Joint Preserving Surgical Techniques for Posttraumatic Hip Disorders
Mark J. Jo
William M. Ricci
Michael J. Gardner
Introduction
Hip fractures remain one of the most common injuries seen by orthopedic surgeons. In 2007 the CDC reported approximately 1,047,000 hospital discharges related to fractures. Of those 297,000 (28%) were hip fractures (1). Although a vast majority of these fractures go on to heal uneventfully; a small subset of patients may develop posttraumatic complications (2). Although femoral head and acetabulum fractures are not as prevalent as femoral neck or intertrochanteric fractures, because of the articular damage and the higher energy typically involved in these injuries, a high percentage of these patients can go on to develop adverse outcomes. Traumatic dislocations of the hip without an associated fracture of the femoral head or acetabulum can also develop posttraumatic complications. For all fractures about the hip, even in the presence of uncomplicated fracture healing, adverse outcomes can arise. Excluding infectious complications, the most common failures related to fracture surgery around the hip are nonunion (with or without associated malunion and with or without fixation failure) and osteonecrosis. These problems can lead to debilitating pain, difficulty with ambulation and a decrease in function, and in some cases contribute to mortality.
Faced with an evolving patient population where the distinctions between young and elderly patients are blurred, treating posttraumatic complications associated with fra-ctures about the hip with procedures that can maintain the native joint and maximize the functionality of the hip is becoming more and more important. Older patients are leading healthier and more active lifestyles thus surgeons must evaluate the patient as a whole considering their preinjury activity level, medical comorbidities, cognitive level, fracture type, bone quality, and patient goals (3,4). Taking into account the physiologic age instead of chronologic age is important to help choose the correct treatment option that is best suited for that individual patient. Joint preserving treatment for fracture-related disorders can include revision reduction and internal fixation, osteotomy, and the use of different bone augmentation techniques. Despite the benefits of joint preservation, because hip arthroplasty provides a predictable outcome with a quick recovery, careful patient selection is required when considering preserving the hip joint in the management of failed treatment of fractures about the hip. In general, hip arthroplasty is reserved for those patients who are physiologically older and lead relatively sedentary lifestyles or for patients whose joint damage is beyond salvage.
Joint preserving procedures for posttraumatic conditions about the hip can be challenging for even the most experienced surgeon. Discussed will be posttraumatic disorders after acetabulum, femoral head, femoral neck, intertrochanteric, and subtrochanteric fractures. Although each may be categorized as a posttraumatic problem after fracture about the hip, each has very unique characteristics, causes, prognosis, and treatments. Therefore, a thorough understanding of how and why the initial treatment failed as well as the reconstructive surgical options available will help prepare the surgeon to address the problem, get the patient back on track to recovery, and maximize their functional capacity.
Risk Factors for Failure of Proximal Femur Factures
Treatment of fractures about the hip can lead to failure because of a myriad of factors. Some are related to the fracture itself. Extensive comminution, soft tissue injury, poor or disrupted blood supply can all lead to impaired healing (5). The fracture pattern may also be biomechanically unfavorable and therefore predisposing the fracture to impaired healing (6). Osteonecrosis can be caused by a vascular insult to the articular blood supply or a direct mechanical injury to the articular surface. Patient factors such as use of nonsteroidal anti-inflammatory drugs (NSAIDs) (7,8), tobacco (9,10), poor nutrition (11), vitamin D deficiency (12), other endocrine abnormalities, and infection can also impede fracture healing (13). Also renal failure has been shown to adversely affect fracture healing (14). Whenever identified, these issues should, if possible, be rectified or optimized. Every effort should be made to ensure that the patient is receiving adequate postoperative care and rehabilitation. Poorly monitored patients may not be compliant with postoperative weight-bearing instructions or may sustain a secondary injury such as a fall that results in
construct failure or new fracture. Fracture healing can also be compromised by technical error. Misdiagnosis of the fracture pattern, poor reduction, improper implant choice and placement can all increase the risk of failure.
construct failure or new fracture. Fracture healing can also be compromised by technical error. Misdiagnosis of the fracture pattern, poor reduction, improper implant choice and placement can all increase the risk of failure.
The morphology of the fracture can play a part in fracture healing. Because a majority of hip fractures occur in the elderly, poor nutrition and osteoporosis have a negative effect on bone quality. Biologically, the fracture milieu may not have normal capacity to heal. Furthermore, because of the limited blood supply to the femoral head, fracture displacement or comminution can disrupt blood supply and impede healing and/or cause osteonecrosis (5,15). Femoral head, acetabulum, and hip fractures seen in younger patients are usually because of high-energy injuries. The energy imparted can disrupt the blood supply to the femoral head as well as cause comminution at the fracture site (6,16,17). This comminution can predispose to either malreduction or lack of bony contact after reduction, both of which can increase the likelihood of nonunion or malunion. The different regions of the hip have different healing characteristics. Intracapsular fractures can have a lower healing rate because of the surrounding synovial fluid which bathes the fracture site impeding the healing process whereas the intertrochanteric region is extracapsular and has a broad surface area with good blood supply. The subtrochanteric region of the femur is subject to a high varus stress and is mostly cortical bone which can take longer to heal (18).
Osteonecrosis following a fracture of the hip is related to multiple factors. Initial impact at the time of injury between the femoral head and acetabulum can cause injury to the cartilage that initiates a cascade of cartilage necrosis and subsequent osteonecrosis of the femoral head or acetabulum. Vascular compromise can be caused by the disruption of the blood supply to the femoral head or soft tissue stripping of acetabular fragments. Some studies have also implicated a tamponade effect associated with intracapsular femoral neck fractures (19,20,21). Increased pressure in the hip joint from a hemarthrosis is thought to impede venous drainage of the retinacular vessels.
The use of NSAIDs, tobacco, vitamin D deficiency, poor nutrition, and endocrine abnormalities can also predispose a patient to healing problems if the underlying etiology is not addressed. Many patients may already be taking NSAIDs before their fracture occurred. Although the effects of NSAID use on bone healing has been known since the 1970s (22), there is no clear consensus or recommendations regarding their use in the setting of acute fractures. Studies have indicated that NSAID use slows time to union as well as decreases the mechanical properties of healing bone (7,8,9,10,22,23). It seems prudent that a patient at risk for nonunion should be advised to discontinue the use of NSAIDs. Postoperatively, rather than NSAIDs, patients should be advised to use oral acetaminophen or low-dose opioids for pain control (23). Recently intravenous acetaminophen has been introduced and has been shown to provide good perioperative pain control and is a viable alternative to intravenous anti-inflammatory medication (24). Ensuring the patient is receiving adequate nutrition supplementation is also vital to the success of fracture healing. Vitamin D deficiency and poor nutrition can be diagnosed using simple blood tests (12). It can be beneficial to involve geriatricians, endocrinologists, and nutrition counselors in the immediate postoperative period. It is equally important to ensure adequate follow-up after discharge so that the patients can continue to optimize their healing potential (25).
Malreduction and improper implant choice can predispose a fracture to nonunion or malunion. Malreduction with a lack of adequate bony apposition decreases the stability of the construct and puts higher stresses on the fracture and implant (26,27). Varus reduction of the proximal femur predisposes the construct to fail by increasing the sheer forces across the fracture site. Improper implant placement can also affect the reduction of the fracture (28,29). Placement of a lag screw into the femoral head distant to a center–center position has been shown to increase the risk of cutout for intertrochanteric fractures (30). Fracture patterns and patient characteristics dictate which implant gives the patient the highest chance of success. Treatment of a vertically oriented femoral neck fracture with percutaneous screws may not be sufficient to resist the sheer forces across the fracture and may require a fixed-angle device (6). Use of a cephalomedullary device rather than a sliding hip screw and plate for an intertrochanteric fracture with lateral wall comminution or an unstable fracture pattern has shown some evidence of benefit (31,32).
Evaluation of the Patient with Failed Treatment of Fractures About the Hip
History and Physical Examination
Failure of fracture treatment may be related to poor inherent capacity to heal, a poor mechanical environment to promote healing, and/or tertiary causes such as infection. Understanding the underlying reasons for failure helps to choose the most appropriate treatment. Relative functional deficits are also important factors in determining future treatments. Therefore, obtaining a history of baseline function and goals for future function are critically important to optimize treatment. These factors are most important in the elderly population who often had limited function prior to their index traumatic event, or are so debilitated at the time of presentation that return to preinjury function is unrealistic.
Malunion after fracture about the hip is common. This can be related to initial malreduction of the fracture or from secondary loss of reduction. Signs and symptoms include pain, abnormal gait, weakness, and decreased range of motion. The biomechanics of the hip has been studied extensively in the setting of arthroplasty (33,34,35). Concepts such as alterations to the neck length and offset and relative coxa vara and valgus are concepts that can easily be applied to proximal femur fractures. Excessive shortening of the neck and alterations to the offset can affect the abductor moment causing gait abnormalities and weakness. Shortening can also affect range of motion and cause greater trochanter impingement. Varus malreduction of a femoral neck fracture can lead to excessive sheer forces and ultimately lead to failure. Because of the muscle attachments about the hip and the biomechanical forces, many fractures have a tendency to displace into varus.
Many of the constructs used to treat proximal femur fractures are dynamic in nature. Their inherent ability to allow
progressive compression across the fractures site has been used to increase healing rates and decrease time to union when compared to a static device. Such dynamic constructs may result in some degree of acceptable hip deformity to allow compression across the fracture site to maximize the healing potential of the fracture (33). Uncontrolled or excessive fracture collapse can lead to excessive deformity which may alter the biomechanics of the hip beyond a tolerable range. An important factor to prevent malunion is proper reduction and appropriate fixation. Some degree of gait changes and decreased range of motion is expected following treatment of proximal femur fractures with dynamic constructs and secondary intervention is rarely necessary. In young patients, when malalignment interferes with a patient’s ability to regain their maximum potential, secondary surgical procedures may be indicated to restore anatomy and hip mechanics.
progressive compression across the fractures site has been used to increase healing rates and decrease time to union when compared to a static device. Such dynamic constructs may result in some degree of acceptable hip deformity to allow compression across the fracture site to maximize the healing potential of the fracture (33). Uncontrolled or excessive fracture collapse can lead to excessive deformity which may alter the biomechanics of the hip beyond a tolerable range. An important factor to prevent malunion is proper reduction and appropriate fixation. Some degree of gait changes and decreased range of motion is expected following treatment of proximal femur fractures with dynamic constructs and secondary intervention is rarely necessary. In young patients, when malalignment interferes with a patient’s ability to regain their maximum potential, secondary surgical procedures may be indicated to restore anatomy and hip mechanics.
The typical signs and symptoms of nonunion are a combination of pain, tenderness, and detectible motion at the site of fracture. It should be noted that symptoms of nonunion can be masked in patients with relatively stable or rigid fixation such as is seen with locked plate constructs. It is not uncommon for such patients to present with the acute or subacute onset of pain and disability associated with implant fracture subsequent to a period of full weight bearing with no or a relative paucity of symptoms. In these circumstances, the loss of stability accompanying implant failure incites the onset of symptoms. In a recent opinion poll of orthopedic trauma surgeons, the lack of ability to bear weight was felt to be the most important clinical factor in diagnosing a lower-extremity nonunion followed by fracture pain, weight-bearing status, and tenderness on palpation (36). Diagnosis of nonunion generally requires radiographic evaluation.
Posttraumatic arthritis and osteonecrosis of the hip can also be related to prior fracture. These entities are typically diagnosed with radiographic examinations. History and physical examination findings relate to progressive activity and weight-bearing–related pain and progressive joint stiffness.
Ruling out infection is generally one of the initial goals of evaluation of the patient with failure of fracture healing or failure of fracture fixation. Patient history is of little help in determining index of suspicion for infection in patients with posttraumatic problems about the hip. Since fractures about the hip are rarely open fractures, this is rarely obtained from the patient history. Local signs of infection are also often masked because of the large soft tissue envelope involved. However, a wound draining pus would certainly point to infection. Symptoms of pain can increase the index of suspicion for infection, but in the presence of nonunion or joint arthrosis, this symptom is very nonspecific. Joint aspiration, if the fracture is intra-articular, is indicated to rule out infection. This should be performed when the patient is off all antibiotics for at least 1 and preferably 2 weeks. Extra-articular fractures rely on more indirect markers of infection including serologies, namely CRP and ESR, and bone scan. Bone scan is so nonspecific that its utility in evaluation of infection associated with nonunion, is very limited. Provision for staged treatments, biopsy and culture with or without hardware removal and formal debridement as the first stage, is indicated when a high index of suspicion of infection exists. In the presence of infection, eradication of infection becomes the first priority. In the absence of infection, repair or reconstruction can be performed.
Imaging
Nonunion and Malunion
Diagnosis of a nonunion may only require clinical examination and routine radiographs. Surgeons should scrutinize postoperative radiographs and serial films for evidence of progressive displacement, change in implant position, and radiographic evidence of healing. Radiographs demonstrating an absence of callus formation or persistent lucencies may be diagnostic of nonunion. Sometimes the diagnosis of a nonunion may be more subtle; pain may be the only symptom of nonunion. Plain radiographs can be inadequate to evaluate some fractures for nonunion, especially when primary fracture healing is expected. In such instances, callus formation is not expected therefore radiographs should be scrutinized for secondary signs of nonunion. Such signs include screw migration or “windshield-wipering,” new fracture lines, and broken or loose implants. If a nonunion is suspected, a CT scan may be useful to make a definitive diagnosis or to better define the extent of fracture healing via qualitative assessment of persistent fracture lines and the amount of bridging callus. CT may also elucidate malreductions or rotational deformities that may require correction. Bone scintigraphy is useful for assessing vascularity to distinguish between a viable nonunion, one with blood flow and osteoblastic activity, or cold fracture site that does not show vascular flow nor anabolic activity of the bone (13).
Osteonecrosis
Diagnosis of posttraumatic osteonecrosis can be difficult as it may not be evident on radiographs until 6 months after the onset of the disease. And until there is collapse of the femoral head there may be no signs on radiographs. Coupled with the fact that necrotic bone can maintain its structural properties and be asymptomatic for many years, early detection and diagnosis is difficult. Pain in the groin, gluteal area, or proximal femur region are the most common complaints (37). Although MRI can detect early osteonecrosis in nontraumatic cases, the presence of metallic implants limits the usefulness of MRI and CT when diagnosing posttraumatic osteonecrosis. With more modern MRI technology and when nonferrous materials such as titanium have been used for fracture fixation, special MRI protocols can be successfully used to diagnose osteonecrosis (38). Bone scintigraphy will usually show an area of increased uptake with a central region with low signal. The low-uptake area represents the avascular necrotic area which is then surrounded by reactive bone that has increased uptake.
Posttraumatic Arthritis
The diagnosis of osteoarthritis following a fracture to the proximal femur or acetabulum can usually be accomplished with plain radiographs. Care must be taken that an accurate diagnosis is made as other posttraumatic complications can
present in a similar fashion. Because of the presence of posttraumatic changes and implants, evaluation of the joint space may be difficult. Healing callus, heterotopic ossification, and artifacts from implants may obscure the typical changes seen in osteoarthritis. Also, one must be careful not to confuse the changes seen with osteonecrosis as osteoarthritis as the treatment can be drastically different. Regardless, the mainstay of diagnosis is serial radiographs showing joint space narrowing, osteophyte formation, and sclerotic margins.
present in a similar fashion. Because of the presence of posttraumatic changes and implants, evaluation of the joint space may be difficult. Healing callus, heterotopic ossification, and artifacts from implants may obscure the typical changes seen in osteoarthritis. Also, one must be careful not to confuse the changes seen with osteonecrosis as osteoarthritis as the treatment can be drastically different. Regardless, the mainstay of diagnosis is serial radiographs showing joint space narrowing, osteophyte formation, and sclerotic margins.
Treatment of Posttraumatic Disorders about the Hip
Treatment of Hip Disorders After Acetabular Fracture
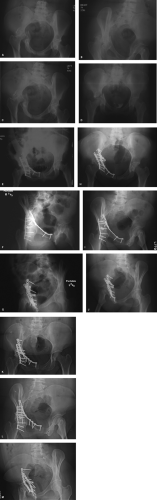
Early postoperative complications following operative fixation of acetabular fractures include malreduction and loss of fixation. Late complications include posttraumatic arthritis and osteonecrosis of the femoral head, usually in the setting of an associated dislocation. Accuracy of reduction has been shown to be a strong predictor of outcome and development of posttraumatic osteoarthritis (39). Malreduction, either primary or secondary (Fig. 59.1), can cause substantial changes on the forces across the hip and least to degenerative changes (40).
Failure of fixation is a rare complication after operative fixation of acetabular fractures and is either attributed to poor bone quality, poor compliance of patients with postoperative weight-bearing restrictions, or with improper implants. To reduce the joint reactive forces across the hip, toe-touch weight bearing is recommended postoperatively until the fracture healing has occurred. Because of the immense forces across the hip, operative strategies should maximize fixation strength by utilizing techniques such as the use of buttress plates and lag screws (41,42). Having a thorough knowledge of the pelvic bony anatomy and where
screw purchase is optimal can be vital to creating a maximally stable construct. When malreduction occurs, the type of malreduction (step or gap or a combination thereof), the age and functional expectations of the patient, and the time after injury when the malreduction is recognized are important factors dictating treatment.
screw purchase is optimal can be vital to creating a maximally stable construct. When malreduction occurs, the type of malreduction (step or gap or a combination thereof), the age and functional expectations of the patient, and the time after injury when the malreduction is recognized are important factors dictating treatment.
In general, gaps are thought to be better tolerated than step malreductions. Hak et al. demonstrated in a cadaveric model that step malreductions of transverse acetabular fractures increased joint reactive forces across the hip. They also showed that step malreductions were worse than gap malreductions (40). In cases where malreduction is recognized, the goal should be early intervention and accurate reduction. Mayo et al. (43) published a series of 64 patients with recognized malreduction of their acetabular fractures. The cases were collected from six surgeons all of whom had expertise in treating acetabular fractures. Loss of fixation was seen in 12 patients, initial malreduction in 52 patients, and retained intra-articular fragments in 14 patients. Malreduction was defined as 2 to 3 mm of step-off, joint asymmetry, or frank subluxation of the femoral head. They were able to improve the reduction in 56% of the patients and 42% of the revised patients went on to good to excellent results at 4 years. Patients with revision surgery within 3 weeks of their index procedure had a better result than those who were operated on later (44




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree