilization of the patient, and (3) to maintain range of motion of the prosthetic knee. Most authors seem to agree that these goals can be achieved with conservative means when dealing with type I fractures. However, most also point out the benefits of ORIF in patients with displaced fractures in achieving rigid internal fixation so that early mobilization and range of motion may be accomplished. In their review, Rorabeck and Taylor8
LISS PLATE FIXATION OF
PERIPROSTHETIC SUPRACONDYLAR
FEMUR FRACTURES
RISK FACTORS FOR PERIPROSTHETIC FRACTURES
CLASSIFICATION OF PERIPROSTHETIC SUPRACONDYLAR FEMUR FRACTURES
CONVENTIONAL METHODS OF TREATMENT OF PERIPROSTHETIC FRACTURES
CLOSED TREATMENT
OPEN REDUCTION AND INTERNAL FIXATION
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree