15 Ligament Injuries: Anterior Cruciate Ligament with Quadriceps Tendon Reconstruction
Patient Presentation and Symptoms
A 17-year-old male basketball player presents with a swollen, painful knee after sustaining an injury during a game in which he experienced a “pop” and sharp pain within the knee. There was immediate swelling with decreased range of motion. The knee has been unstable with weight bearing since the injury.
Indications
Positive Lachman testing and positive pivot shift testing
Contraindications
Open physes
Mechanism of Injury
The injury is produced by sudden deceleration and hyperextension of the knee, often with a rotational component that tears the anterior cruciate ligament.
Physical Examination
- Tenderness and swelling of the knee
- Positive Lachman test
- Decrease in range of motion
Diagnostic Tests
- Anteroposterior (AP), lateral, and patella profile radiographs are needed to access the knee for fractures or bony avulsions.
- Magnetic resonance imaging (MRI) can be useful to assess meniscal injury.
Special Considerations
Care should be taken to assess the knee for combined injuries including posterior cruciate ligament (PCL), collateral ligaments, and especially the posterior lateral corner. A missed posterior lateral rotatory instability will put any repair or reconstruction of the anterior cruciate ligament (ACL) at a high risk of failure.
Preoperative Planning and Timing of Surgery
Delaying surgery for 2 to 3 weeks after the injury is helpful to allow pain, swelling, and inflammation to subside. During this period the patient is placed on a preoperative program to regain and improve muscle tone.
Special Instruments
- ACL guide
- Bioabsorbable interference screws
Anesthesia
Options are general anesthesia, spinal block, epidural block.
Patient and Equipment Positions
- Patient is placed in the supine position.
- Knee is prepped and draped in knee holder.
Surgical Procedure
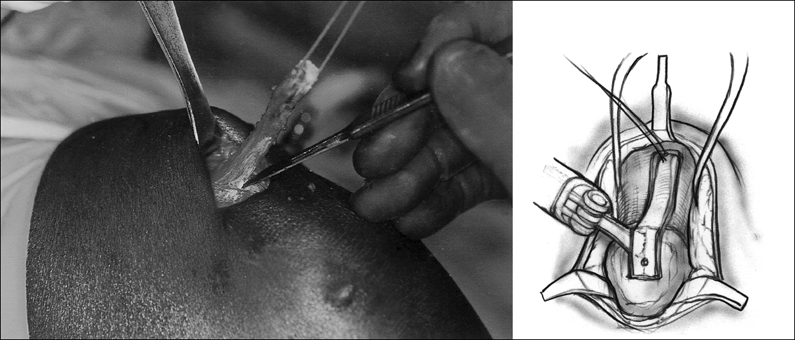
- Make a small longitudinal incision at the superior border of the patella. Dissect the subcutaneous tissue off the patella and the quadriceps tendon for exposure and to mobilize the skin. Start the incision in the quadriceps tendon 1 to 2 mm lateral to the vastus medialis oblique (VMO) (tendon is thickest here) and bring it down onto the patella. A second incision is made 10 mm lateral and parallel to the first incision. Both incisions should penetrate approximately 80% of the quadriceps tendon thickness and not enter the suprapatella pouch. With an oscillating saw harvest a 20-mm bone plug from the patella end of the graft. Prior to removing the plug from the patella, drill a small hole to accept a suture. After freeing the bone plug from the patella, fashion it with a rongeur or burr to pass through a 9-mm sizer. Place two long No. 1 sutures through the bone plug. With distal traction on these sutures and proximal skin retraction, the remaining graft can be harvested with a knife or scissors (Fig. 15–1). Try to stay just above the suprapatella pouch, but any penetration can be repaired when the quadriceps defect is reapproximated. After a total graft length of 85 to 90 mm has been achieved, amputate the graft with scissors. Reapproximate the sides of the defect in the quadriceps tendon with a running absorbable No. 1 suture.
- Size the tendon portion of the graft. The graft should be 10 mm wide and 8 mm thick and pass through a 10-mm sizer. It is preferable to go up to an 11-mm sizer than to trim the graft. The bone plug should fit into a 9-mm sizer. Divide the graft between the vastus intermedius and the rectus femoris (a small layer of fat is present here) up to within 25 mm of the bone plug. Place a baseball stitch of No. 1 absorbable braided suture in each tail of the graft covering 30 mm of length. A graft with a 20-mm bone plug, a 30-mm intraarticular, and two tails 35 to 40 mm long with baseball-type sutures will be produced (Fig. 15–2). Leave the needles attached to these sutures. Resize the graft after all sutures have been placed.
- Make a small skin incision at the anterior medial tibia metaphysis and drill the tibial tunnel to be the same size as the graft. If impactors are used, it is helpful to impact ½ mm larger than the graft size. Make sure the tibial tunnel is at least 45 mm in length to prevent graft/tunnel mismatch and take an accurate measurement of the tibial tunnel at this point.
- Drill the femoral tunnel to accept the 9 mm × 20 mm bone plug. Notch the superior femoral tunnel to accept a screw guide wire. Pass a suture passing pin through the tibial and femoral tunnels to exit the anterior thigh. Hyperflexing the knee keeps this pin from exiting too far proximal in the thigh. Attach the pull-out sutures in the bone plug in the pin and pull them out to exit in the anterior thigh. Prior to pulling the graft into the knee joint, place a screw guide between the two graft tails and secure it in the intraarticular portion of the graft. Pull the graft into the joint, keeping the tails from twisting, and secure the bone plug in the femoral tunnel. An indelible mark on the graft at its bone/tendon junction helps in judging the depth of seating the bone plug.
- Make a small puncture with a No. 15 knife blade through the skin and patella tendon at the level of the tibia plateau and insert a screw guidewire into the superior notch in the femoral tunnel. Use a dilator to ensure enough room between the tunnel and bone plug and then insert a 7-mm × 20-mm interference screw. Absorbable screws are preferred but a metal screw can be used.
- Tension can be applied and the knee cycled to pretension the graft. Use a 25- to 30-mm absorbable screw and the previously inserted screw guide pin to fix the graft in the tibial tunnel. In normal bone use a screw 1 mm smaller than the tunnel, in less dense bone, or if the first screw does not get good purchase, a screw the same size of the tunnel can be used (Fig. 15–3). Using the previous tibial tunnel length measure, insert the screw up to the level of the tibial tunnel’s exit into the joint. Set both sutures into the graft tails to the periosteum at the tibial tunnel exit to add a “safety stitch” to enhance tibial graft fixation.
- Use bone from the tibial tunnel to graft the patella defect and close all incisions with routine closure.
- Size the tendon portion of the graft. The graft should be 10 mm wide and 8 mm thick and pass through a 10-mm sizer. It is preferable to go up to an 11-mm sizer than to trim the graft. The bone plug should fit into a 9-mm sizer. Divide the graft between the vastus intermedius and the rectus femoris (a small layer of fat is present here) up to within 25 mm of the bone plug. Place a baseball stitch of No. 1 absorbable braided suture in each tail of the graft covering 30 mm of length. A graft with a 20-mm bone plug, a 30-mm intraarticular, and two tails 35 to 40 mm long with baseball-type sutures will be produced (Fig. 15–2). Leave the needles attached to these sutures. Resize the graft after all sutures have been placed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








