Lesser Toe Deformities and Bunionettes
Mark E. Easley
Umur Aydogan
Lesser toe deformities may occur in isolation or may be associated with other forefoot disorders. Although some lesser toe deformities are attributable to traumatic, neuromuscular, degenerative, or congenital etiologies, the majority probably result from inappropriate footwear. This chapter addresses the nonoperative and surgical management of lesser toe deformities. To enhance the understanding of lesser toe deformities, functional anatomy and pathogenesis of the various disorders are highlighted. Selected lesser toe disorders include claw toe, hammer toe, mallet toe, metatarsophalangeal (MTP) joint instability, Freiberg infraction, bunionette, intractable plantar keratosis (IPK), and corns.
DEFINITIONS AND ETIOLOGY
Often, lesser toe and forefoot disease are conveniently termed hammer toe and metatarsalgia, respectively; however, metatarsalgia is not a diagnosis, but a general term for plantar forefoot pain. To direct appropriate management, the treating physician must distinguish between the various lesser toe deformities and be familiar with their typical etiologies. Deformities involving the lesser toe joints are classified as follows:
Flexible: passively correctable, usually short to intermediate duration.
Fixed: not passively correctable, long-standing.
Hammer Toe
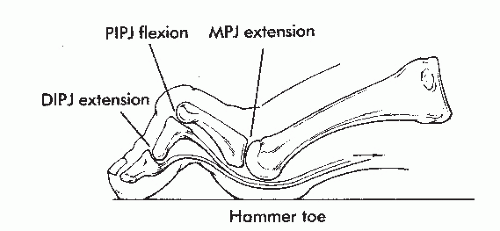
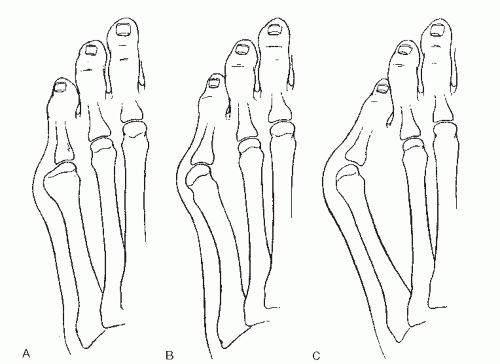
The hammer toe is the most commonly treated lesser toe deformity. Hammer toe deformity is defined by extended MTP and distal interphalangeal (DIP) joints and flexed proximal interphalangeal (PIP) joint posture (Fig. 7.1). Typically, the hammer toe is acquired secondary to direct pressure from inappropriately tight or short footwear. It can be flexible or rigid depending on the passive correctibility to a neutral position.
Claw Toe
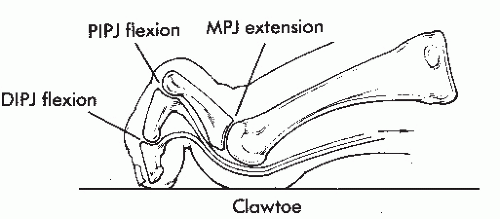
The MTP joint in a claw toe deformity is in extension and the PIP and DIP joints are in flexion (Fig. 7.2). Similar to a claw deformity of the hand, a claw toe deformity is considered an intrinsic minus deformity with weakness or loss of function of the intrinsic muscles of the foot (Fig. 7.3). Tight footwear may contribute to the claw toe deformity, but intrinsic muscle weakness leads to an imbalance between the extrinsic and intrinsic muscles. Occasionally, in bilateral disease, claw toes are secondary to a neurologic condition (and an associated cavus foot) or inflammatory arthritis such as rheumatoid arthritis. Although the terms hammer toe and claw toe are often used interchangeably, these two entities should be distinguished because their treatments may vary.
Mallet Toe
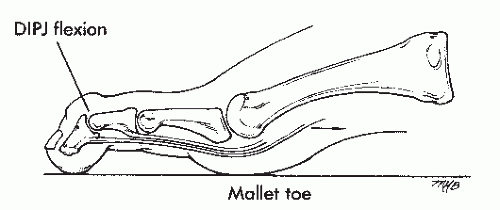
The mallet toe is defined by neutral MTP and PIP joints’ position with DIP joint flexion (Fig. 7.4). Trauma to the DIP joint or extensor mechanism may produce a mallet toe, but tight footwear can be a contributing factor.
Metatarsophalangeal Joint Instability
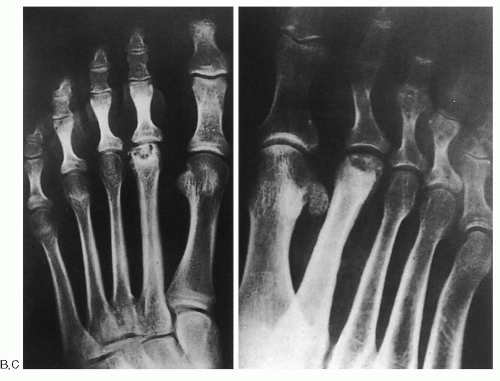
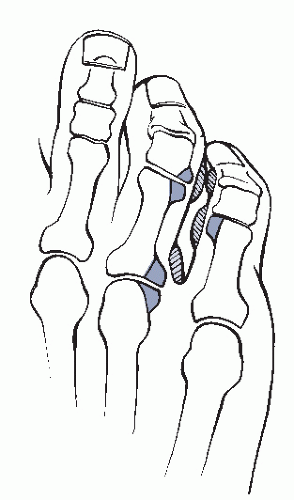
MTP joint instability may occur in any of the lesser toes, but is most prevalent in the second, followed by third and fourth MTP joints. A single traumatic event or, more commonly, repetitive stress or cumulative trauma leads to MTP joint synovitis and eventual subluxation or even dislocation of the second MTP joint (Fig. 7.5). MTP joint imbalance results from weakening of the passive joint restraints. The extrinsic and intrinsic muscles act on the joint without the physiologic resistance of the ligaments. Isolated coronal plane instability is secondary to collateral ligament attenuation and causes toe deviation; isolated plantar plate disruption leads to subluxation and dislocation in the sagittal plane. A combination of plantar plate and collateral ligament weakening may result in multiplanar instability, termed a crossover toe, with the unstable toe displacing over the adjacent toe (Fig. 7.6). A relatively common mechanism for the crossover toe is a patient with hallux valgus and overload of the second MTP joint. Mechanical stress on the second MTP joint eventually leads to the second toe crossing over the hallux. Other factors that may create greater than physiologic stresses to the MTP joint, leading to instability, include the following:
 Figure 7.5 End-stage MTP joint instability with dislocation. Note the associated hammer toe deformity. |
 Figure 7.6 (A) Deviated deformity—the result of isolated weakness or rupture of the lateral ligaments or capsule. (B) Multiplanar instability of the MTP joint causes a crossover toe deformity. |
Long second or third metatarsal
Congenital or iatrogenic shortening of the first metatarsal
Poorly fitting shoes with a tight toe box
Bunionette (Tailors Bunion)
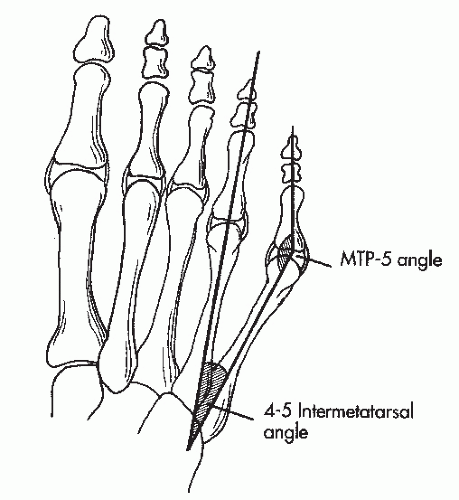
A painful lateral bony prominence of the fifth metatarsal head is termed a bunionette and can be thought of as hallux valgus of the fifth ray. Traditionally, tailors sat in a cross-legged position, creating chronic irritation on the lateral fifth metatarsal head, hence the expression tailor’s bunion. Although chronic pressure on the fifth metatarsal head can produce symptoms without deformity, an increase in the intermetatarsal and MTP joint angle is associated with symptoms. Physiologically, the 4-5 intermetatarsal and MTP-5 angles average 6.2° and 10.2°, respectively (Fig. 7.7). On the basis of radiologic appearance, three types of bunionettes have been defined:
Type I is a simple enlargement of the fifth metatarsal head with lateral prominence, without increase in the intermetatarsal or MTP joint angles.
Type II bunionette deformity is characterized by a congenital lateral bowing of the fifth metatarsal shaft that creates a symptomatic increase in the MTP-5 angle.
Type III deformity is defined by a greater than physiologic 4-5 intermetatarsal angle (Fig. 7.8).
Freiberg Infraction
Freiberg infraction (not infarction) is an osteochondrosis of the lesser metatarsal heads, most commonly recognized in the second metatarsal head. Although the exact etiology remains unknown, current theory suggests that repetitive stress or cumulative trauma results in microfractures and avascular necrosis of the metatarsal subchondral bone. Initial synovitis may progress to articular degeneration. The prevalence of Freiberg infraction appears to be greatest in healthy, adolescent females, but these avascular changes are not isolated to that patient population (Fig. 7.9).
Corns
Hyperkeratotic tissue may form over bony prominences with chronic external pressure; in the toes, these areas of hyperkeratosis are called corns. Purely hyperkeratotic lesions are hard corns, whereas macerated hyperkeratotic lesions are soft corns. Hard corns most commonly occur on the dorsal or lateral aspect of a toe where a prominent condyle contacts the shoe (Fig. 7.10). Soft corns develop between toes in response to contact of adjacent prominent phalangeal exostoses or condyles; the maceration is a result of the web space location (Fig. 7.11). Whereas hard corns are most common on the lateral fifth toe, soft corns are typically found in the fourth web space. Factors that may contribute to formation of corns include tight shoe toebox and relatively long toes.
 Figure 7.9 Radiographic appearance of Freiberg infraction. (A) Early stage with osteolysis and central collapse. |
 Figure 7.10 (A) Hard corns are typically found over the superolateral aspect of the fifth toe. (B) The cause is usually a prominent fibular condyle of the distal phalanx. |
Intractable Plantar Keratosis
IPKs are symptomatic proliferations of hyperkeratotic tissue occurring on a plantar area subjected to greater than physiologic stress, generally under the metatarsal heads. IPKs may be focal or diffuse (Fig. 7.12). The focal IPK comprises a rigid core of avascular tissue and generally develops under the fibular condyle (plantar lateral aspect of the metatarsal head). Often, an IPK is confused with a plantar wart. In contrast, a plantar wart is highly vascular, and if shaved, punctate bleeding can be identified instead of a seed of hard tissue. The diffuse IPK affects more than one metatarsal and is usually a result of a substantial mechanical imbalance of the forefoot, such as a short first metatarsal (congenital or iatrogenic) or cavus foot. The IPK develops diffusely as the primary weight-bearing area is transferred to the lesser metatarsal heads.
FUNCTIONAL ANATOMY
The lesser toes increase the forefoot weight-bearing area during the stance phase of gait. Proper balance of the extrinsic and intrinsic musculatures and passive ligamentous or capsular restraints allows physiologic propulsion during pushoff and a physiologic resting position of 20° of dorsiflexion relative to the metatarsals.
Physiologic lesser toe balance and function rely on intact passive and dynamic stabilizers. The primary passive MTP joint stabilizers are the plantar fascia, plantar plate, and collateral ligaments. The plantar fascia augments the stabilizing effect of the plantar plate; these two structures have a combined 30% role in preventing the dorsal dislocation of the MTP joint. Although greater tensile strength of the plantar plate will be advantageous for joint stability, it will be deleterious to effective joint dorsiflexion during gait. The collateral ligaments are the more powerful static MTP joint stabilizers, contributing 50% of the resistance to dorsal dislocation and the majority of medial and lateral stability. The remainder of the stability is derived from the dynamic stabilizers.
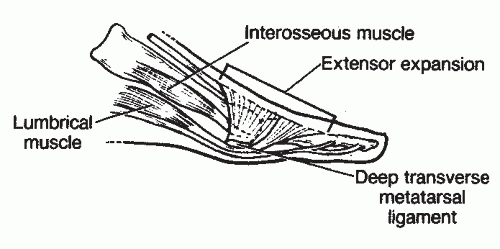
Lesser toe extensor and flexor anatomy is complex. The extensor digitorum longus (EDL) branches into three slips over the proximal phalanx. The central slip inserts onto the dorsal base of the middle phalanx, and the two lateral slips converge distally and insert onto the dorsal base of
the distal phalanx (Fig. 7.13). Although the EDL has no direct connection to the proximal phalanx, it has indirect attachments through a fibroaponeurotic sling. The three EDL slips and fibroaponeurotic sling form the extensor hood. The EDL dorsiflexes the toe most effectively with the MTP joint in plantarflexion or neutral position; this explains why EDL function is neutralized by extension of the proximal phalanx in a hammer toe deformity. The extensor digitorum brevis (EDB) inserts into the lateral part of the extension hood of the second, third, and fourth proximal phalanges, enhancing toe dorsiflexion.
the distal phalanx (Fig. 7.13). Although the EDL has no direct connection to the proximal phalanx, it has indirect attachments through a fibroaponeurotic sling. The three EDL slips and fibroaponeurotic sling form the extensor hood. The EDL dorsiflexes the toe most effectively with the MTP joint in plantarflexion or neutral position; this explains why EDL function is neutralized by extension of the proximal phalanx in a hammer toe deformity. The extensor digitorum brevis (EDB) inserts into the lateral part of the extension hood of the second, third, and fourth proximal phalanges, enhancing toe dorsiflexion.
The flexor group of muscles comprise the flexor digitorum longus (FDL), flexor digitorum brevis (FDB), and intrinsic muscles. The FDL inserts onto the distal phalanx base to flex the DIP joint; the two slips of the FDB attach at the base of the middle phalanx base to flex the PIP joint. The intrinsic muscles comprise seven interosseus and four lumbrical muscles. The interossei originate from the metatarsals, course plantar to the metatarsal head axis, and attach at the proximal phalangeal bases and plantar plate. The lumbricals take origin from the FDL tendons, pass plantar to the transverse intermetatarsal ligament, and insert onto the medial proximal phalanx and extensor hood. Because there is no lumbrical laterally, attenuation of the lateral collateral ligament may be exacerbated by the effects of the lumbrical anatomy. Under physiologic conditions, however, the interossei contribute balanced dynamic plantarflexion and transverse axis MTP stabilizing forces. In addition to plantarflexing the MTP joints, the lumbricals extend the interphalangeal joints (Fig. 7.14).
PATHOPHYSIOLOGY
Trauma, congenital deformity, neuromuscular disease, and inflammatory arthropathy may induce lesser toe deformities, but the commonest factor leading to acquired lesser toe malalignment remains improper footwear. Consistent use of unaccommodating narrow shoes with tight toeboxes creates external forces on the MTP and interphalangeal joints that over time may disrupt the delicate static and dynamic balance responsible for maintaining anatomic toe alignment (Fig. 7.15). Initial synovitis evolves into ligament (static restraint) attenuation and eventual eccentric forces from the dynamic stabilizers (intrinsic and extrinsic muscles). Furthermore, unaccommodative footwear may promote the development of hallux valgus, leading to second toe impingement and further eccentric second toe joint stresses.
Imbalance between the extrinsic and intrinsic muscles, either from neuromuscular disease (i.e., Charcot—Marie—Tooth, peripheral neuropathy) or from consistent external pressure (tight footwear) may lead to shortening of the intrinsic musculotendinous units. Without the physiologic stabilizing effect of the intrinsics, the MTP joint assumes an extended posture and the interphalangeal joint a flexed posture. Ultimately, this imbalance may evolve into hammer toes, claw toes, or MTP joint instability.
 Figure 7.15 A narrow toebox shoe can cause significant crowding of the toes, which can lead to deformities. |
Cumulative trauma or repetitive stress and inflammatory arthropathies may create MTP joint synovitis that contributes to attenuation of the static restraints (MTP joint capsule, collateral ligament, and plantar plate). Eventually, MTP joint subluxation and even dislocation may occur. In the second toe, development of deformity may be accentuated by a relatively long second metatarsal or concomitant hallux valgus. Moreover, if the lateral collateral ligament weakens, the medial pull of the unopposed lumbrical may further disrupt the balance. With loss of both the transverse and the sagittal restraints, instability may evolve into a claw toe that crosses over the hallux (see Fig. 7.6B).
DIAGNOSIS
History
The patient may have difficulty in identifying the focus of pain, but the pain is typically isolated to the forefoot. Occasionally, the symptoms are easy to localize, if they are confined to the dorsum of the affected toes. Hammer and claw toes may impinge on the toe box of tighter shoes; the pain is typically relieved when the patient is barefooted. Likewise, a mallet toe is usually symptomatic at the tip of the toe only. With synovitis and attenuation of the MTP joints, patients typically report pain on the plantar forefoot, but may not be able to identify the exact location of pain. Freiberg infraction may have a similar but vaguer presentation. In contrast, IPKs, particularly focal IPKs, are simple to isolate on the plantar foot. Bunionettes are also easy for the patient to localize because the pain is uniformly over the fifth metatarsal head—laterally or plantarward.
Occasionally, forefoot pain involving the lesser toes may have a systemic etiology. Given that forefoot pain may have a neurogenic component, the patient should be questioned about diabetic neuropathy and lower back pain with radiating symptoms. If symptoms persist despite non— weight-bearing and rest, peripheral neuropathy may be contributing to the generation of pain. Typically, these symptoms are burning in nature. Neuralgia may also be focal, as with a Morton neuroma; patients may describe a vague lateral forefoot discomfort interrupted by occasional sharp, shooting pains. If symptoms continue or even worsen with elevation, consideration should be given to peripheral vascular disease. Forefoot symptoms may also be secondary to an inflammatory arthritis, and the patient should be questioned about a possible rheumatologic condition.
The history should help focus the diagnosis. Although metatarsalgia is relatively nondescript, some patients may have atrophic fat pads. These individuals often feel pain relief in shoes and cannot ambulate comfortably barefooted.
Physical Examination
Although the diagnosis may appear obvious, the physician should resist the temptation to focus the examination to the affected toe. For example, a tight heel cord may be contributing to forefoot overload and should be treated in conjunction with correction of the toe deformity. Similarly, a relatively obvious claw toe deformity may be associated with hallux valgus, and treatment of the lesser toe without addressing the great toe malalignment leads to early recurrence of the lesser toe deformity.
A brief examination of the lower back with a straight leg raise test can rule out a radiculopathy. Checking pulses and sensation should identify peripheral vascular disease and neuropathy, respectively. An equinus contracture or cavus foot alignment may lead to forefoot overload. Percussion and compression over the tibial nerve to elicit a Tinel sign should rule out a compressive plantar neuralgia.
A thorough forefoot examination should avert missing associated forefoot pathology. Whereas tenderness with direct dorsal palpation of the metatarsals is suggestive of a stress fracture, tenderness between the metatarsals is indicative of an interdigital neuralgia (compressive neuropathy from perineural fibrosis of the common digital nerve, i.e., “Morton neuroma”).
Lesser toe deformities frequently occur in association with disorders of the great toe. Hallux valgus may contribute to second toe disease, with chronic impingement. in combination with tight footwear, second toe hammering, clawing, or instability in particular may occur (see Fig. 7.15). Hallux rigidus or stiffness of the great toe MTP joint may lead to compensatory overload of the lesser metatarsal heads; likewise, a congenitally or iatrogenically short first metatarsal may have a similar effect.
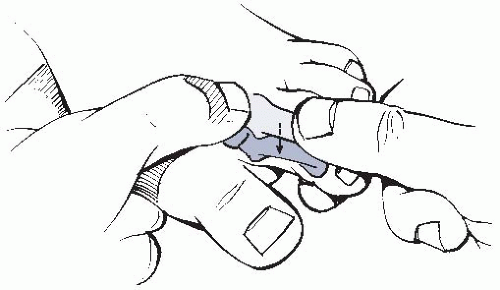
Lesser toe MTP joint instability evolves from synovitis and capsulitis. Tenderness directly over the joint with dorsal and plantar pressure indicates articular disease. With metatarsalgia and IPKs, the tenderness is isolated to the plantar aspect of the metatarsal heads. As synovitis and repetitive trauma to the involved joint progresses, plantar
plate and collateral ligament insufficiency can be demonstrated with a toe Lachman test (Fig. 7.16). Toe deviation, subluxation, or dislocations become clinically apparent with more advanced disease.
plate and collateral ligament insufficiency can be demonstrated with a toe Lachman test (Fig. 7.16). Toe deviation, subluxation, or dislocations become clinically apparent with more advanced disease.
It is difficult to distinguish MTP joint synovitis from interdigital neuralgia, especially the second MTP joint instability from a second web space interdigital neuroma. If no deformity is noted, no instability is demonstrated, and there is some difficulty in distinguishing MTP joint disease from interdigital neuralgia, then a diagnostic (and possibly therapeutic) injection may be diagnostic. The injection can be performed into the joint, the web space, or both, but in a staged fashion. With advancing MTP joint instability, deformity progresses. The proximal phalanx may be subluxed or dislocated on the lesser metatarsal head. The joint and prominent metatarsal head are tender. The MTP joint may be reducible if the deformity is flexible. With associated collateral ligament attenuation, toe deviation is noted. Occasionally, the deformity is not apparent when the patient is non—weight-bearing, but becomes obvious with the patient standing. A common example of this is a crossover second toe in a patient with hallux valgus. Deviation is apparent, but the crossover may not occur until the patient stands (Fig. 7.17).
 Figure 7.17 Patients should also be examined in non—weight-bearing (A) and weight-bearing (B) positions to see the dynamic nature of the deformity. |
The clinical examination should document whether the deformity is flexible or fixed because this finding dictates the surgical treatment. Metatarsalgia is an inexact term meaning pain beneath the metatarsal heads. With atrophy of the fat pads (typically in older patients) or in patients with claw toe deformities (where the fat pads are displaced distally), tenderness is directly over the metatarsal heads. IPKs also produce tenderness on the plantar aspect of the metatarsal heads but with thickened skin. A focal plantar keratosis is located under a specific metatarsal head and a diffuse IPK is under multiple heads. The diffuse form is typically associated with hallux disorders, typically shortening of the first metatarsal. To distinguish a focal IPK from a plantar wart, the callused area should be trimmed. With paring of the lesion, the IPK has a deep keratotic area, whereas the plantar wart reveals punctate bleeding. Furthermore, an IPK is most tender with direct pressure, whereas a plantar wart is most tender with side-to-side “pinching” of the lesion.
A bunionette is tender on the lateral fifth metatarsal head; occasionally, tenderness is also present on the plantar aspect of the fifth metatarsal head. Although the problem may be isolated to the fifth MTP joint, typically widening of the forefoot
is evident. The examination should not only identify widening of the 4-5 intermetatarsal angle, but also include an evaluation of the hallux and 1-2 intermetatarsal angle because occasionally to effectively relieve lateral symptoms, the first ray may need to be addressed. Coexisting hindfoot varus and fifth toe clawing need to be identified because these may be responsible for lateral and plantar fifth metatarsal overload, respectively.
is evident. The examination should not only identify widening of the 4-5 intermetatarsal angle, but also include an evaluation of the hallux and 1-2 intermetatarsal angle because occasionally to effectively relieve lateral symptoms, the first ray may need to be addressed. Coexisting hindfoot varus and fifth toe clawing need to be identified because these may be responsible for lateral and plantar fifth metatarsal overload, respectively.
Finally, we also evaluate the midfoot, hindfoot, and ankle with the patient standing. Limited active or passive ankle or transverse tarsal joint (talonavicular and calcanocuboid) dorsiflexion and/or cavus foot posture may contribute to forefoot overload or deformity. Limited active or passive hindfoot eversion or varus hindfoot position may contribute lateral forefoot overload. Although the problem and patient’s complaints may be isolated to the forefoot, we recommend examining the entire foot and ankle to identify associated pathology.
Imaging Studies
A standard set of standing foot radiographs (anteroposterior [AP], lateral, and oblique) generally suffices to evaluate lesser toe deformities. It is important to obtain weight-bearing X-rays, which provide a better appreciation for the extent of deformity. The hindfoot and midfoot are also inspected to ensure that there is no deformity that may contribute to forefoot disease. First ray deformities (e.g., hallux valgus, hallux rigidus, short first metatarsal) should be noted. Radiographs usually rule out stress fractures and arthritic change. Furthermore, relative length discrepancies, such as a long second metatarsal, can be confirmed (Fig. 7.18). AP and particularly oblique X-rays may reveal evidence for Freiberg infraction (subchondral collapse of the metatarsal head) or inflammatory arthropathy (periarticular erosions); in our opinion, Freiberg infraction is best visualized on the oblique foot radiograph. All three views help define hammer toe, claw toe, and MTP instability. The hammer toe and claw toe deformities are evident on the lateral view, with the affected phalanges visualized in profile, dorsal to the other toes. On the AP view with severe hammering, clawing, or MTP joint dislocation, the proximal phalanx may be seen axially, giving a “gun barrel sign” (Fig. 7.19).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree