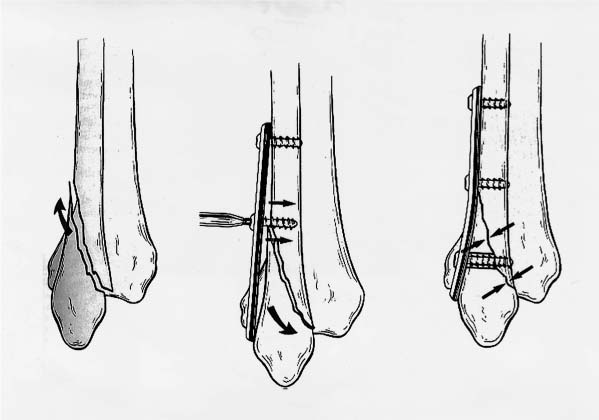
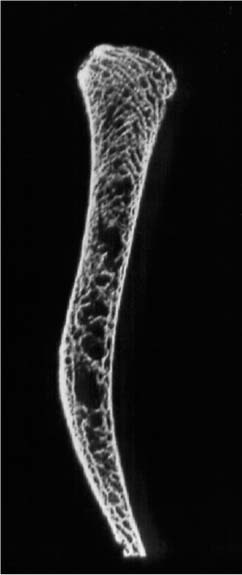
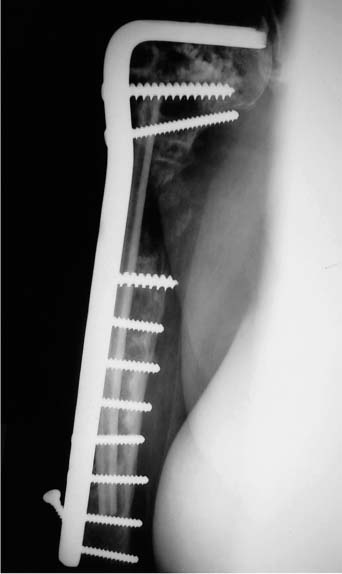
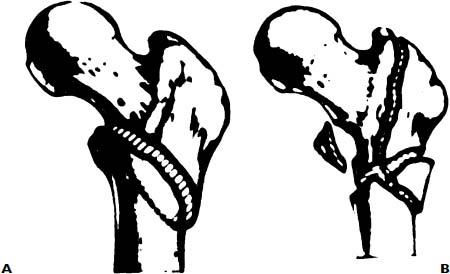
Chapter 8 The impact of skeletal loss becomes most vividly apparent as the skeleton begins to fail in its ability to withstand the required loads of everyday life. When this occurs, osteoporosis becomes a disease impacting quality of life and challenging survival. The severe economic consequences of this disorder also become reality. Osteoporosis currently affects 28 million Americans.1 With the elderly representing the fastest growing age group in the population, this epidemic grows yearly. It is believed that osteoporosis is related to 75% of the fractures that occur in the elderly.2–4 By the year 2020 there may be as many as 500,000 hip fractures annually in the United States alone. It is clearly documented that less than 50% of hip fracture patients recover fully following their injury and treatment.5,6 These statistics emphasize the need for skilled fracture care in these patients. A reasonable return of function following fracture in the elderly often requires aggressive internal fixation and rapid rehabilitation. Conversely, prolonged immobilization of the patient through nonoperative care increases the risk of thromboembolic disease, pulmonary compromise, decubitus ulceration, and further generalized musculoskeletal deterioration from which complete recovery is unlikely. The need for stable internal fixation in osteoporotic bone is paramount. In this chapter, strategies to achieve these goals will be reviewed and analyzed. Elderly patients are best served by rapid, definitive fracture care aimed at early restoration of function. In most cases, these patients are healthiest on the day of injury and are usually in the best condition to undergo surgery within the first 48 hours of their injuries.7,8 Nevertheless, many concurrent illnesses are often present and should be thoroughly evaluated prior to surgery. In some cases, judicious preoperative medical management to reverse medical decompensations causing or resulting from the injury benefits survival.8 Similarly, surgical procedures should be kept simple to minimize operative time, blood loss, and physiologic stress upon these patients. The aim of the operative intervention is to achieve stable fracture fixation that permits early return of function. For the lower extremity this implies early weight bearing. Although anatomic restoration is important for intraarticular fractures, metaphyseal and diaphyseal fractures are best managed by efforts to primarily achieve stability rather than anatomic reduction. The primary mode of failure of internal fixation in osteoporotic bone results from bone failure rather than implant breakage. Since bone mineral density correlates linearly with the holding power of screws, osteoporotic bone often lacks the strength to hold plates and screws securely.9–12 Furthermore, comminution can be severe in osteoporotic fractures. Internal fixation devices that allow load sharing with host bone should be chosen to minimize stress at the bone-implant interface. For these reasons, sliding nail plate devices, intramedullary nails, and tension band constructs are ideal for osteoporotic bone. Finally, whenever possible, the principles of biologic fracture fixation must be applied.13,14 Adherence to these principles improves the speed with which these fractures heal, improving the odds in the race against fixation failure. Resistance to pullout of a screw placed in bone is dependent upon the length of the screw purchase, the thread diameter, and the quality of the bone into which it is inserted. Recent studies have also indicated that the trabecular orientation within the bone is also important. Bone is highly anisotropic. Screws placed parallel to the trabecular pattern have greater pullout strength than those placed across the trabeculae.15 In osteoporotic bone, the variable of bone quality becomes the prime determinant of screw holding power.15–17 When bone mineral content falls below 0.4 g/cm2, the effect of varying thread diameter is lost.16 Therefore, when a surgeon plans to place screws into osteoporotic bone, he or she should strive to place screws as parallel to the cancellous trabeculae as possible and should use the largest thread diameter that is compatible with the scale of the fracture being fixed. Most importantly, he should try to secure fixation into cortical bone, if at all possible. In bone of poor quality, a smaller diameter cortical screw is definitely a superior choice over a larger diameter cancellous screw, which doesn’t secure a cortical “bite.” In cases of severe osteoporosis, the surgeon should be ready to augment screw fixation with cement.14,18–21 Polymethylmethacrylate is currently the only cement that has been used for such a purpose but calcium phosphate cements that are bioresorbable and replaced by host bone are under investigation.22–24 Polymethylmethacrylate cement has poor adhesion to bone but by intruding into the cancellous structure it results in a vastly stronger composite after the cement sets. The surgeon can predrill a screw hole, fill it with cement, allow it to cure, then redrill the hole and tap it to insert the screw; or he or she can drill, insert the cement, and follow with the screw before the cement hardens. The latter method is easier on equipment and allows the surgeon the choice of only augmenting those screws that have inadequate purchase. If this latter method is used, the surgeon should tighten the screw in the cement and allow the cement to set completely without any additional screw manipulation. Once the cement has hardened, a final tightening of the screw can be performed. Manipulation of the screw while the cement is setting loosens the bond between the cement, bone, and screw, lowering the pullout strength.20 Kleeman et al21 describe a method for use of cement, which is similar to cement techniques used for fixation of intramedullary prosthesis. This technique is most useful for situations where poor screw fixation is combined with significant bone loss.21 The security of plate fixation is affected primarily by the degree of comminution and the resulting size of any gap at the fracture site. In addition, the pattern of screw placement influences the strains experienced within the plate and its screws.25 The most important factor, which reduces strain in plated fractures, is the degree to which cortical contact at the fracture site can be achieved. Experimental fractures stabilized by plates spanning a gap experience three times the strain as fractures stabilized with secure cortical contact. In addition, for a given fracture pattern the spacing of screws is more important than the number of screws used for fixation.25 Strain within a plated construct is least when screws are placed as close to and as far away from the fracture site as possible. Intervening screws add little to the overall strength of fixation. These principles become extremely important when dealing with osteoporotic bone. When using plate and screw fixation in osteoporotic bone the surgeon must try to achieve cortical contact at the fracture site. If moderate areas of comminution exist then the fracture should be shortened to achieve contact, especially in the cortex opposite the plate.14,26–28 In essence, this principle directs us not to use plates as buttresses in osteoporotic bone unless a simple fracture pattern exists. In osteoporotic bone plates should be used as tension bands, which require an intact, load-sharing cortex opposite the plate. In osteoporotic bone longer plates with widely spaced screws should be used. In addition, the surgeon should try to place the plates to act as “antiglide plates” whenever possible. Antiglide plates are especially useful in short oblique or spiral oblique fracture patterns. In these situations the plate can be positioned to create an axilla with the cortex at the apex of the oblique tongue of the fracture (Fig. 8–1). This position of the plate acts to prevent fracture displacement, placing less importance on screw fixation, and positions the plate nicely for insertion of lag screws, which are so important for the oblique fracture pattern.14 Intramedullary nail fixation is nicely suited for osteoporotic bone, especially for diaphyseal fractures. Interlocking nails provide broad areas of purchase, allow load sharing, and provide secure enough fixation to allow immediate weight bearing.29,30 There is no question that intramedullary nailing is the treatment of choice for diaphyseal fractures of the femur and tibia.30,31 The development of interlocking nails has extended the indications for intramedullary nailing to include metaphyseal fractures as well. Mechanically locked intramedullary nails provide greater strength in axial loading than condylar blade plates, but are significantly less stable in bending and torsion when applied to the distal femur.32,33 As such, although locked nails provide less stability than condylar blade plates in simple metaphyseal fractures, they are better suited for fixation of severely comminuted fractures with no reconstructable medial buttress in osteoporotic bone. The major weakness of locked intramedullary nails is the security of the distal locking screws. The distal locking screws can easily loosen, especially within the bone of the distal femur, leading to loss of control of the distal fragment. This often results in rotational and varus/valgus malalignment. Locking screw fixation can be improved by using different planes of screw orientation34 and by using locking bolts or cement to improve fixation.14 FIGURE 8–1 The antiglide principle. The plate is positioned to create an axilla at the apex of the fracture. The distal fragment reduces into the axilla. The plate then prevents the tendency for displacement and achieves compression along the fracture line. Traditionally, surgeons have resorted to cancellous bone grafting to augment or ensure rapid and complete healing of fractures. In osteoporotic fractures, bone grafting plays several important roles. Cancellous bone grafts can be used to encourage rapid fracture healing, improving the odds of healing in the race against eventual failure of internal fixation. Cancellous bone is osteoinductive, osteoconductive, and osteogenic35 and will stimulate new bone formation periosteally, as well as in fracture gaps created by comminution. There is no current evidence that osteoporotic bone is an inferior graft material. Bone grafting is also important in osteoporotic fractures to replace regions of skeletal loss due to comminution or crush injury. Bone grafts, which are corticocancellous, can replace structural loss and as such can help restore skeletal stability in fracture constructs. This is especially true in metaphyseal and joint depression-type fractures. Osteoporosis affects regions of cancellous bone more quickly than compact, cortical bone. Metaphyseal injury with joint depression is a typical fracture pattern associated with osteoporosis. Examples include split-depression tibial plateau fractures, intraarticular fractures of the distal radius, distal humeral fractures, and calcaneal fractures. Operative repair of these injuries requires elevation of the articular surface to restore joint congruity, with the use of structural bone graft to fill in the crushed, metaphyseal void to provide support to the subchondral region. The donor source for autogenous bone graft is usually the iliac crest. The morbidity associated with the harvest of autogenous bone has recently become a concern.36 In the elderly this is a particularly important issue. Very often, the quantity and quality of bone available at the iliac crest is insufficient, requiring a larger exposure and increasing the risk of donor site complications (Fig. 8–2). Bone graft substitutes can provide an attractive alternative to autograft in osteoporotic patients.37–39 In situations of severe skeletal loss complete replacement of comminuted areas by cement is often required. Polymethylmethacrylate has been used with success, especially in supracondylar fractures of the femur.14,19 Polymethylmethacrylate has also been used in intertrochanteric fractures.40 Although polymethylmethacrylate has proven useful, it is not an ideal material for this purpose. It binds poorly to bone and can be difficult to inject accurately and to control.18 Over the long term, failure of healing and loosening of screws fixed with cement can lead to gross osteolytic damage to the surrounding bone (Fig. 8–3). Cements made from calcium phosphate have better adhesion to bone and have the advantage of being resorbed and replaced by host bone, avoiding the long-term consequences associated with polymethylmethacrylate. Calcium phosphate cements have been demonstrated to have usefulness in intertrochanteric, distal radius, and calcaneal fractures.22–24,41,42 These new cements can provide enough support to allow earlier load bearing and decrease the dependency upon the internal fixation devices. Although they are not approved for general use as yet, they will be available in the near future. It is expected that they will replace polymethylmethacrylate in this application. FIGURE 8–2 A cross-sectional radiograph of the iliac crest from an elderly osteoporotic female. The cortices are thin with little cancellous bone available for harvest as bone graft. Augmentation of the severely osteoporotic diaphysis can be accomplished using polymethylmethacrylate, but another useful approach is to place an augmentation device into the medullary canal, which can incorporate as bone or be resorbed. Fibular allograft struts can be used for this purpose (Fig. 8–4). The fibular strut improves local bone stock for screw purchase and can be incorporated to provide a span across regions of diaphyseal deficiency. MainilVarlet and colleagues have proposed use of a resorbable poly (L-lactide) material for the same purpose.43 Creative strategies such as these can be extremely successful in osteoporotic diaphyseal fractures and nonunions. FIGURE 8–3 An example of severe osteolysis that can occur following use of polymethylmethacrylate cement for augmentation of screw fixation. FIGURE 8–4 A radiograph of a nonunion of the humerus with severe bone loss. A fibular strut allograft has been fashioned into an intramedullary peg. It spans the fracture but also improves the screw purchase proximal and distal to the fracture site. FIGURE 8–5 Diagrammatic illustration of fracture patterns that have a high risk of poor outcome when treated with the standard sliding hip screw. (A) Reverse obliquity fracture pattern; (B) highly comminuted fracture with subtrochanteric extension that lacks a lateral buttress.
INTERNAL FIXATION OF
OSTEOPOROTIC LONG BONE
GENERAL PRINCIPLES OF FRACTURE MANAGEMENT IN PATIENTS WITH OSTEOPOROSIS
BIOMECHANICS OF IMPLANT FIXATION IN OSTEOPOROTIC BONE
INTERNAL FIXATION USING SCREWS
INTERNAL FIXATION USING PLATES
INTRAMEDULLARY NAILS
AUGMENTATION OF FRACTURE HEALING AND STABILITY
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree