Instrumentation
D. Scot Malay
Robyn Winner
Surgical instrumentation is highly specialized, and it has been said that there is a tool for every maneuver. In many instances, multiple instruments serve the same function, and each surgeon develops his or her own preferences. All foot and ankle surgeons should familiarize themselves with the basic set of podiatric surgical instruments. A thorough understanding of the design and proper use of the basic tools enable the surgeon to operate with comfort and proficiency.
METALLURGY AND MANUFACTURING
High-quality surgical instruments are typically made of austenitic (300 series) or martensitic (400 series) stainless steel. These iron-based alloys contain carbon, chromium, nickel, and molybdenum as essential elements in their production. The presence of carbon makes the steel extremely hard, whereas chromium primarily allows resistance to corrosion. The formation of a passive layer of chromium oxide on the surface of the alloy imparts corrosion resistance. Corrosion-resistant alloys, when properly manufactured, are capable of replenishing the inert chromium oxide layer after mechanical disruption. Repassivation spontaneously occurs when exposed chromium within the alloy covalently bonds with oxygen from the aqueous environment of the tissue fluids. The presence of the other elements in the molecular configuration of the stainless steel allows the manufacturer to manipulate the alloy’s ductility, malleability, toughness, and corrosion resistance further. When extreme hardness is required for a specific component of the surgical instrument, such as the grasping surface of a needle holder, a tungsten-carbide insert is often used (Fig. 1.1).
The most useful implantable alloy, austenitic stainless steel, is designated in manufacturing terms as 300 series alloy or, more specifically, 316LVM. Austenitic stainless steel offers superior corrosion resistance, malleability, and ductility in comparison with the harder martensitic (400 series) steel alloys. Austenitic stainless steel is ideal for the production of metallic implants, such as screws, plates, pins, and other fixation devices, because of the alloy’s ability to resist corrosion. Austenitic alloys are also used to manufacture forceps and retractors in which resilience is a necessary property of the instrument. Martensitic alloys are used to manufacture cutting instruments that must maintain sharp edges and accurate jaw alignment, such as osteotomes, scissors, curettes, and rongeurs. The combination of austenitic and martensitic alloys for specific component parts of high-quality surgical instruments is also beneficial with respect to instrument performance and durability. High-quality surgical scissors, for instance, have finger rings and handles made of 300 series alloy, blades made of 400 series alloy, and tungsten-carbide blade edge inserts.
SURGICAL BLADES
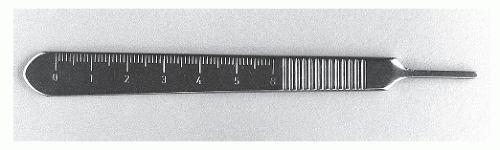
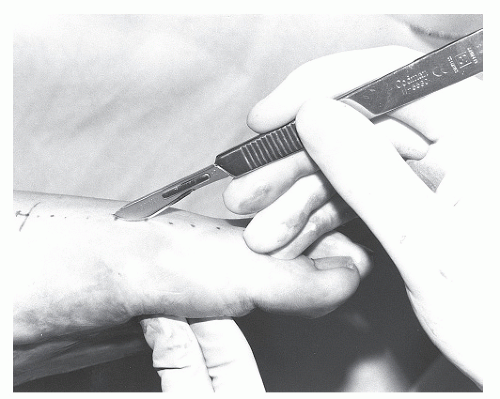
The scalpel is the instrument of choice for precise, atraumatic division of tissue. The scalpel consists of a handle portion and a blade portion. Blades may be detachable and thereby replaceable, or the scalpel may consist of a solid piece of steel that requires periodic sharpening of the blade. The handle portion of the scalpel may differ in size. The no. 3 handle is most commonly used for foot and ankle surgery (Fig. 1.2). The handle should have an engraved metric scale on one side. The scalpel can be held between the thumb and third finger, with the index finger placed along the back of the blade. This is referred to as the pencil grip and is used in foot and ankle surgery because it provides excellent control for making precise incisions (Fig. 1.3). When it is held in the reverse fashion, the scalpel handle may also be used to assist in separating the subcutaneous tissue from the deeper layers. This is commonly performed in the reflection of the subcutaneous tissue from the medial aspect of the first metatarsophalangeal joint in hallux abducto valgus surgery (Fig. 1.4).
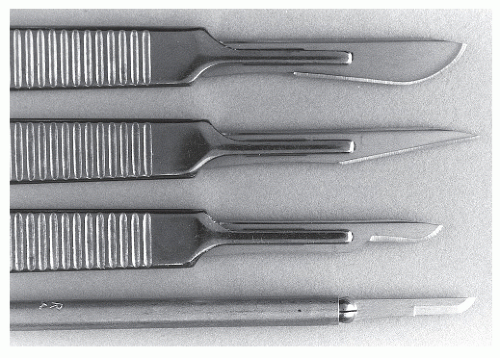
Scalpel blades are also available in various sizes and shapes (Fig. 1.5). Blades are constructed of high-quality surgical steel, with the cutting edge honed to a width of approximately 0.015 inch. The scalpel blade is designed strictly for incising tissues, and the belly of the blade should be used as the primary cutting edge. Scalpel blades should not be used for prying because they may easily break within the wound. Reversing the instrument and prying or bluntly separating with the handle portion of the scalpel may be useful. Separate blades are usually used for incising the skin and deeper tissues. The broad no. 10 blade functions well as the skin knife in most cases, although the smaller no. 15 blade may be desirable for making precise skin incisions on the digits. The no. 15 blade is also most commonly used as the deep knife. The no. 11, or bayonet, blade is useful for performing open Z-plasty tenotomy, as well as incising superficial abscesses for drainage. Some surgeons find the smaller Beaver blades (nos. 64, 67, and 81) and matching handle useful for digital arthroplasty as well as for nail plate and bed incisions.
SCISSORS
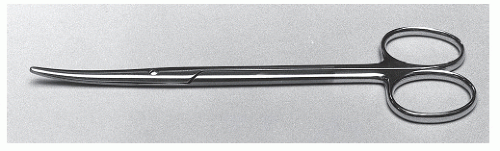
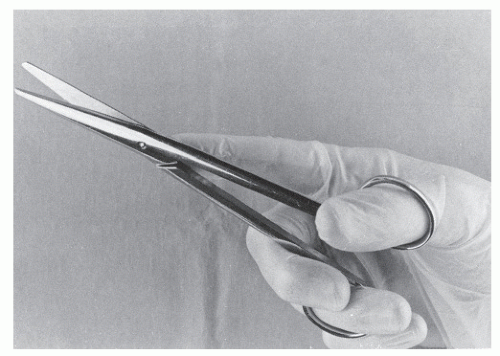
Besides the scalpel, scissors are the instruments most commonly used for tissue dissection (Figs. 1.6 and 1.7). Scissors also serve as the general-purpose instrument for cutting sutures, bandages, and other materials. Tissue scissors are finely constructed of surgical steel and are of lighter weight compared with the heavier suture cutting and utility scissors. Dissecting scissors are designed to cut soft tissues only and should not be used to cut other materials. These instruments are best grasped with the thumb and ring fingers in the finger rings, with the index finger stabilizing the hinge region of the scissors and the middle and little fingers on either side of the lesser digital finger ring (Fig. 1.8).
The blunt tips of dissecting scissors are best used for spreading and cutting tissues, and thumb forceps are usually held in the contralateral hand to manipulate tissues. The blades of the scissors should not be closed without first visualizing the tips.
Tungsten-carbide blade inserts prolong the maintenance of a sharp cutting edge. Straight blades are used near the wound surface, whereas curved blades aid in deeper dissection. The curved design of dissecting scissors enhances visualization of the cutting field, improves directional mobility, and readily allows tissue separation along smooth curves. Heavier blunttipped Mayo scissors are used for cutting thick bands of fascia and ligament; they are available with either straight or curved blades. The lighter Metzenbaum scissors have narrow, slightly curved, blunt-tipped blades that are ideal for subcutaneous
dissection and cutting lighter fascial and capsular structures. The fine cutting blades of the lightweight iris scissors are suited only for delicate tissue dissection, and careful manipulation of the sharp tips of this instrument is necessary. The short, broadblade, collar-and-crown, or Sistrunk, scissors are occasionally used for accurate dissection of osseous structures such as sesamoid bones.
dissection and cutting lighter fascial and capsular structures. The fine cutting blades of the lightweight iris scissors are suited only for delicate tissue dissection, and careful manipulation of the sharp tips of this instrument is necessary. The short, broadblade, collar-and-crown, or Sistrunk, scissors are occasionally used for accurate dissection of osseous structures such as sesamoid bones.
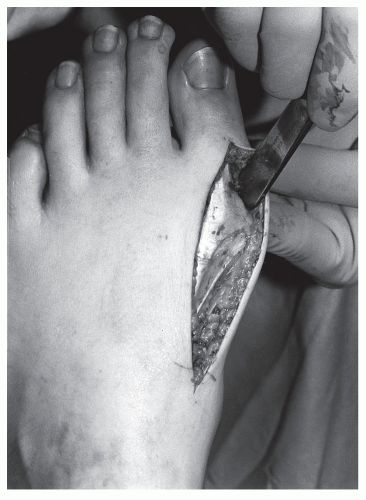 Figure 1.4 The reverse end of the scalpel may be used to help separate the subcutaneous tissue from deeper layers. |
Suture scissors usually have straight blades with blunt tips that reduce the chance of inadvertent injury to nearby tissues. When deep sutures are cut, the tips of the scissors are placed about the suture and the blades are slid down to the level of the knot; they are turned approximately 25 degrees, and, with the tips in full view, the scissors are closed. In cutting deep sutures that are under a large amount of tension, a small tag of suture should be left above the knot. A larger tag is left when one is cutting skin sutures that will be removed later. Often, general utility scissors, which come in various sizes, are used for cutting sutures. Stainless steel monofilament wire sutures are cut with wire-cutting scissors.
Bandage scissors are designed with a flat, plow-like lower blade tip that protects the patient from inadvertent injury during bandage removal. Ideally, a wound should be undressed without cutting the deep layers of the bandage. All house staff members and medical students should carry, and have readily available, a clean, sharp pair of bandage scissors.
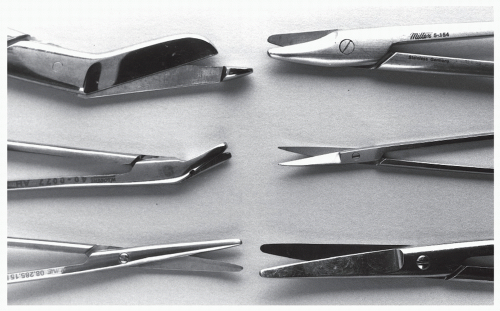 Figure 1.7 Scissors (left, top to bottom, then right, top to bottom): bandage, wire-cutting, Metzenbaum, crown-and-collar or Sistrunk, iris, and Mayo. |
HEMOSTATIC FORCEPS
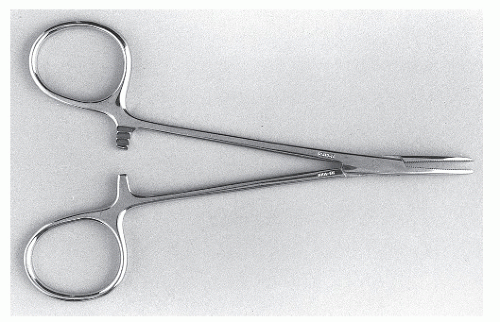
Hemostats are hinged instruments composed of a set of jaws, finger rings, and a locking mechanism (Fig. 1.9). They are the primary means of acquiring hemostasis during anatomic dissection and are also useful for bluntly spreading tissues. Many types of hemostatic forceps are available, and those most commonly used in foot surgery include the mosquito (Halsted), Crile, and Kelly designs. Hemostatic jaws are straight or curved, with serrations that run either perpendicular or parallel to the long axis of the jaws. The forceps close with force about the vessel and lock and thereby crush the contained tissue that will be ligated. If the clamped portion of vessel is to remain functional, such as in vascular reconstruction, a noncrushing or controlled-closure hemostat must be used. Hemostatic metal clips may also be used to obtain secure ligation of vessels in sites that are poorly accessible with hand ties.
THUMB FORCEPS
Thumb forceps consist of two pieces of surgical steel attached at one end, and they are used to pick up or grasp tissues (Fig. 1.10). The forceps are held among the thumb, middle finger, and index finger of either hand. The tips may be flat or have teeth or fine serrations, and they vary in width. Forceps with teeth (Brown-Adson, rat-tooth or one-two) are usually narrow and allow the surgeon to hold structures securely while a minimum of tension is applied. Flat-tipped or finely serrated narrow forceps (atraumatic forceps) are used to delicately grasp vital structures, to pull sutures and needles, and, with great care, to manipulate skin during closure. The one-two (rat-tooth) pickup is frequently used for skin closure, depending on the surgeon’s preference. The wide-tipped Russian forceps are excellent for delicate manipulation of deep tissues in the hindfoot and ankle. Wide-tipped atraumatic forceps (Potts-Smith) may also be useful for the application and removal of surgical dressings.
TRACTION FORCEPS
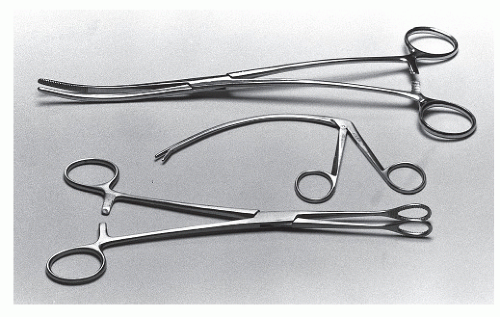
Traction forceps are of heavier construction than hemostats and consist of a locking mechanism and finger rings, as well as jaws for grasping tissues (Fig. 1.11). The grasping portion of each jaw typically has teeth, or a single sharp point, that provides traction without undue pressure or crushing force.
 Figure 1.10 Assorted thumb forceps (top to bottom): one-two or rat-tooth, Brown-Adson, and atraumatic. |
 Figure 1.11 Assorted traction forceps (top to bottom): Backhaus towel clamp, phalangeal forceps, Lewin, sesamoid clamp, Kocher, and Allis clamp. |
The Backhaus towel clamp provides a double-sharp set of jaws and is used for draping the operative field and, occasionally, for grasping bone. The Allis clamp is available with narrow or wide jaws, each jaw composed of opposing serrated edges or short teeth. These are effective for grasping and retracting fascia and the subcutaneous layer, and they are occasionally used for clamping towels while draping. Kocher forceps have two long-blade jaws displaying transverse serrations with opposing sharp, interlocking teeth at the tips. These are useful for placing traction on heavy fascia, although care must be taken to avoid crushing the contained tissues. Uterine packing forceps have gently curved, long jaws that make them ideal for transferring tendons along tendon sheaths during myoplastic reconstruction. The sesamoid clamp and phalangeal forceps are specifically designed for grasping small ossicles and bony fragments. The sponge clamp has two opposing circular jaws with transverse serrations used to hold a folded gauze sponge during preparation or blotting of the surgical area (Fig. 1.12).
RETRACTORS
Retractors are used to hold tissues aside, thereby increasing exposure and protecting vital structures. The blade portion of the retractor may be fixed or malleable, and the retractor itself may be handheld or self-retaining. Handheld retractors enable the assistant to control the force with which tissues are held and to release tension intermittently as necessary (Figs. 1.13 and 1.14). Conversely, self-retaining retractors free the assistant to perform duties that may expedite the procedure (Figs. 1.15,1.16 and 1.17). Self-retaining retractors should be gently set and intermittently released during long procedures in an effort to avoid tissue necrosis or excessive retraction trauma. Large handheld retractors such as the Army-Navy devices are helpful in providing full exposure when dissection is performed in the rearfoot and ankle area (Fig. 1.18).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree