CHAPTER 8 Internal Snapping Hip Syndrome
A snapping hip, also referred to as coxa saltans, can be the result of external, internal, and intra-articular causes.1–3 In 1984, Schaberg and colleagues3 first classified the distinction between internal and external snapping hip. External snapping hip is the most common type, and is caused by the posterior iliotibial band or anterior border of the gluteus maximus slipping over the greater trochanter with hip flexion and extension. Intra-articular snapping hip can be caused by various pathologies within the hip joint, such as labral tears, loose bodies, articular cartilage flaps, displaced fracture fragments, or synovial chondromatosis.4,5 Recently, Byrd2 has suggested that the term snapping hip should only be used for extra-articular causes, because various intra-articular pathologies can be identified as causes of these symptoms.
This chapter focuses on internal snapping hip, which refers to a symptom complex most commonly attributed to catching of the iliopsoas tendon when it moves laterally to medially as the hip moves from a flexed, abducted, and externally rotated position to extension and internal rotation (Fig. 8-1).1 In 1951, Nunziata and Blumenfeld6 first described internal snapping tendon in a case series of three patients. Although the exact cause of the snapping remains controversial, it has been most often hypothesized to originate from the movement of the tendon over the anterior femoral head, joint capsule of the hip, or iliopectineal eminence at the pelvic brim.2,7,8 Less commonly, the snapping may be caused by the iliopsoas tendon sliding over exostoses of the lesser trochanter.3 Alternate theories suggest that internal snapping may be caused by the iliopsoas tendon slipping over the iliopsoas bursa—the anterior inferior iliac spine—by stenosing tenosynovitis of the iliopsoas tendon at its insertion into the lesser trochanter, or by movement of the iliofemoral ligament over the anterior femoral head and joint capsule.9 In actuality, it is likely that various patients may have different sources for their snapping. Different surgical approaches have been suggested for treatment based on the specific structure believed to be responsible for the snapping,10 although it is basically a tight iliopsoas musculotendinous unit that most agree is part of the problem.
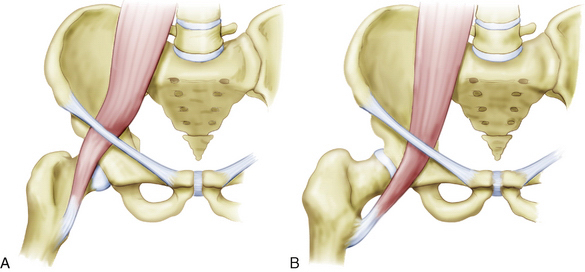

FIGURE 8-1 A & B (left to right), The proposed mechanism of snapping iliopsoas tendon. C, AP pelvic radiograph of a former soccer player with a traction spur of the lesser trochanter.
ANATOMY
The iliopsoas muscle, composed of the psoas major and iliacus muscles, is the strongest flexor of the thigh at the hip joint. It serves as an important postural muscle and prevents hyperextension of the hip joint when standing. The iliopsoas acts inferiorly to flex the trunk when rising from a supine to a sitting position. The psoas major muscle is innervated mainly by the ventral rami of L1 and L2. It has origins on the sides of the vertebral bodies, spinous processes, and intervertebral disks from T12 to L5. The iliacus muscle is mainly innervated by the femoral nerve and originates from the superior two thirds of the iliac fossa, ala of the sacrum, and anterior sacroiliac ligaments. The iliopsoas is unique in that it has both tendinous and direct muscular attachments; it first forms from the psoas muscle superior to the inguinal ligament. As the tendon runs inferiorly, it internally rotates and fans out to insert over the lesser trochanter. The iliacus tendon joins the posterior psoas tendon at the level of the pelvic brim and inserts into the body of the femur inferior to the lesser trochanter. When the hip is flexed, the iliopsoas tendon lies lateral to the center of the femoral head–anterior hip joint capsule and iliopectineal eminence. With hip extension and internal rotation, the tendon slides across the femoral head to lie medially (see Fig. 8-1).
HISTORY AND PHYSICAL EXAMINATION
Internal snapping hip has been estimated to exist incidentally in 5% of the population.2 Although the snapping phenomenon is frequently asymptomatic, in certain individuals it is accompanied by pain. Certain populations, such as ballet dancers and professional athletes, are more prone to painful snapping secondary to overuse.1,5,11,12 In one cross-sectional study, 91% of elite ballerinas reported experiencing snapping hip, with 80% having symptoms bilaterally but only 58% experiencing painful snapping. Clinical examination revealed the vast majority of these to be of the internal snapping type. The incidence of snapping hip has been noted to increase after total hip arthroplasty, often when a curved stem has been used. Usually, this can be classified as an external type of snapping hip, and it is thought to be related to catching of the posterior iliotibial band over the greater trochanter when the femoral component is placed too medially.1 With the advent of surface replacements, and the larger femoral head component, there appears to be an increased incidence of internal snapping hip following this procedure, as compared with a standard total hip arthroplasty, because the iliopsoas snaps over a more prominent acetabular component.
Internal snapping hip pain can manifest as groin pain that radiates to the anteromedial thigh and/or toward the knee. A dull ache after the snapping may be reported, and can last from minutes to hours.13 Rarely, internal snapping hip has been reported to cause pain in the lower back, flank, buttock, or sacroiliac joint.2,14 This type of pain is related to the posterior origins of the psoas (lumbar spine) and iliacus (posterior pelvis). The patient may report a history of painless snapping that has progressed to painful snapping. Internal snapping can occur unilaterally or bilaterally, and patients may or may not report a history of trauma. For internal or external snapping hip, the reported history of trauma is often minor and/or remote, whereas an acute history of significant trauma is often associated with intra-articular pathology. With intra-articular causes for snapping, patients more often report an intermittent clicking rather than a snapping sensation.
On physical examination, internal snapping hip is characterized by a painful and often audible clunk as the patient’s hip actively or passively moves from flexion, abduction, and external rotation to an extended, adducted, internally rotated position. Additional evidence to support the diagnosis of internal snapping hip can be gleaned if snapping is preceded by anterior pressure applied over the hip joint can.1,2
During the physical examination, it is critical to assess the patient for other causes of hip pain, including intra-articular causes. The Thomas test should be done to evaluate the patient for a flexion contracture of the iliopsoas or rectus femoris muscles. Patients may exhibit weak external rotation of the hip when it is in flexion and/or weak flexion of the hip while seated. Patients with internal snapping hip may also demonstrate an antalgic gait, most often externally rotated and abducted.5 The patient may also have pain and/or weakness with a resisted straight leg raise with the hip flexed at 15 degrees.
IMAGING
Plain radiographs and MRI scans are most commonly normal in patients with internal snapping hip, but they can be useful in ruling out other pathology. In patients in whom the snapping is secondary to lesser trochanter exostoses, synovial osteochondromatosis, or intra-articular loose bodies, there may be characteristic findings on plain films (see Fig. 8-1C). MRI can yield indirect evidence by demonstrating inflammation and/or swelling of the iliopsoas bursa (iliopsoas bursitis; Fig. 8-2A), or iliopsoas tendinopathy (see Fig. 8-2B). MRI is also important to rule out intra-articular causes for snapping hip, such as loose bodies and labral tears.
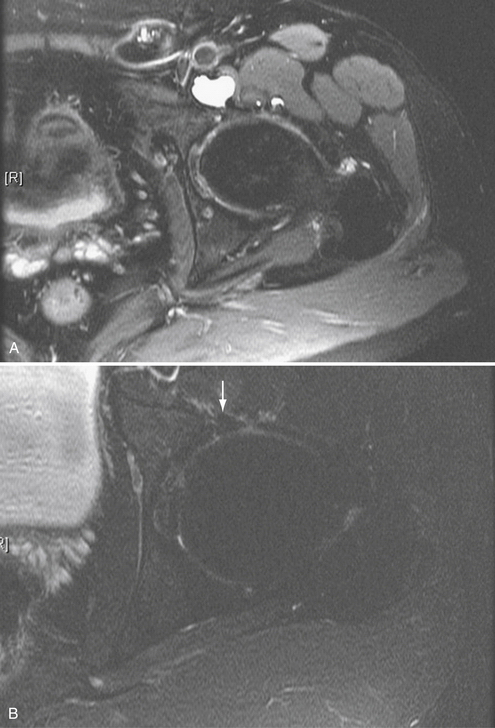
FIGURE 8-2 Axial cut MRI scans. A, Iliopsoas bursitis. Iliopsoas bursitis can accompany snapping hip. B, Professional tennis player with iliopsoas tendinitis. The arrow is pointing to the iliopsoas tendon, with the edema seen about the tendon.
Iliopsoas bursography can be a used to visualize the iliopsoas tendon catching in conjunction with the patient’s snapping.3,9,15 Diagnosis of internal snapping hip can be aided by a concomitant injection of bupivacaine (Marcaine), which may provide temporarily relief of the patient’s symptoms. Drawbacks to the use of iliopsoas bursography include difficulties associated with reproducing the snapping with the patient lying down constrained by the fluoroscopic imager located above the hip.2
The limitations of iliopsoas bursography can be overcome through the use of dynamic ultrasound to demonstrate the catching of the iliopsoas tendon.16 This technique allows for a greater range of motion at the hip to reproduce the snapping sensation. Other evidence in support of the diagnosis of internal snapping hip includes thickening of the iliopsoas tendon and peritendinous fluid collections. A diagnostic injection of bupivacaine can also be used with dynamic ultrasound to check for alleviation of symptoms. Disadvantages of dynamic ultrasound include the fact that results are technician-dependant, and its success also requires a high-resolution ultrasound machine.2
TREATMENT OPTIONS
Conservative Management
In most cases, internal snapping hips are asymptomatic and hence require no treatment other than reassurance. Patients should be counseled that painless internal snapping is a normal variant, and is not a sign of current or future pathology. For painful internal snapping hips, the first step is activity modification to avoid the movements that cause pain. Additionally, physical therapy, focusing on stretching and gentle strengthening of the hip flexors and abductors, and core stabilization may prove beneficial to some patients.1,14,17 Nonsteroidal anti-inflammatory drugs (NSAIDs) are used to decrease pain and inflammation. The vast majority of symptomatic patients are successfully treated with conservative management. However, it can take several weeks before symptoms begin to improve, and several months to 1 year before pain resolves and normal function is regained. For athletes, the goal of treatment is to be pain-free prior to returning to sports. Corticosteroid injections into the iliopsoas bursa can also be used as an adjunct for patients who do not respond to the measures described.









