Joint Salvage and Preservation Surgical Techniques for Hallux Limitus
Annalisa Y. Co
Thomas J. Chang
Craig A. Camasta
Although conservative treatment may be helpful in the early stages of hallux limitus, many patients warrant surgical intervention (1). Often, attention is directed solely toward the osseous deformity, to affect the overall alignment of the joint. The soft tissues also play a vital role in limitation of joint motion.
The surgical approaches to joint preservation procedures are varied, but several goals are shared. Relief of excessive joint tension is required (2). If excessive joint compression is present and is not alleviated, hallux limitus will return, often worse than before. Structural correction of the first metatarsal often assists in achieving this goal. The second key principle is to ensure that mobility of the plantar joint structures is adequate. In reality, one cannot ensure relief of joint tension without providing mobility of the sesamoids and flexor apparatus. Preoperatively, sesamoid and flexor plate mobility may be evaluated by pulling the plantar fat pad distally and placing a thumbnail against the distal margin of the sesamoid (2). With the surgeon’s thumb in that position, the hallux is passively dorsiflexed. The movement of the thumb indicates the degree of mobility of the flexor plate. Finally, orthotic control may be necessary to provide a supportive environment for maintenance of joint function.
The approach to joint salvage focuses on the local deformity at the first metatarsophalangeal joint (MTPJ), with the understanding that proximal deformities need to be adequately controlled. The proximal deformities that need to be addressed may require procedures such as release of posterior equinus or medial column stabilization. At the level of the first MTPJ, the approach begins with the initial soft tissue release and cheilectomy. Afterward, the first ray may then be further evaluated to determine which, if any, additional measures will be required to provide the best correction.
CHEILECTOMY
Cheilectomy is the removal of the osteophytic proliferation about the metatarsal head and/or the proximal phalangeal base. This technique was first described by Nilsonne (3) and served as only a temporary treatment at that time. This is the first step in the repair of hallux limitus for most patients. The normal gliding function of the joint is absent in hallux limitus and is replaced by a rocking motion that produces intermittent bone-on-bone impingement at the dorsal margins of the joint. Hypertrophic bone formation and fragmentation result from this chronic microtrauma. This process eventually blocks dorsiflexion and can become painful even without shoe pressure.
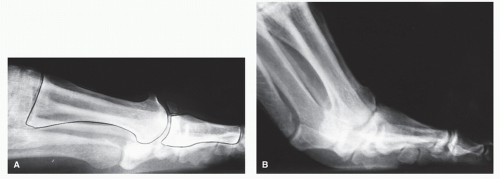
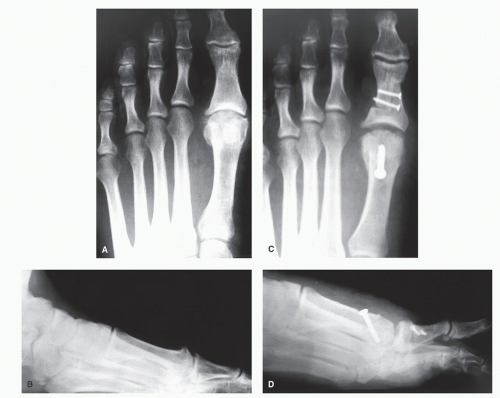
Cheilectomy may also be employed as a sole procedure in the repair of hallux limitus when no metatarsal deformity is present (Fig. 33.1). In general, favorable results have been reported (4,5 and 6), although some authors have recommended resection of one-fourth to one-third of the metatarsal head to avoid recurrence (4,7). Aggressive cheilectomies have been reported, characterized by removal of one-half to two-thirds of the dorsal aspect of the metatarsal head. Removal of this large a segment of bone is beyond the scope of cheilectomy, which serves to restore normal anatomy, and is more accurately termed an arthroplasty.
EVALUATION/DIAGNOSIS/FUNCTIONAL ANATOMY
The applications of cheilectomy alone are limited. A dorsal exostosis in addition to medial, lateral, and maybe proximal phalanx base bony proliferation can usually be visualized clinically and/or radiographically. A limitation in dorsiflexion of the first MTPJ with a hard block is typical. The patient should have only minimal erosive or degenerative changes within the joint, and the central regions of the hyaline surfaces should be mostly intact.
CONTRAINDICATIONS
If there is deformity to the first metatarsal such as metatarsal elevation, additional procedures in addition to the cheilectomy should be utilized. The etiologic factors involved in creating the hallux limitus should be amenable to supportive measures postoperatively. Otherwise, the duration of improvement may be relatively brief. Subsequent procedures are often required in patients with more advanced joint degeneration after cheilectomy alone.
TECHNIQUE
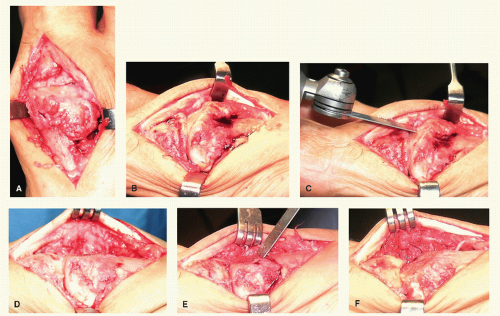
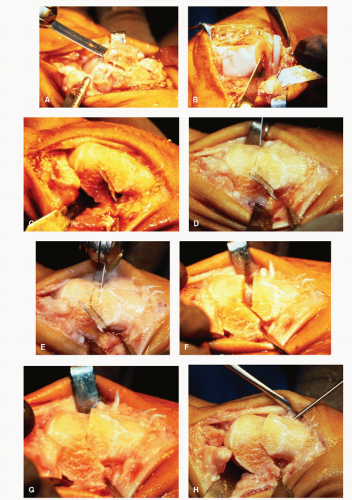
The approach to the joint is generally through a dorsomedial incision. A rectus hallux does not require capsular modifications that decrease joint volume. When the normal anatomy of the metatarsal head is altered, the hypertrophic bone should be remodeled. Generally, the amount of proliferation seen surgically is large compared with the appearance on radiographs, inasmuch as the outer portions of the exostosis may be largely cartilaginous. The resection involves the dorsal, dorsomedial, and dorsolateral corners of the joint. True cheilectomy does nothing more than reestablish normal anatomic contours to the osseous structures (8). If the joint range of motion remains to be significantly limited or blocked after the initial cheilectomy, a more aggressive resection from both the dorsal metatarsal head and proximal phalanx can be achieved by slightly angling the exostectomy dorsal to plantar toward the joint (Fig. 33.2). The articular surfaces should be inspected for
gross arthritic changes both on the metatarsal head and on the proximal phalanx. A satisfactory quality of motion should be noted. When indicated, abrasion arthroplasty or subchondral drilling techniques may be recommended to encourage fibrocartilage repair of defects (9) (Fig. 33.3). Caution should be used if both the proximal phalanx base and metatarsal head are significantly arthritic because drilling both surfaces may lead to a postoperative pseudoarthrodesis.
gross arthritic changes both on the metatarsal head and on the proximal phalanx. A satisfactory quality of motion should be noted. When indicated, abrasion arthroplasty or subchondral drilling techniques may be recommended to encourage fibrocartilage repair of defects (9) (Fig. 33.3). Caution should be used if both the proximal phalanx base and metatarsal head are significantly arthritic because drilling both surfaces may lead to a postoperative pseudoarthrodesis.
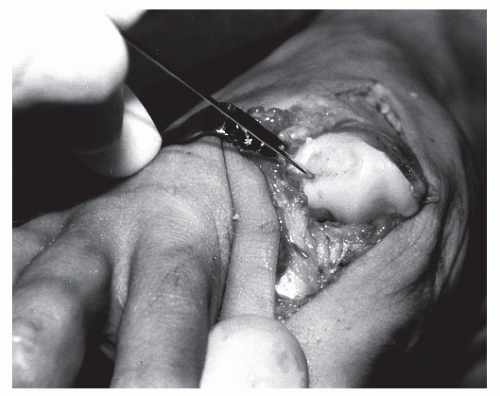 Figure 33.3 Technique of subchondral drilling in an attempt to encourage fibrocartilage regrowth into the cartilage defect. |
After resection of the hypertrophic bone and treatment of eroded cartilage, the sesamoid apparatus should also be inspected. Banks and McGlamry (2) described the importance of the flexor plate in hallux limitus. If mobility of the sesamoids and flexor plate is questionable, the flexor plate can be freed by sharp dissection or by use of the McGlamry metatarsal elevator. Sesamoid shape and position can also affect the mobility of the joint. Partial resection of a hypertrophic or proximally elongated sesamoid often allows the metatarsal head to plantarflex more predictably and to maintain hallux motion. When severe adhesions or arthritic changes of the sesamoids are present, a different surgical approach is indicated, possibly involving removal of the arthritic sesamoid.
The range of motion should again be evaluated after capsular release, cheilectomy, and sesamoid release. If structural deformity of the metatarsal is determined to be present or the range of motion after completion of the cheilectomy is still not adequate, then an osteotomy should be considered.
Weight-bearing is permitted immediately in a surgical shoe. Gentle passive range-of-motion exercise is started early in the postoperative phase.
COMPLICATIONS
Potential complications after cheilectomy are minimal. If there is extensive arthrosis or metatarsal pathology, a cheilectomy should be part of the surgical intervention. If the cheilectomy is used alone, any postoperative relief can be brief and additional surgery may be warranted.
DISTAL METATARSAL OSTEOTOMIES
Distal osteotomies are primarily used to help decompress the first MTPJ in hallux limitus or when the patient appears to have minimal or mild metatarsal primus elevatus. The goals should include shortening and plantarflexion of the capital fragment (2). Rotation of the capital fragment may also be considered when dorsal articular cartilage is absent. The most important structural change is shortening of the metatarsal, a maneuver that effectively relaxes the plantar structures and decompresses the joint space to provide for increased range of motion. This will produce an improved mechanical environment for joint function. Most of the distal osteotomies are inherently stable in their design.
WATERMANN OSTEOTOMY
Indications
The Watermann osteotomy is a dorsally based closing wedge that serves to derotate the intact articular cartilage dorsally and mildly shortens the first metatarsal, allowing joint decompression. The Watermann procedure can also be employed when a double osteotomy is necessary in surgically treating hallux limitus. Most of the proximal plantarflexory osteotomies employed in moderate to severe metatarsus elevatus result in rotation of the capital fragment in the sagittal plane. This change places the final position of the articular cartilage in a slightly plantar position. Although the range of motion of the first MTPJ may improve, the actual amount of functional cartilage available when the hallux purchases the ground is decreased. A Watermann procedure may be helpful derotating the cartilage into a more functional position. This theory is analogous to employing a double osteotomy (Logroscino) for a hallux valgus deformity (10).
Technique
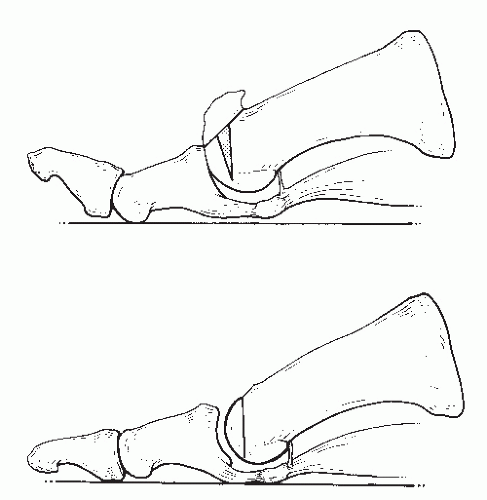
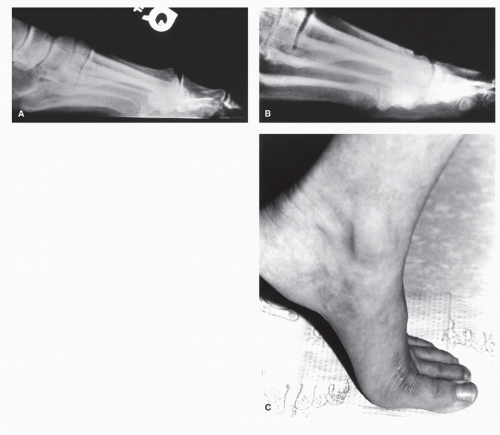
After the initial soft tissue release and cheilectomy, attention is directed to the first metatarsal head. The original Watermann procedure consisted of the removal of a trapezoidal wedge of bone from the first metatarsal head with its base dorsally (Fig. 33.4), to redirect the effective motion of the joint to allow more dorsiflexion of the hallux (11). Although not discussed by the original author, a second important effect is produced as a result of the intracapsular nature of the osteotomy. The internal cubic content within the joint is reduced, thereby relaxing capsular and periarticular soft tissues and permitting an increase in joint motion, provided sesamoid mobility is adequate. When a dorsally based piece of bone is removed, the dorsal cortex of the first metatarsal is also shortened. This tends to alleviate some of the jamming of the joint that occurs at the end range of motion. Although internal fixation is not generally required, provided the osteotomy hinge has been sufficiently weakened to allow easy closure of the interface, some form of fixation may allow for more predictable healing. Absorbable pins or screws can stabilize this closing wedge osteotomy. Absorbable fixation may be directed through the articular cartilage into the shaft of the metatarsal.
A modification of the Watermann osteotomy can be employed using a triangular wedge of bone with the base
oriented dorsally leaving a plantar hinge and articular cartilage intact (Fig. 33.5). The sesamoids are carefully evaluated for mobility. Marked arthritic changes must not be present. If this condition primarily involves only one of the sesamoid bones, then removal may be required.
oriented dorsally leaving a plantar hinge and articular cartilage intact (Fig. 33.5). The sesamoids are carefully evaluated for mobility. Marked arthritic changes must not be present. If this condition primarily involves only one of the sesamoid bones, then removal may be required.
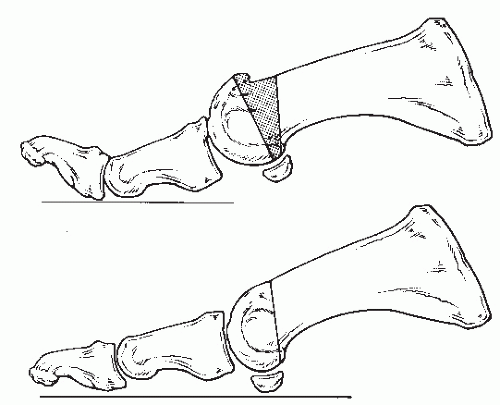 Figure 33.4 Original Watermann osteotomy involved a dorsally based trapezoidal wedge osteotomy of the first metatarsal head and neck area. |
Weight-bearing is permitted immediately in a surgical shoe. Gentle passive range-of-motion exercise is started early in the postoperative phase. The hallux may be splinted in mild dorsiflexion until radiographic evidence of bone healing is present, generally in 4 to 6 weeks. This approach facilitates compression at the osteotomy site.
Complications
Complications of the Watermann are inherent within the design of this osteotomy. Obviously, a complete osteotomy may leave the capital fragment unstable.
Because of its design, this osteotomy mildly decompresses the joint space but does not correct any structural elevation within the metatarsal. However, the redirection of forces at the first MTPJ may result in a buckling effect, so a flexible first metatarsal elevatus may be reduced to a suitable weight-bearing position.
MODIFIED GREEN-WATERMANN OSTEOTOMY
Indications
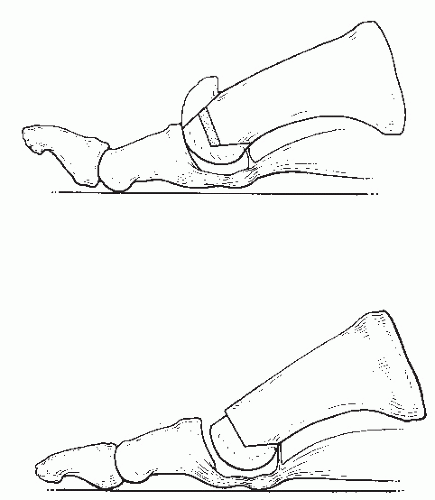
The Green-Watermann modification was devised after it became apparent that simple wedge osteotomy alone was often inadequate to relieve joint tension. Although mobility appeared to increase, in some patients, persistent binding was often noted intraoperatively at the end range of motion. The Green-Watermann osteotomy incorporates the removal of a small section of bone, to provide more dramatic relaxation of the flexor apparatus (Fig. 33.6). The procedure has been performed in conjunction with a Kessel-Bonney type of phalangeal osteotomy (12) (Fig. 33.7).
The goal of the procedure is twofold: to provide enough shortening of the bone to relieve all tension on flexor structures and at the same time to displace the first metatarsal head plantarly to avoid the lesser metatarsal symptoms that can be associated with first ray shortening. Because of the design of the osteotomy, it addresses two separate aspects of the hallux limitus deformity.
The “Watermann” name can be misleading because no actual rotation of the cartilage occurs, as seen in the traditional Watermann osteotomy.
Technique
The osteotomy is technically easy to perform and can be easily stabilized. After the initial cheilectomy approach, the initial osteotomy is made from the central portion of the metatarsal head, to form the apex, to the dorsal cortex and is oriented perpendicular to the long axis of the first metatarsal. The second cut is angulated similar to the plantar cut of an Austin procedure. The second dorsal arm is parallel to the first and is performed to remove an appropriate section of bone to create the desired amount of shortening. Critics may argue that the shortening also results in the loss of functional weightbearing length. However, by angulating the plantar cut toward the weight-bearing plane, plantar displacement of the metatarsal head occurs as the osteotomy is closed. The angulation of the plantar arm to the weight-bearing surface determines the amount of plantarflexion achieved (12,13). However, as the angle between the arms of the osteotomy increases, the inherent stability of the design decreases. A plantar arm at 45 degrees to the weight-bearing surface will result in 1 mm of plantarflexion for 1 mm of shortening (14). Any plantarflexion helps to offset the loss of length and secondarily enhances the procedure by providing some of the benefits of more proximal plantarflexory procedures (Fig. 33.8).
Fixation of the modified Green-Watermann is recommended and may consist of either absorbable or metallic fixation devices such as Kirschner wires (K-wires), staples, or screws (Fig. 33.9). The angle between the arms is approximately 120 to 140 degrees and does not provide the same stability of the osseous fragments seen with the usual 60-degree cut of an Austin procedure. If absorbable pins are used, the author recommends one point of fixation across the dorsal arm and a second point across the plantar arm. This approach has provided good stable fixation with no documented evidence of postoperative
complications. One device across the plantar arm alone, however, does not appear to stabilize the vertical portion of the osteotomy adequately.
complications. One device across the plantar arm alone, however, does not appear to stabilize the vertical portion of the osteotomy adequately.
On the contrary, one metallic device across the plantar arm is usually adequate. Smooth or threaded 0.062-inch K-wires that are bent or are cut flush with the dorsal cortex have been employed. When threaded K-wires are used, they can be driven distally and plantarly until the tip of the wire is viewed at the distal end of the metatarsal head. The wire driver is reversed, and the wire is retracted just beneath the cartilage. A flush pin cutter may then be used to cut the wire down to a length of approximately one-fourth inch. The cutter is repositioned, and the wire is then cut flush with the metatarsal. The threaded wires are left in place permanently. One wire may be adequate, whereas two wires provide extremely secure fixation. Both solid and cannulated screws are also adequate; however, the screw head may at times prove to be prominent and may require later removal. If screws are used, the surgeon must be especially careful to avoid violating joint cartilage. The configuration of the osteotomy tends to have a self-seating effect with weight-bearing and further compresses the fragments.
AUSTIN AND YOUNGSWICK MODIFICATION OSTEOTOMIES
Indications
If the patient has hallux limitus as well as an increase in the intermetatarsal angle, the standard Austin osteotomy or Youngswick modification osteotomy can be utilized. With the standard Austin procedure, correction in two planes may be obtained by simply using the appropriate axis guide. The capital fragment may be plantarflexed or shortened in conjunction with lateral transposition (15). This is ideal when hallux valgus exists in conjunction with hallux limitus.
Modifications of the Austin procedure have been described that provide shortening of the first metatarsal in addition to the lateral transposition (16,17), with an end result similar to that achieved with the modified Green-Watermann osteotomy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree