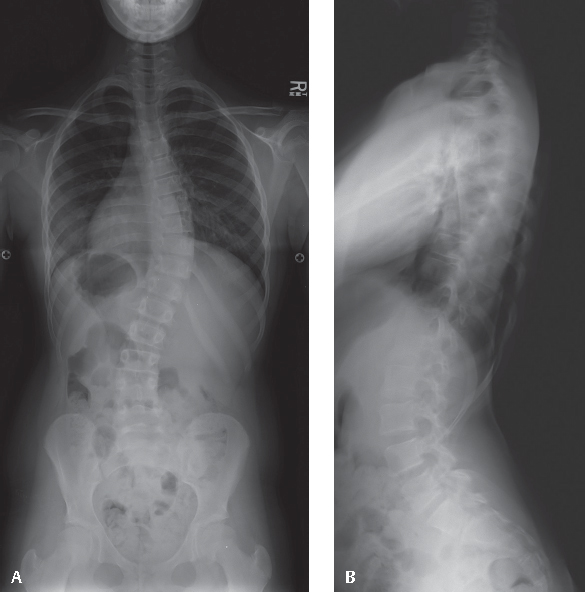
38 Juvenile idiopathic scoliosis (JIS) is defined as scoliosis with onset between ages 4 and 10 years. By definition, the term implies a lack of identifiable cause.1,2 Once the diagnosis of scoliosis has been made, the differential diagnosis in this age group also includes congenital scoliosis (scoliosis resulting from malformed vertebral elements), neuromuscular scoliosis, scoliosis in association with a genetic syndrome, and scoliosis secondary to spinal cord pathology. The diagnosis of JIS is, therefore, one of exclusion. Approximately 20% of patients with juvenile-onset scoliosis will have an identifiable abnormality of the neural axis, and approximately one-half of these will require surgical intervention directed toward the neuraxis abnormality.3 The evaluation should include a detailed family history and review of systems to identify disorders known to be associated with scoliosis. Neurologic symptoms, such as weakness, fatigue, balance or gait disturbance, and changes in bowel or bladder habits, should be elicited. The presence of back pain may indicate underlying neural axis pathology, particularly in young patients. Physical examination of the child with juvenile-onset scoliosis includes evaluation of trunk shape (including scapular position, shoulder height, and trunk rotation, assessed by forward bending), coronal and sagittal balance (including trunk shift, lordosis, and kyphosis), limb length (including pelvic obliquity), skin markings (particularly those overlying the spine), and associated skeletal abnormalities or dysmorphisms. Spinal flexibility should be assessed, as diminished range may be due to pain, muscle spasm, and/or hamstring tightness that may indicate underlying spinal pathology. Gait should be observed, paying particular attention to balance, coordination, and muscle strength. Subtle posturing of an extremity may become more apparent when the child is running. A detailed neurologic examination should focus on upper- and lower-extremity strength and sensory function, as well as deep tendon and abdominal reflex testing, Babinski reflex testing, and evaluation for clonus. Full-length posteroanterior (PA) and lateral spinal radiographs obtained in the standing position are required for the initial evaluation of scoliosis to enable measurement of the curve magnitude and to screen for congenital scoliosis or an acquired lesion. PA, lateral, and oblique radiographs of the lumbosacral spine may also be indicated if spondylolysis and/or spondylolisthesis is suspected by the presence of low back pain, posterior thigh pain, hamstring spasm, abdominal creasing, and/or atypical gait (“pelvic waddle”). In young patients with an underlying neurologic cause for their scoliosis, abnormal neurologic findings on physical examination are often absent and the scoliosis itself should be considered as the presenting sign of underlying neural axis pathology. Therefore, magnetic resonance imaging (MRI) is recommended for all patients with juvenile-onset scoliosis, even if the findings of the neurologic examination are normal.3,4 This is especially important if surgical treatment of the scoliosis is contemplated. The treatment of JIS follows guidelines that are similar to those for adolescent idiopathic scoliosis (AIS). Compared with AIS, however, JIS is more likely to progress, less likely to respond to bracing, and more likely to require surgical treatment.5 In general, observation is warranted for curves measuring less than 20 to 25 degrees, with physical examination and standing PA spinal radiographs performed every 4 to 6 months. Documented progression or curvature measuring more than 25 to 30 degrees at presentation is typically managed with a spinal orthosis. If curve progression is demonstrated despite brace treatment, the brace may be utilized to help slow progression until the child is older, to avoid surgical creation of a short trunk or the “crankshaft phenomenon,” in which subsequent spinal deformity occurs as a result of continued anterior spinal growth in the face of posterior surgical fusion.6 Neither observation nor brace treatment is warranted, however, in rapidly progressive curvature and/or severe spinal deformity (> 50 degrees), for which surgery is indicated. Surgical options can include the use of spinal instrumentation without fusion, the so-called “growing rod” technique.7 This technique requires subsequent rod lengthening every 6 to 12 months until adequate trunk size is achieved, at which point spinal fusion is indicated. This technique has gained considerable popularity, although a high complication rate appears to be associated with the subsequent lengthenings.8 In younger children with JIS (usually ages 4 to 5), convex hemiepiphysiodesis can also be considered and can be added to the growing rod procedure when indicated. For older children with JIS (usually age 8 to 10 years), posterior spinal fusion with instrumentation can be performed, with the addition of anterior apical growth arrest to avoid the crankshaft phenomenon9 (Figs. 38.1 and 38.2). Anterior fusion with anterior spinal instrumentation for select thoracic curvatures, utilizing open or thoracoscopic techniques, is another option, as it can address issues of crankshaft phenomenon and hypokyphosis (thoracic lordosis) simultaneously.10 Fig. 38.1 Ten-year-old, premenarchal female with juvenile-onset idiopathic scoliosis. (A) Pre-operative standing posteroanterior spinal radiograph demonstrating a 55 degree thoracic curvature from T5 to L1. The triradiate cartilage is just closing, and the iliac crest apophyses have not begun to ossify (Risser 0). (B) Preoperative standing lateral spinal radiograph demonstrating mild thoracic hypokyphosis and rib prominence.
Juvenile Idiopathic Scoliosis
![]() Classification (Etiologic)
Classification (Etiologic)
![]() Workup
Workup
History
Physical examination
Spinal Imaging
![]() Treatment
Treatment
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






