Internal Impingement
James R. Andrews
Patrick J. Casey
INTRODUCTION
Overhead athletes subject the shoulder to tremendous forces and stresses during competition. Extreme external rotation with the arm abducted 90 degrees is required to generate the appropriate force to pitch a 90-mph fastball, serve in tennis, or hit a winner in volleyball. In particular, during the late cocking phase of throwing, the arm can require 170 to 180 degrees of external rotation to generate the torque required (1,2) (Fig. 9-1). Moreover, the shoulder is one of the least constrained joints in the human body with the glenoid and labrum combined surface area totaling only 28% of the humeral articular surface area (3).
During the acceleration phase of pitching, the shoulder joint is exposed to some of the highest forces seen in the body. A throwing athlete often generates 7,000 degrees of angular velocity per second repetitively throughout a performance (1,4). Not only does the shoulder have to generate this angular velocity, it also must dissipate this energy in the deceleration phase of throwing. The arm position and force required to create such acceleration can lead to pathology in the shoulder over the course of a season or career.
Internal impingement is a process by which there is repeated contact between the undersurface of the rotator cuff tendon and the posterosuperior glenoid that leads to injury and dysfunction. Internal impingement pathology is essentially an overuse injury associated with overhead athletics. With rare exception, it is not usually seen in patients unless they are high caliber athletes who perform repetitive abduction and external rotation of the glenohumeral joint. Typically, these patients have symptoms only while playing and are free of symptoms during activities of daily living. Internal impingement has only recently been recognized as a cause of pain and dysfunction in the shoulder (5). Modern understanding of this disease process and its treatment is still in infancy, even though it represents about 80% of the problems seen in the throwing and overhead shoulder in our experience.
HISTORY
Internal impingement has been well recognized as a clinical entity for more than a decade. The major tool that led to its discovery was the arthroscope. Routine arthroscopy has led to improved visualization and understanding of the glenohumeral anatomy, yielding a high amount of information with minimal invasiveness. Visualization of the posterior labrum, posterior glenoid, and undersurface tear of the rotator cuff became much improved with arthroscopy compared with the traditional open procedures.
One of the earliest descriptions of internal impingement was by Barnes and Tullos in 1978 (6). Examining 56 baseball players with shoulder pain, they described the typical symptoms of internal impingement in 24 of them. However, the authors attributed their symptoms to Bennett’s lesions (thrower’s exostoses) despite normal x-ray studies. Although they may not have appreciated the exact mechanism of injury, this was an important description of posterior shoulder pain in the overhead athlete. During the same time period, Jackson described 10 young pitchers with shoulder pain and the inability to pitch (7). He believed these players were having primary external impingement and performed subacromial decompressions on these patients. His results were fair, with just more than half returning to competition. In retrospect, he too was probably describing internal impingement in these throwing athletes.
Several years later, Andrews and colleagues published his arthroscopic findings of shoulder pathology in the throwing athlete (8,9). In the 35 pitchers who underwent shoulder arthroscopy, they found 73% had partial undersurface tears of the rotator cuff muscles (9). Andrews found this unusual considering these patients were young, healthy athletes with no history of acute traumatic episodes to the shoulder. He hypothesized that repetitive tensile forces, not contact between the posterosuperior glenoid and the rotator cuff muscles, caused these injuries.
Walch was the first clinician to correctly describe the pathogenesis of internal impingement (5). Looking at 17 throwing athletes, he found that 16 had contact between the posterior glenoid and undersurface of the infraspinatus in the abducted and externally rotated position during arthroscopy. All of these patients were young (average age 25 years) and were not thought to be at risk of tearing the rotator cuff tendons. His finding of labral wear and undersurface tearing was the first descriptions that these processes were caused by an impingement within the glenohumeral joint itself. During this same time period, Jobe did cadaveric and clinical studies demonstrating that repetitive contact between the undersurface of the rotator cuff and the posterosuperior glenoid in throwing athletes led to shoulder injury and pathology (3,10).
ETIOLOGY
The shoulder is a complex joint with multiple articulations, ligaments, and tendons involved in its kinematics. These structures generally work in concert with one another; however, if there is dysfunction in one, it may affect other structures of the glenohumeral joint. Internal impingement has an insidious onset that slowly becomes more debilitating with time as more components of the shoulder become involved. In other words, injury begets injury.
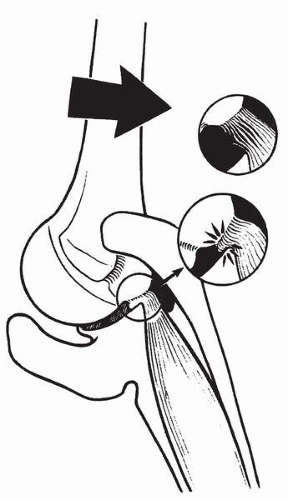
Internal impingement is caused by the repetitive contact and microtrauma that occurs to the posterior labrum and the undersurface of the rotator cuff musculature during the throwing motion (Fig. 9-2). Contact between the posterosuperior glenoid and the cuff also occurs in asymptomatic people (11). Therefore, some contact between these structures may be physiologic, but repetitive contact with altered shoulder mechanics is pathologic.
The overhead athlete who develops internal impingement tends to have repeated stress placed on the glenohumeral joint over the course of many years. These stresses often lead to adaptive changes to the surrounding tissue and altered shoulder mechanics. The structures that are most commonly involved in internal impingement include the humeral head, the anterior capsule, the inferior glenohumeral ligament, the posterior capsule, and the rotator cuff muscles.
The humeral head develops, on average, 17 degrees more retroversion in a throwing arm than the nondominant side (12). This is likely secondary to the repetitive torsional stresses seen to the physis during juvenile development. Increased retroversion provides greater external rotation in the abducted position and may be a protective mechanism against internal impingement (13). Increased retroversion does not lead to a greater total arc of motion than on the contralateral side, but it does lead to an “overrotation” of motion, which is more external and less internal rotation in the 90-degree abducted position. Patients with diminished
retroversion are more likely to impinge the cuff between the posterosuperior glenoid and the greater tuberosity in the late cocking position (14). The overrotation that develops in a throwing arm allows more external rotation in the abducted position before anterior ligamentous restraint is reached. Baseball players who become pitchers after full skeletal maturity has been reached may be more at risk for development of internal impingement secondary to less retroversion of the humeral head.
retroversion are more likely to impinge the cuff between the posterosuperior glenoid and the greater tuberosity in the late cocking position (14). The overrotation that develops in a throwing arm allows more external rotation in the abducted position before anterior ligamentous restraint is reached. Baseball players who become pitchers after full skeletal maturity has been reached may be more at risk for development of internal impingement secondary to less retroversion of the humeral head.
The inferior glenohumeral ligament and anterior capsule are static restraints to forward translation of the humeral head in the throwing position. The subscapularis muscle is a dynamic restraint. With repetitive overhead motion, the subscapularis can fatigue and provide less dynamic restraint. The anteroinferior glenohumeral ligament may then be subjected to more force, which over time can lead to plastic deformation and rotational instability. That is, the repetitive throwing or overhead motion stresses the anterior capsule and causes increased laxity (15, 16, 17, 18, 19, 20, 21). Laxity of the anterior capsule can lead to both increased translation and external rotation (22). Increased anterior movement of the humeral head may exacerbate the contact between the posterosuperior glenoid and the rotator cuff (23). Normally, in external rotation, there is obligate posterior translation of the humerus that allows for more motion and less contact between the greater tuberosity and posterosuperior glenoid (24). Posterior translation prevents a mechanical block between greater tuberosity and glenoid. With laxity in the anterior capsule and subsequent loss of posterior translation, there is increased contact leading to injury.
Posterior tightness may also develop in throwers (13,25,26). Some authors believe that this posterior tightness originates from a capsule contracture and may lead to a decrease in the needed posterior translation of the humerus during abduction external rotation to avoid cuff impingement (24,27). Both posterior capsule tightness and anterior laxity have an additive effect on diminished humeral posterior translation. Again, this loss of posterior translation of the humeral head exacerbates contact between the undersurface of the infraspinatus and the posterosuperior glenoid, worsening the internal impingement. In our experience, we believe the posterior tightness may also be related to an infraspinatus or teres minor contracture isolated or in combination with the capsule itself. In some recent data from our institution (Wilk KE. Personal communication, 2000.), we have found in elite throwing athletes there can be lack of internal rotation in the 90-degree abduction position and concomitant posterior laxity. Whether the posterior tightness is due to capsule contracture, or cuff contracture, or both, the clinical manifestation is the same with diminished posterior translation and resultant posterior superior translation of the humeral head, worsening the internal impingement.
Burkhart and Morgan have suggested that internal impingement is related to repetitive posterosuperior subluxation of the humeral head in the throwing position (28,29). When in the abducted and externally rotated position, there is a torsional stress on the biceps anchor, referred to as the peel-back mechanism. Repetitive torsional stresses can lead to the posterosuperior labrum lifting off the glenoid. The end result is pathologic posterosuperior motion of the humeral head. This motion, along with the torsional stresses on the rotator cuff, leads to fatigue and failure. A recent biomechanical model (Tibone JE, MD. Personal communication.) has shown that, if a posteroinferior capsule contracture is present, the humeral head demonstrates a resultant posterosuperior subluxation, leading to internal impingement and rotator cuff failure.
The cuff muscles, which function as dynamic stabilizers of the glenohumeral joint, compensate for the changes in static restraint in internal impingement. However, while the rotator cuff tendons perform more work, they are subject to repeated articular-sided injury from internal impingement. This can lead to partial tears, tendonitis, and weakness within the cuff musculature. A cycle develops in which the rotator cuff muscles compensate for capsular changes, but in a fatigued, weakened, or injured state. The result is the injured rotator cuff muscles cannot function maximally and becomes dysfunctional as a dynamic stabilizer.
Other pathology in the shoulder may worsen or contribute to internal impingement. For example, overhead athletes are also at risk for SLAP (superior labrum anterior-to-posterior) lesions. SLAP lesions are not caused by internal impingement, but rather are the result of excess stress and contact on the biceps anchor. SLAP lesions have been found to increase anterior translation of the humeral head up to 6 mm (30). That is, SLAP lesions lead to further loss of static restraint. In one biomechanical study, loss of the biceps anchor resulted in an increase in 100% strain on the inferior glenohumeral ligament (1). This increase in anterior translation may worsen the contact and stresses seen on the posterior labrum and undersurface of the rotator cuff musculature (31).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree