CHAPTER 97 Instrumentation Complications
Classification of Complications
Biologic Failure
Spinal fixation and motion-preserving devices need to reside in a bioactive and mechanically challenging environment. Infection surrounding these devices can occur shortly after insertion or many years after the surgical procedure. Wound infection rates are slightly higher in the presence of instrumentation compared with noninstrumented procedures.1,2 For example, a posterior bone-only lumbar fusion may have a smaller infection rate than an instrumented fusion. The infection can be related to the presence of the hardware itself or the increased operative time associated with the instrumentation procedure. Early instrumentation systems were made from stainless steel. The advent of titanium systems theoretically will decrease the affinity of bacteria to the surface of the device.3 However, unintended wear debris may be greater with titanium implants in a developing pseudarthrosis with implant interface micromotion leading to a more robust inflammatory response.4,5 The issue of wear debris as it relates to disc arthroplasty does not seem to be as problematic compared with arthroplasty in a synovial environment.6,7 With a wide range of disc designs and arthroplasty interfaces in use in Europe and only recently approved in the United States, a definitive statement regarding wear debris cannot be made at this time.8 However, infection in the anterior lumbar interbody region can be extremely difficult to approach, drain, and reconstruct.9
The interface between spinal instrumentation systems depends on the quality of the host bone and/or vertebral endplate. Osteoporosis can lead to early fixation failure or implant loosening before an attempted arthrodesis procedure heals. Deficient vertebral endplates or subchondral osteoporosis can lead to interbody device loosening or subsidence.10–12 Motion-sparing devices rely on a solid point of fixation to the spine. Osteoporosis can compromise the interface leading to alterations in the biomechanical performance of the motion-sparing device.
Many other patient-related factors contribute to biologic failure and subsequent instrumentation complications. Steroid use, smoking, cancer, prior radiation therapy, multiple trauma, and poor nutrition are all factors than can either adversely affect a patient’s ability to heal a biologic procedure (fusion), diminish bone quality, and/or increase the risk of infection.13–21 Many of these such as steroid use, cancer, and trauma are unavoidable factors that one must encounter in the use of spinal instrumentation. Nutritional status can be assessed and improved if surgery is elective.22 Smoking cessation before spinal reconstructive procedures can improve fusion rates.16 The option should always be explored with patients. The decision of what to do if a patient cannot stop smoking before surgery is a social, ethical, and national health problem that is beyond the scope of this chapter. Needless to say, smoking is a deterrent to the success of a spinal fusion and may contribute to an increased incidence of instrumentation complications.
Biomechanical Failure
It is difficult to discuss biomechanical failure of spinal instrumentation without considering it along with an initiating problem. As mentioned earlier, an instrumented posterior fusion procedure resulting in a pseudarthrosis can lead to pedicle screw or rod breakage (Fig. 97–1).23 With any instrumented fusion, it is a race between failure of the instrumentation and healing of the fusion procedure.
Error in Thought Process
Accurate assessment of spinal anatomy leads directly to the next step of preoperative planning. Nearly every device placed in the interbody region will usually have a corresponding set of templates, corrected for varying degrees of magnification, to allow templating for the proper implant size. Threaded lumbar interbody cages are a typical implant that requires templating. Dual cages require adequate left to right spacing so that they will be well confined to the interbody region without encroachment of the cauda equina or lumbar root in the neuroforamina.24 They also need to adequately engage the superior and inferior endplates for stability and healing. Potential cage size can be determined from preoperative templating. More important, templating one size larger and smaller than the planned size will give the surgeon insight as to what may be necessary during surgery, what can be attempted should the planned cage size not be correct, and ensure that the proper implants are available at the time of surgery. Other implants/anatomic regions requiring templating on a routine basis are pedicle screws and pedicle diameter, anterolateral plates and vertebral body screws for the thoracolumbar spine, and disc replacements.
Error in Application
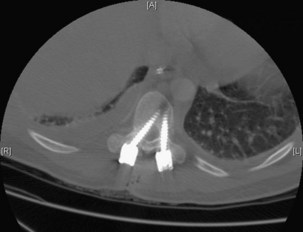
Execution of a well-designed and thought-out surgical plan is not without complication. Spinal instrumentation is no exception to this problem. Application errors can be directly linked to errors in thought process by deciding on the incorrect implant for a particular goal in a spinal reconstructive procedure. They can also include basic errors such as misplacing a pedicle screw in a pedicle. Hopefully, this would occur laterally into muscle rather than inferiorly into the foramen or medially into the spinal canal (Fig. 97–2).
Lack of intraoperative orientation to the spine can lead to application errors as well. Applying an anterolateral plate at the thoracolumbar junction requires the patient to be in the true lateral position. If the patient has rolled slightly anterior or posterior, vertebral body screws run the risk of entering the spinal canal or injuring the great vessels.25 Loss of midline orientation in the anterior cervical spine can lead to malpositioning of an anterior cervical plate and even vertebral artery injury from vertebral body screws. The surgeon must maintain his or her own three-dimensional orientation while inserting spinal instrumentation in order to prevent injury to surrounding neural, vascular, visceral, and other soft tissues. Intraoperative feedback from live fluoroscopy or image-guidance systems are not substitutes for a thorough understanding of anatomy and surgical landmarks associated with inserting different types of spinal instrumentation systems (Fig. 97–3).
Complications by Spinal Region and Implant Type
Anterior Cervical Spine
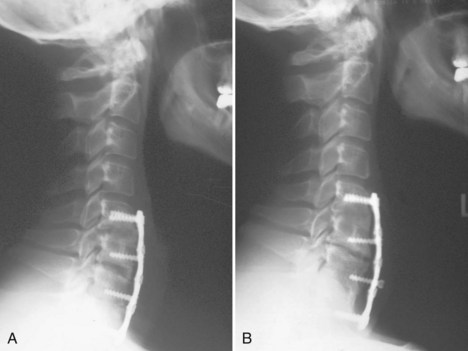
Cervical plates are the most common implants used in the anterior cervical spine. The use of buttress screws and wire has fallen out of favor over the past 20 years. Anterior plates have evolved from nonlocking, simple bone plates and bicortical screws to systems that have a locking mechanism between the plate and screw while allowing dynamic settling of the plate if the surgeon chooses this option. Contemporary systems tend to use unicortical fixation rather than bicortical screw fixation. Therefore screw penetration into the spinal canal with neurologic injury is a rare complication. Plate fracture is also quite rare. Screw back-out can still occur despite the locking mechanisms designed to prevent this problem. If this occurs, it typically represents abnormal motion at the fusion site leading to a pseudarthrosis (Fig. 97–4). Screws that back out should be removed to prevent esophageal injury, and pseudarthrosis repair should be undertaken if necessary. Occasionally, the screw-plate locking mechanism will remain intact and the plate will lift off the anterior vertebral body surface as the screw-bone interface loosens. This would also be indicative of a pseudarthrosis and should be addressed surgically. Screw breakage can occur with settling of a statically locked, anterior-plated fusion construct. If the plate remains flush with the vertebral body and the fusion heals, then a revision is typically not required.
Placement of the anterior plate can also be associated with complication. Placing the plate too lateral puts the vertebral artery at risk when drilling for and inserting screws on that side. This was particularly of concern when screws were inserted in a divergent direction. Most contemporary systems make use of convergence to minimize the risk of this occurrence. One must also evaluate each level to be instrumented for vertebral artery anomalies so as to avoid injuring the artery during drilling or screw insertion.26 Placing a plate too cephalad or caudal relative to an adjacent unaffected disc places that disc space at risk for adjacent-level ossification.27 Whether or not this represents a long-term problem remains to be demonstrated.
Anterior odontoid screws have a limited role in the overall treatment of odontoid fractures. Safe screw insertion requires a reducible fracture that is not the reverse oblique pattern, minimal bone comminution, reasonable bone quality for screw purchase, and the ability to keep the odontoid fragment from spinning while drilling and inserting the screw. Fluoroscopic visualization in the anterior-posterior and lateral planes needs to be established before the start of surgery. Patients with large/barrel chests may preclude the surgeon from obtaining a shallow enough angle to drill and insert the screw. Complications therefore include inability to insert the screw, screw cutout, spinning of the odontoid fragment and malreduction, fracture displacement, and spinal canal penetration.28
One set of complications of anterior cervical instrumentation cannot be defined on radiographs—those associated with the surgical approach and the use of power drills and taps. Care must be taken to safely mobilize the midline neck structures and protect the nerves associated with speech and swallowing function. Drill and tap sleeves should be used to prevent soft tissue injury. A common postoperative complication following anterior cervical spine surgery, dysphagia, has been linked to prolonged retractor use.29 Careful attention to adjusting retractors, working efficiently, and attempting to limit retractor time can help to reduce this complication.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree