Leg Length Inequality
Prevention/Treatment
Saurabh Khakharia and William A. Jiranek
Key Points
Introduction
True limb length is usually defined as the distance from the anterior superior iliac spine to the medial malleolus. True leg length inequality is defined as lengthening or shortening of the above measurement as compared with the contralateral limb. Apparent leg length is defined as the distance from the umbilicus to the medial malleolus; thus an assessment of the coronal plane equality of the pelvis or spine must be included in the evaluation. Table 104-1 lists the possible combinations of true and apparent leg lengths and their causes.
Table 104-1
Possible Combinations of True and Apparent Leg Lengths and Their Causes
| Combination | Cause |
| TLL and ALL equal | Limb length is equal, pelvis is balanced |
| TLL and ALL unequal same amount | Limb length is unequal, pelvis is balanced |
| TLL equal and ALL unequal | Pelvic obliquity exists |
| TLL unequal and ALL equal | Limb length inequality and compensatory pelvic obliquity are present |
ALL, Apparent leg lengths; TLL, true leg lengths.
In 1979, Sir John Charnley1 stated that overlengthening of up to 1 cm can be justified because “… it permits active rehabilitation … and patients very soon become adjusted to 1 cm overlengthening.” Nonetheless, in most situations with careful preoperative templating and intra-operative trialing, leg length discrepancies can largely be avoided.
Incidence and Prevalence
No precise definition has been put forth for leg length inequality following total hip arthroplasty (THA); therefore, its prevalence following THA remains unknown. Incidence varies from 1% to 27%.2 Mean leg length discrepancy after hip arthroplasty as reported in the literature ranges from 2.8 to 11.6 mm,3–6 with some series reporting greater variability (1 to 15.9 mm).7–12 Leg length inequality is perceived in approximately 32% to 43% of patients with a substantial (defined as greater than 1 cm) limb length discrepancy following THA.3,7
Notable leg length inequality may be associated with gait disorders,13,14 back pain,15,16 nerve injury,17 and the need in severe cases for revision surgery.18 Nerve injury is among the most feared and difficult to manage consequences of leg lengthening, and although some authors have documented an amount of lengthening associated with sciatic nerve palsy, the exact amount by which a limb can be lengthened is unclear. However, the majority of studies show that a range of 2 to 2.5 cm is safe in most patients. (See Chapter 105, “Neurovascular Injuries,” for more information.17) Leg length inequality can give rise to patient dissatisfaction, which can adversely affect an otherwise good outcome and is a common reason for litigation following THA.
To prevent the previously mentioned problems associated with leg length inequality, the surgeon should take precautionary steps both before and during the operation.
Steps to Prevent and Minimize Leg Length Inequality
Steps to prevent and minimize leg length inequality should include preoperative and intraoperative assessments of leg length.
Preoperative Assessment
History and Physical Examination
Evaluation should begin with a thorough history and physical examination. Patients should be asked if they perceive any leg length inequality or have any history of unequal hemming of pants or of flexing one knee, preferentially in the stance phase. A history of spinal deformity, hip dysplasia, muscular dystrophy, poliomyelitis, or spinal surgery, including spinal fusion, may be associated with leg length inequality. Physical examination can include an assessment of true and apparent leg length inequality, contractures around the hip joint, spine curvatures, and pelvic obliquity. Clinical methods such as tape measurement and standing blocks can be used as screening tools for measurement of leg lengths.
Measuring True Leg Length Inequality
The “Direct Method”: Using a Tape Measure.
A tape measure is used to measure the length of the lower extremity by determining the distance from the anterior-superior iliac spine to the medial malleolus; this reflects the actual length of the extremity. The range of error of this measurement has been reported to be .5 to 1.0 cm.19,20 This is also known as the direct method of measuring leg length (Fig. 104-1). However, difficulty in identifying bony prominences, particularly in obese patients, and angular deformities in the lower limb can contribute to error when this clinical measurement tool is used.
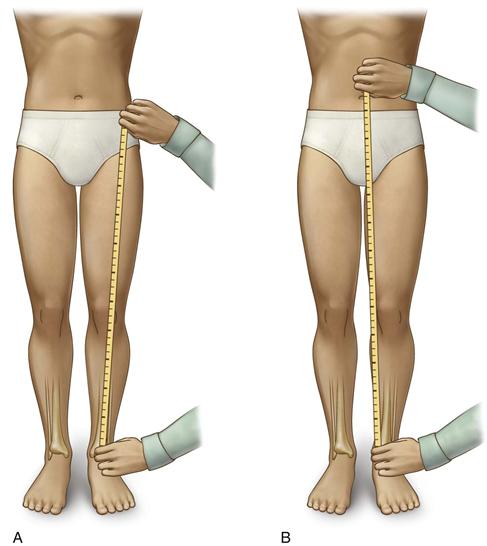
Figure 104-1 Direct tape measurement to assess leg length. A, True leg lengths. B, Apparent leg lengths.
Eichler and coworkers19 described several potential sources of error when measurements are obtained using a tape measure, including poor reproducibility of finding the anterior-superior iliac spine (ASIS) and abduction or adduction contractures of the hip. Beattie and colleagues20 reported on the reliability of tape measure method (TMM) measurements. They found low reliability (interclass correlation coefficient [ICC] of 0.668; ICC is a descriptive statistic that describes how strongly units in the same group resemble each other) when measurements were obtained by different examiners (interobserver variability). However, when the mean value of paired measurements taken by the same observer was used, intraobserver variability was much lower (ICC, 0.910). Investigators concluded that the reliability of tape measure measurement improved when the means of repeated measurements by the same observer were compared with measurements by other observers.
The Indirect Method: The “Block Test.”
The use of blocks placed underneath the patient’s foot is known as the indirect clinical method of assessing leg length inequality. It is helpful in differentiating fixed from flexible pelvis obliquities. Causes of fixed pelvic obliquities include lumbosacral fusion and severe lumbar degenerative scoliosis, as well as previous pelvic fracture. The surgeon can inspect and palpate the spinal curvature and the pelvic tilt; then the pelvis should be leveled by placing a series of blocks under the short leg until the spinal curvature and pelvic tilt disappear (Fig. 104-2). If the pelvic tilt corrects, then the pelvic obliquity is flexible; if not, the patient has a fixed pelvic obliquity and will be unable to compensate for any change in leg lengths. Regardless of whether the patient has a fixed or a flexible pelvic obliquity, the height of the block that the patient identifies as making him feel equal indicates the amount of length discrepancy that the surgeon can consider correcting.

Figure 104-2 Indirect clinical method (block test) used to assess leg length inequality.
Hanada and colleagues21 studied the reliability and validity of measuring leg length inequality using the iliac crest palpation and block correction method in 34 healthy volunteers with simulated leg length inequality; they compared clinical observations with those obtained using standing anteroposterior (AP) pelvis radiographs. Iliac crest palpation underestimated the leg length discrepancy by a mean of 4 mm. Similar findings have been reported by other authors.22
Measuring Apparent Leg Length Inequality
When a patient has apparent leg length inequality, despite true leg lengths being equal, the patient feels that one limb is longer. Apparent leg lengths are measured from the umbilicus to the medial malleolus. Apparent leg length measurement takes into account contractures around the hip and lumbar spine pathology, both of which can lead to pelvic obliquity. An abduction contracture of the hip, which is common in the early postoperative period, results in an apparent leg length discrepancy on the involved side, but an adduction contracture of the hip has the opposite effect (Fig. 104-3).
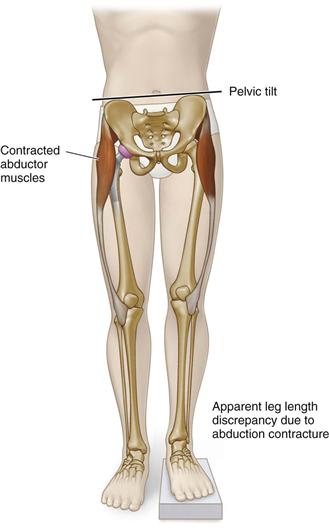
Figure 104-3 An example of apparent leg length inequality due to abduction contracture.
Chronic lumbar spine pathology can produce a fixed pelvic obliquity. Adding blocks underneath the lower extremity in a patient with fixed pelvic obliquity will not level the pelvis and spinal curvature. If a fixed obliquity is recognized preoperatively, the patient can be educated that hip replacement surgery may not equalize an apparent leg length inequality.
Radiographic Assessment.
Radiographs may be used to confirm clinical measurements. Radiographic evaluation can include the following:
Techniques for assessing leg length inequality using radiographs are described in the following section.
AP pelvis radiograph.
A low-centered AP radiograph of the pelvis with both femurs in 10 degrees of internal rotation along with a true lateral of the hip is optimal for templating. According to Woolson and colleagues,23 transverse lines are drawn across a pelvic reference point (typically the bottom of the obturator foramen) and a femoral reference point (typically the top of the lesser trochanter). A line is then drawn from each femoral reference point to the perpendicular intersection with the pelvic reference line. This distance between the two reference points is taken as an index of preoperative and postoperative leg length (Fig. 104-4).

Figure 104-4 Radiographic assessment of leg length inequality using the Woolson technique.
Konvyes and coworkers7 used the inferior margin of the acetabular teardrop and the most prominent point of the lesser trochanter and the center of rotation of the femoral head as reference points and then measured the distances between them. They reported this method of determining leg length inequality due to hip abnormality to be as reliable as orthoroentgenograms and reproducible with a measurement error of ±1 mm.
Full Limb Standing Radiographs.
Full limb radiographs are another method used to measure leg lengths. This method helps the surgeon to identify other potential causes of leg length inequality such as prior trauma affecting epiphyseal growth or malunited fractures. Sabharwal and Kumar24 evaluated the limb length obtained with the use of a full-length standing anteroposterior radiograph of the lower extremities and compared it with lengths obtained with the use of plain radiograph scanograms on 111 patients. Measurement of limb length inequality on a standing anteroposterior radiograph was very similar to that on a scanogram, especially in the absence of substantial mechanical axis deviation.24
Beattie and colleagues,20 in a prospective study, used a plain radiograph scanogram as the gold standard in 19 patients to compare the variability of measurements of true leg lengths performed with a tape measure. The mean value obtained from the two clinical measurements correlated better with the radiographic measurement of leg length inequality than with those obtained during the first and second clinical assessments. The authors concluded that the surgeon should not rely solely on clinical assessment of leg length inequality and encouraged using the average value of two separate measurements when obtaining a tape measurement. In another study, Cleveland and coworkers25 compared tape measurements of leg length discrepancy (measured from the anterior-superior iliac spine) of 10 standing patients with standing and supine radiographs. They reported a statistically significant difference and poor to moderate correlation when comparing clinical and radiographic techniques but found no difference in measurements obtained between sitting and standing radiographs.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








