Knee Dislocation
Volker Musahl
Russell F. Warren
Answorth A. Allen
INTRODUCTION
A knee dislocation is the most severe injury to the lower extremity. It can present as a pure soft tissue injury or as a fracture dislocation. A knee dislocation is defined as complete disruption of the femorotibial joint; whereas subluxation is defined as disruption of the joint with some remaining contact of the joint surfaces. A devastating and common complication of knee dislocation is injury to the neurovascular structures, which is reported to occur in 15% to 50% of all knee dislocations (11,27,29,35). A multiple-ligament injured knee is a knee that experienced subluxation or dislocation and has two or more ligaments disrupted (3,17,19,25). The most common clinical presentation is an occult knee dislocation; however, multiple-ligament injured knees should be treated as a “dislocated knee” even if dislocation was never witnessed (10,27).
Kennedy classifies knee dislocations according to the position of the tibia with respect to the femur. In order of decreasing incidence, knee dislocations are described as, anterior, posterior, lateral, medial, and rotatory (Figs. 39.1 and 39.2) (17). Rotatory knee dislocations are subdivided into four groups: (1) anteromedial, (2) anterolateral, (3) posteromedial, and (4) posterolateral. Up to 50% of knee dislocations are spontaneously reduced prior to evaluation and cannot be classified with the Kennedy system. Therefore, an anatomic system was developed that is based on ligament injury as well as additional designations of (C) arterial injury and (N) neural injury. Injuries are described from single cruciate tear (KD I) to involvement of all four ligaments (KD IV). Involvement of the medial collateral ligament (MCL) is designated with (M), involvement of the lateral collateral ligament (LCL) or posterolateral corner (PLC) is designated with (L). KD V involves a fracture dislocation (4).
Newer classification systems are based on surgical timing and staging. Fanelli et al. described a lateral sideand a medial side-classification system (5,8). In the lateral side classification system, a type A injury (isolated increase in external rotation) consists of injury to the popliteofibular ligament (PFL) and popliteus tendon. Type B injuries (increased external rotation and 5 mm varus laxity at 30 degrees of knee flexion) consist of injury to the PFL, popliteus tendon, and LCL. In type C injuries (increased external rotation and 10 mm varus laxity at 30 degrees of knee flexion), additional tearing of the lateral capsule occurs. In the medial side classification
system, type A injuries consist of isolated axial rotational laxity (anteromedial or posteromedial). Type B injuries consist of axial rotational laxity and additional valgus laxity at 30 degrees of knee flexion with a firm end point. In type C injuries, valgus laxity is gross with a soft end point. Surgical staging and timing according to this classification system is described later in this chapter (20).
system, type A injuries consist of isolated axial rotational laxity (anteromedial or posteromedial). Type B injuries consist of axial rotational laxity and additional valgus laxity at 30 degrees of knee flexion with a firm end point. In type C injuries, valgus laxity is gross with a soft end point. Surgical staging and timing according to this classification system is described later in this chapter (20).
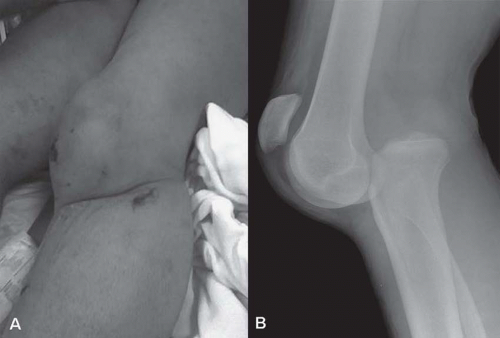
 FIGURE 39.1 Clinical presentation of an anterior knee dislocation (A) and corresponding lateral radiograph (B). |
HISTORY
Anterior knee dislocations usually result from a hyperextension mechanism (11,12,17). With increasing severity of hyperextension force, injury occurs to the posterior capsule at 30 degrees of knee flexion, followed by injury to the anterior cruciate ligament (ACL) and the posterior cruciate ligament (PCL). The popliteal artery ruptures after 50 degrees of hyperextension (Fig. 39.3) (17).
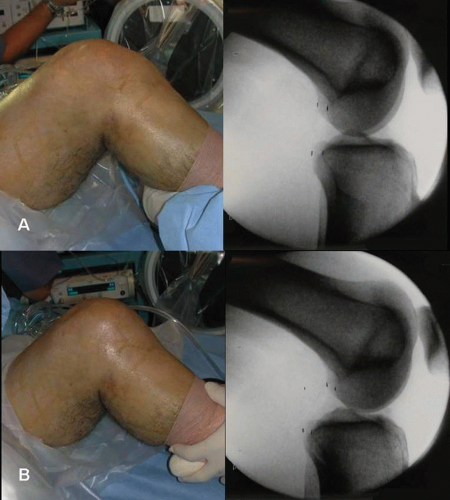
Posterior dislocations are caused by direct posterior force to the anterior tibia (11). The anterior blow to the tibia can occur while foot is fixed on the ground during contact sport or by abrupt deceleration and dashboard strike to the anterior tibia with the knee in a flexed position during motor vehicle collisions (12,30). The PCL is the most important stabilizer to posterior tibial forces and is always disrupted in posterior dislocations. Because extreme posterior loads are required to rupture the PCL, concomitant disruption of the patella tendon is common (17). The ACL is also commonly injured during posterior knee dislocations (Fig. 39.4).
Occult dislocation is a common clinical presentation and especially occurs with lateral, medial, and rotatory dislocations. These injuries are usually the result of valgus, varus, or rotatory torques, respectively (12). The incidence of lateral and medial dislocations is far less common. However, there is a higher incidence of concomitant fractures, and peroneal nerve injuries with medial and lateral knee dislocations, respectively (3,30).
Lateral knee dislocations are associated with potential for irreducibility. The irreducibility is caused by interposition of the medial capsule into the knee joint. The medial femoral condyle buttonholes through the medial capsule. The classic presentation is a patient with a grossly deformed knee and a “dimple sign” of the medial soft tissue structures. Direct surgical approaches to the invaginated tissues are preferred to facilitate open reduction.
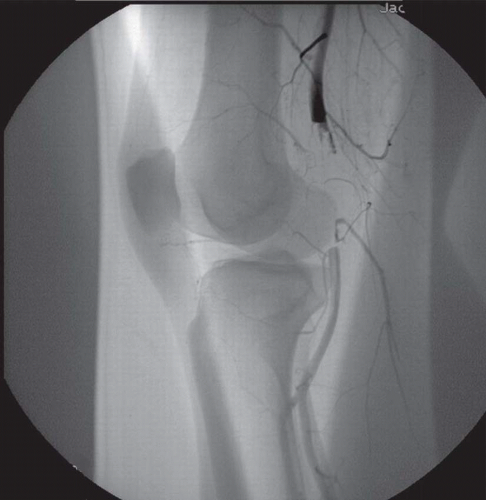 FIGURE 39.3 Arteriogram obtained intraoperatively demonstrates complete disruption of the popliteal artery. |
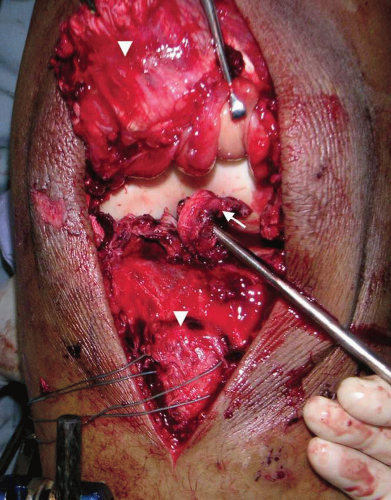 FIGURE 39.4 Intraoperative photograph of the same patient (Fig. 39.3) demonstrating complete disruption of the patella tendon from the tibial tubercle (arrow heads) and complete disruption of the ACL (arrow). The patella tendon was repaired with transosseous sutures in Krackow technique. The ACL was staged reconstructed. |
MANAGEMENT
The initial management of knee dislocation is dependent on the clinical setting. Patients who present with a dislocated knee to the trauma center will be managed according to advanced trauma life support guidelines. The knee must be reduced in a timely fashion to prevent further injury to neurovascular structures and associated injuries to the soft tissue compartments. After stabilization of the patient in the trauma center or upon initial evaluation of a patient with occult knee dislocation in the office, it is recommended to follow a management algorithm.
1. The adequacy of reduction must be documented. Radiographs in two planes (anterior-posterior and lateral) should be obtained. In cases where closed reduction cannot be achieved, that is, lateral knee dislocation with interposition of soft tissues, open reduction should be performed emergently. If adequate reduction can be achieved but not maintained by noninvasive means, external fixation may be necessary to assist in maintaining the reduction of the knee. Surgical repair of damaged ligaments and tendons should be performed as soon as the patient’s general condition will allow (ideally within 7-21 days).
2. Vascular examination. Perfusion of the distal extremity needs to be assessed carefully in every case of suspected knee dislocation. Physical examination includes hard signs of vascular injury, such as absent distal pulses, active bleeding, distal ischemia, expanding hematoma, and popliteal bruit or thrill. Presence of any of these findings denotes limb-threatening injury and mandate immediate exploration by a vascular surgeon (1,22). Arterial blood flow must be reestablished within 6 hours of the injury to prevent ischemic effects that would lead to amputation in the majority of cases. Patients with normal pedal pulses may be managed with observation and frequent monitoring by physical examination, ankle-brachial indices, or waveform assessment on Doppler evaluation. Arteriograms are obtained only when abnormal physical examination findings exist (20).
The incidence of popliteal artery injury is reported from 5% to 40% (11,16). Anterior dislocation usually results in a traction injury to the popliteal artery as the vessel stretches and is introduced into the intercondylar notch. This traction injury often results in intimal tears. In general, low-velocity injuries tend to be associated with fewer vascular injuries (27,29), whereas high-velocity injuries are reported to produce a greater incidence of vascular complications (35). Intimal flap tears are injuries to the endothelial lining of the arterial wall. They are often undetectable by physical examination and usually require an arteriogram for diagnosis. Potter et al. described popliteal fossa magnetic resonance angiography (MRA). In their series, a 100% correlation between MRA and arteriogram was found in six patients after knee dislocation (23).
3. Neurological examination. It is important to document any sign of peroneal nerve injury preoperatively. Peroneal nerve palsies have been noted to occur in 14% to 35% of knee dislocations (15). The most common occurrence is in posterolateral dislocations a result of traction injury as the nerve is stretched along the posterior aspect of the lateral femoral condyle (17,28). Recovery of function after peroneal palsy associated with knee dislocation has a guarded prognosis. The energy of this insult to the nerve usually results
in axonotmesis over a large segment of the nerve (35). Nerve grafting, rather than primary repair, is often required because of the long segment of injury.
in axonotmesis over a large segment of the nerve (35). Nerve grafting, rather than primary repair, is often required because of the long segment of injury.
4. Condition of the soft tissues. In open knee dislocations, surgical irrigation and debridement must be performed at the earliest opportunity. Healing of the soft tissue envelope is then monitored prior to attention to the ligament injuries. It is recommended to adhere to the same algorithm in cases of closed knee dislocation with severe blunt injury to the soft tissue envelope and skin. A high index of suspicion for compartment syndrome is important.
5. Physical examination. At this point, a thorough assessment of alignment, range of motion, extensor mechanism, and knee ligaments is performed. Because of pain, guarding, ipsilateral fractures, or altered mental status the physical examination may not be reliable. However, a knee that can only move from 10 to 45 degrees may still enable the surgeon to obtain useful information for preoperative planning. The integrity of the extensor mechanism can be assessed by a simple straight leg raise test. A minimal effusion in the face of a severe multiligamentous injury may give a clue to a capsule injury with extravasation. Compartments can be assessed. With a pillow under the knee, the Lachman test can be performed with reasonable sensitivity. The position of the anterior tibia with respect to the femur can be assessed at 45 to 60 degrees of flexion and reveal if there is normal (1 cm) anterior tibial step off or sag (Fig. 39.5). With the leg on the stretcher, a varus and valgus stress test can be performed to assess the integrity of the LCL and MCL, respectively. While
the dial test at 90 degrees of flexion may not be possible, increased tibial external rotation at 30 degrees of flexion raises the suspicion for PLC injury (Fig. 39.6).
the dial test at 90 degrees of flexion may not be possible, increased tibial external rotation at 30 degrees of flexion raises the suspicion for PLC injury (Fig. 39.6).
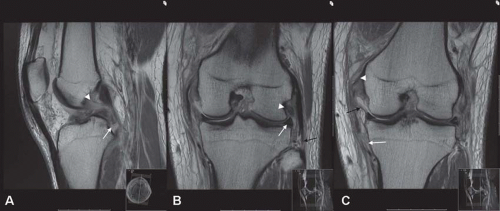 FIGURE 39.7 A: Sagittal fast spin echo MRI demonstrating complete tear of the ACL (arrow head) and partial tibial sided avulsion of the anterolateral bundle of the PCL (arrow). B: Coronal fast spin echo MRI demonstrating extrusion of the lateral meniscus (arrow), avulsion of the LCL off the fibula (black arrow), and intermediate signal in the popliteus tendon indicating interstitial injury (arrow head). C: Coronal fast spin echo MRI demonstrating complete tear of the tibial sided MCL (arrow
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|