I. Introduction—Knee trauma involves a continuum of velocity and energy that changes a knee injury from what is classically considered sports injury (low velocity, low energy) to motor-vehicle injury (high velocity, high energy). Frequently, there is blurring of this distinction based on either energy or velocity, since overlap of injury type exists in both groups. Associated injuries, such as soft-tissue injuries (open vs. closed), fractures, and neural or vascular injuries, are more frequent in motor vehicle trauma, but can be present in sporting injuries as well. The terms dislocation and fracture-dislocation can be confusing, but are important to distinguish. Fracture-dislocation can be considered part of a continuum of fracture and ligamentous injuries, from the classic tibial plateau fracture (in which the ligaments are not torn), to fracture-dislocation (usually a tibial or femoral condyle fracture with a ligament injury), to pure ligamentous injuries (knee dislocations [KDs]). These distinctions are important clinically, especially in recognition of an associated vascular injury in regards to the surgical treatment. Lastly, approximately 20% of KDs frequently reduce spontaneously after the initial injury, and may not be recognized on cursory plain radiograph inspection. The concepts of examination under anesthesia (EUA) and acute versus chronic management of knee ligament injuries (e.g., repair or reattachment vs. reconstruction) are important in the management of knee trauma.
II. Knee Dislocations
A. Introduction—Knee dislocations (KDs) classically involve pure ligamentous injuries (but also include avulsions of ligaments) of the knee wherein the tibiofemoral joint is completely displaced at the time of injury. Initially, KDs were felt to occur only with tearing of both cruciate ligaments, but dislocations have since been shown to occur with an intact anterior cruciate ligament (ACL) or poster cruciate ligament (PCL) (Figs. 8-1 and 8-2).
B. Classifications—In the literature, three systems are used regularly to classify KDs and involve one of three types: (a) joint position after dislocation, (b) velocity or energy of the injury, and most recently, (c) anatomic structures torn. All three systems are useful but serve different purposes in diagnosis and treatment.
1. Joint position after dislocation—Initially described by Kennedy, joint position after dislocation places dislocations in one of five groups: (a) anterior, 40%, (b) posterior, 33%, (c) medial, 4%, (d) lateral 18%, and (e) rotatory, 5%. Position is based on standard orthopaedic nomenclature and is named by the position of the distal articulating structure (tibia) as related to the proximal one (femur). Joint position is useful in classifying KDs, especially as related to reduction maneuvers. Rotatory dislocation most commonly involves a posterolateral dislocation (torn ACL, PCL, or medial collateral ligament [MCL]), is a complex dislocation (that requiring open reduction due to interposed soft tissue preventing closed reduction as seen in a posterolateral KD with an invaginated MCL and medial knee skin furrowing), is associated with peroneal nerve palsy, and is at high risk for soft tissue necrosis. Over 20% of KDs spontaneously reduce after injury, and hence cannot be classified by position. Furthermore, position does not determine what ligaments are torn (i.e., anterior dislocations can occur with or without tearing of the PCL), and treatment depends on the ligaments and tendons injured. Thus the position classification is useful, but has limitations, especially in directing definitive ligamentous treatment.

FIGURE 8-1 Lateral radiograph revealing an anterior KD that reduced with axial traction. The widened distance between the patella and the femur is characteristic of a KD with both an ACL and a PCL injury. There is greater anterior translation of the tibia on the femur. (Reprinted with permission from Stannard JP, Schenck RC Jr, Fanelli GC. Knee dislocations and fracture-dislocations. In: Bucholz RW, Heckman JD, Court-Brown C, et al., eds., Rockwood and Green’s Fractures in Adults. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006.)

FIGURE 8-2 Lateral radiograph of a PCL-intact KD. Note the proximity of the patella to the femur as compared to that in Figure 8-1. (Reprinted with permission from Stannard JP, Schenck RC Jr, Fanelli GC. Knee dislocations and fracture-dislocations. In: Bucholz RW, Heckman JD, Court-Brown C, et al., eds., Rockwood and Green’s Fractures in Adults. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006.)
2. Velocity or energy of the injury—High-energy, high-velocity motor vehicle injuries account for over 50% of all KDs, and low-energy, low-velocity sporting injuries account for approximately one-third (33%). Although velocity and energy are not interchangeable, sports KDs are considered low velocity or low energy and are considered to have a lower incidence of associated vascular injury as compared with motor vehicle injuries. Regardless of the energy of injury (high or low), the risk of popliteal arterial injury still exists and must be ruled out with the initial clinical evaluation.
3. Anatomic structures torn—The anatomic classification was developed by Schenck to classify KDs by the ligaments torn and thus help direct treatment, compare injuries, and use with all dislocations, even those with spontaneous reduction (those unclassifiable by the joint position system). The anatomic classification requires a standard ligamentous examination to determine which ligaments are torn (Table 8-1). The numeric system uses the two cruciates and two corners (medial or lateral) in combination to describe what can potentially be torn. Increasing numbers in the anatomic system usually implies increasing severity/energy of injury. The anatomic classification uses four classes with five basic injury patterns: KD-I, a single cruciate ligament-intact KD, such as a PCL-intact KD in which the ACL and posterolateral corner are torn, or the ACL-intact KD (tibia is dislocated posteriorly, PCL is torn), which has also been described but is rare; KD-II, ACL and PCL torn and the collaterals are structurally/clinically intact (rare); KD-IIIM (medial) ACL, PCL, and MCL and posteromedial corner torn and the lateral side is clinically intact (most common); KD-IIIL (lateral), ACL, PCL, and posterolateral corner torn, and the medial side is intact; KD-IV, all four ligaments torn (highest energy of injury). The distinction of a clinically intact corner, such as the posterolateral corner in the KD-IIIM, is based on EUA. For example, the KD-IIIM on MRI may have subtle injury changes to the posterolateral corner, but on EUA, the lateral ligaments are structurally competent, thus its distinction from a KD-IV injury. The increasing number implies increasing severity and energy of injury. The modifiers C and N are used for arterial or neural injuries, respectively (C as in Gustilo type IIIC injury and N as in nerve injury). Although surgical techniques change over time, basing the classification on what is torn directs treatment and the appropriate surgical exposure (Fig. 8-3).
C. Associated Injuries—KDs have a wide variation of associated injuries and include vascular injuries, neurologic injuries, fractures, soft-tissue injuries, tendinous injuries, meniscal and hyaline injuries, and of course ligamentous injuries.
1. Vascular injuries
• Popliteal artery—Anatomically, the popliteal artery is rigidly fixed at the adductor hiatus proximally and at the soleus arch distally; tibiofemoral displacement can injure the vessel by traction or direct transection. Collateralization is rich about the knee but insufficient to perfuse the extremity. Limb loss is imminent if revascularization is not performed within 6 to 8 hours from the time of popliteal artery injury. The overall incidence of arterial injury is 20% and varies dependent on population studied. Low-velocity KDs have a lower incidence of arterial injury (approximately 8%).
• Clinical examination—An initial clinical vascular examination of the knee is absolutely necessary (Fig. 8-4). The presence of pulses does not rule out an arterial injury, especially if there is an intimal injury or collateral rupture. However, the absence of pulses (or equivocal findings of vascularity) implies an arterial injury and cannot be considered a temporary finding of spasm that will resolve with time. After adequate joint reduction has been emergently performed, the presence of continued vascular insufficiency requires emergent revascularization, which should not be delayed for arteriography. Recent studies have documented the usefulness and safety of sequential clinical examinations (pulses) to rule out arterial injury. However, any evidence of vascular insufficiency must be further evaluated with vascular consultation, ultrasonography (if available) or arteriography.
• Arteriography—The indications for use of arteriography have become controversial, but arteriography still remains the gold standard for ruling out an arterial injury. Decision making in the presence of vascular insufficiency usually involves a one-shot intraoperative arteriogram before vascular exploration and revascularization. In the past, decision making in the presence of normal pulses has always required arteriography. More recently, clinical observation of normal palpable pulses and the use of noninvasive arterial Doppler studies with ankle–brachial indices have been shown as reliable in the presence of a normal vascular examination. Ankle–brachial indices of less than 0.90 are strongly predictive for vascular injury. Arteriography is still frequently used, especially in patients with multiple injuries or in the patient with closed head trauma. The onus is on the clinician to rule out an arterial injury.
• Compartment syndrome—Severe leg pain in the presence of a KD or stocking-glove paresthesias of the leg (indicating a late compartment syndrome) implies a compartment syndrome. Vascular examination should involve consideration of compartment syndrome and if indicated requires compartment pressure measurement and a fasciotomy if pressures are above 35 mm Hg. (The indications for fasciotomy change if the systemic blood pressure is low or if revascularization is performed.)
2. Neurologic injuries—Injury to nerves from simple mechanical displacement produces neurologic injury, most commonly axonotmesis. Complete disruption of the nerve (neurotmesis) can occur but is much less common. The peroneal nerve is most commonly involved (20% of all KDs) and is most commonly associated with lateral-sided injuries (KD-IIIL) or a posterolateral KD. Tibial nerve involvement is rare, but can be seen with vascular injury. Loss of protective sensation of the foot (the sole of the foot) with a complete tibial nerve injury associated with a vascular injury may result in amputation. In contrast, peroneal nerve involvement is a functional problem from the motor abnormalities and is frequently a significant factor in the patient’s disability.

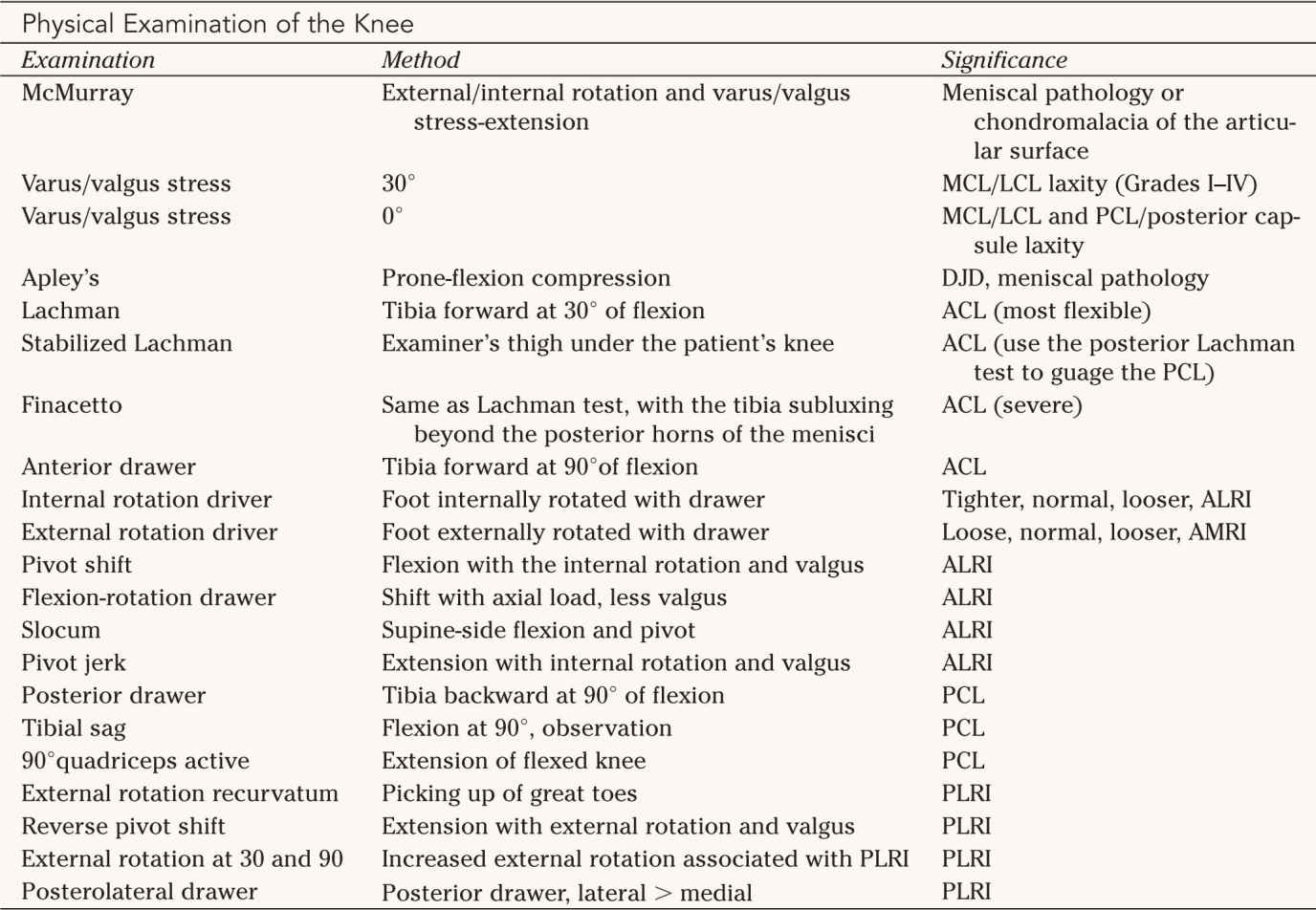
MCI, Medial collateral ligament; LCL, lateral collateral ligament; PCL, posterior cruciate ligament; DJD, degenerative joint disease; ACL, anterior cruciate ligament; ALRI, anterolateral rotatory instability; AMRI, anteromedial rotatory instability; PLRI, posterolateral rotatory instability.
Source: Modified from Miller M. Review of Orthopaedics. 3rd ed. Philadelphia, PA: W B Saunders; 2000, with permission.

3. Fractures—Joint-surface fractures of the tibia or femur create an injury best described and classified as a fracture-dislocation. Ligamentous avulsions are common in KDs and change the character of the injury and can often simplify treatment.
• Multitrauma KDs are commonly seen in multitrauma (multiple fractures severe trauma) and can be missed when there are multiple complex injuries. As noted previously, spontaneous reduction of KDs can make a multiligamentous knee injury less obvious, and careful attention during the skeletal survey is important to evaluate for a severe knee injury. Gross knee swelling in the presence of multiple trauma necessitates consideration of a dislocation, despite the presence of a reduced knee joint on radiographic evaluation. In the presence of multiple trauma, a lower threshold for arteriography may be necessary, as the treatment (i.e., immediate femoral nail fixation) in such situation does not readily allow for the observation of noninvasive studies. Furthermore, a noncooperative patient in light of a closed head injury often pushes the clinician to consider arteriography in evaluation of the vascular tree in the dislocated knee. The treatment of musculoskeletal injuries in multiple trauma is frequently prioritized, and the ligamentous management of dislocations is frequently delayed for days to weeks and follows stabilization of long-bone fractures. KDs in multiple trauma are also acceptably stabilized with external fixation, which will facilitate patient transfer and allows for visualization of the knee and extremity.
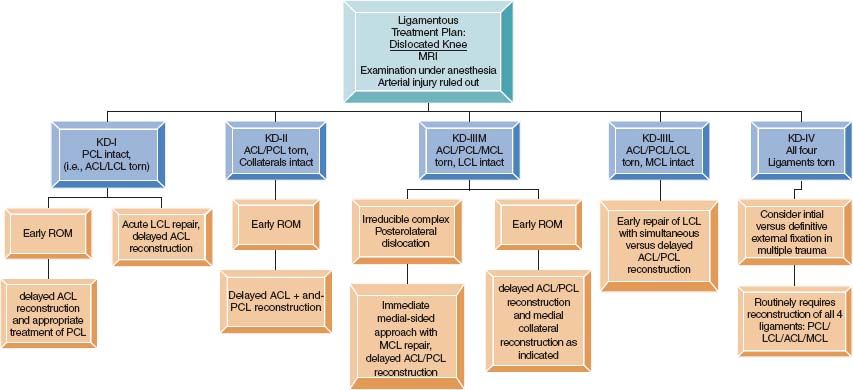
FIGURE 8-3 Suggested ligamentous management plan for KDs based on the anatomic classification system. Delayed surgical treatment is usually 6 to 8 weeks following injury or until full ROM is attained. When combining ACL/PCL reconstruction, one should tension the PCL repair before the ACL; tensioning the ACL first will result in posterior tibiofemoral knee subluxation. LCL, Lateral collateral ligament but includes structures of the posterolateral corners; MRI, magnetic resonance imaging; ROM, range of motion.
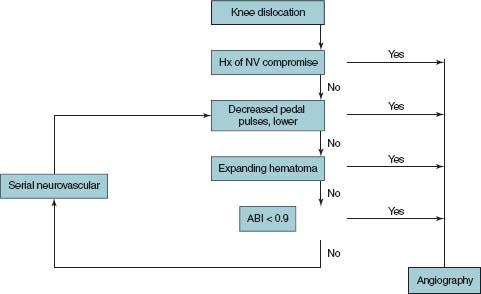
FIGURE 8-4 Suggested vascular evaluation algorithm for managing KDs.
• Microfractures—Bone bruises occur, but, in the past, have been underreported because of the need for magnetic resonance imaging (MRI) to document the injury. Chondral injuries are classified according to standard grading systems but are usually observed unless a reparable surface fracture exists.
4. Soft-tissue injuries—Soft-tissue injuries include the soft tissue envelope and the menisci.
• Soft-tissue envelope—With any high-energy or motor-vehicle trauma, the status of the soft tissues is extremely important. Even with a closed KD, the magnitude of the displacement frequently separates the knee joint proper from its attachments to the subcutaneous tissues. Gross and widespread ecchymosis, as well as subcutaneous crepitus from the soft tissue separation, is a common finding. As an aside, exploration for open ligamentous repair is frequently simplified by the underlying displacement and soft tissue injury. Open joint injuries occur, especially with high-energy trauma, and can compound the eventual ligamentous management with the need for external fixation and eventual soft tissue coverage. Open knee joint injuries from a dislocation require careful evaluation for vascular and neural injuries as a result of the degree of displacement required to cause an open injury. Treatment of an open KD requires the standard approach of debridement, pulsatile lavage, and bony joint stabilization, which frequently requires external fixation, with delayed ligamentous reconstruction.
• Meniscus—With the multiple ligamentous involvement in producing a KD, meniscal tears are variable in presentation and include displaced bucket-handle tears, peripheral tears, crush injuries with nonreconstructable meniscal damage, and coronary ligament avulsions with gross meniscal instability. Intraoperative evaluation requires inspection of both menisci and repair if possible. The inspection of medial and lateral meniscal injuries and the meniscofemoral ligaments is important.
5. Tendinous injuries—Ruptures of supporting tendinous structures about the knee are frequent and should be suspected. Avulsions or ruptures of the patellar, biceps femoris, iliotibial band, and popliteus tendons are common; the last three are usually associated with lateral sided injury. Patellar tendon injuries are problematic if missed and should be evaluated clinically with a straight leg lift, radiographs (patella alta), MRI, or a combination thereof. Quadriceps tendon ruptures can occur and are usually associated with an open injury.
6. Ligamentous injuries—Ligamentous injuries are not truly associated injuries but are the primary reason for the other injuries. As noted in the section on avulsions, ligamentous involvement in KD is usually more complex, extensive, and severe than subluxation injuries involving the isolated collaterals or cruciates.
• Specific injuries—As noted previously, KDs present with varying combinations of ligament involvement. KD (complete tibiofemoral displacement) can occur with an intact PCL or ACL. Thus it is important to clinically diagnose the ligaments torn, especially with the current well-defined clinical tests for the ligament evaluation (see Table 8-1). Clinical examination is crucial and frequently requires an anesthetic for complete patient relaxation.
(a) The cruciate ligaments—Clinically the two patterns of injury, avulsion and more commonly midsubstance tears, and multiple combinations with the collateral ligaments are seen.
• Avulsion—Avulsion can be frequently seen in high-energy trauma. Bone fragments can be associated with the avulsion, but, frequently (and especially with the PCL), the ligament is stripped from the femoral origin (“peel-off lesion”) (Table 8-2). The presence of avulsion allows for the reattachment and may avoid the need for reconstruction of the involved cruciates. The “peel-off lesion” of the PCL can be reattached with heavy, non-absorbable, braided sutures using the Krackow locking suture technique if recognized early (Fig. 8-5). Repair techniques can be performed arthroscopically, but are most easily performed open using drill tunnels and suture anchors. MRI is useful in identifying avulsions/midsubstance tears, and is especially useful for preoperative planning used in conjunction with careful EUA. EUA allows for determination of ligament function and when combined with MRI can allow for thorough preoperative planning.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






