CHAPTER 14 Instability with Bone Loss
PREOPERATIVE CONSIDERATIONS
Bone loss is frequently associated with chronic traumatic glenohumeral instability on the glenoid side or humeral side.1–4 Significant bone loss, often characterized by an inverted pear glenoid or engaging Hill-Sachs lesion, is believed to be a main cause of failure after arthroscopic stabilization.5–7
According to a three-dimensionally reconstructed computed tomography (CT) study with the humeral head digitally subtracted, the prevalence of glenoid bone defect has been reported as high as 90% in shoulders with chronic recurrent traumatic anterior instability.8 In addition, a bony fragment is present at the anteroinferior portion of the glenoid neck in about half of shoulders with glenoid bone loss.8 Furthermore, bone loss in shoulders associated with a bony fragment is relatively significant compared with that in shoulders with attritional glenoid loss without a bony fragment.8,9
ANATOMY AND PATHOANATOMY
Lo and colleagues7 and Burkhart and associates10 have defined the inverted pear glenoid as more than 25% to 30% loss of diameter in the inferior glenoid circle. Burkhart and DeBeer5 have recommended a bone grafting procedure for these shoulders based on their clinical outcome after arthroscopic soft tissue repair.
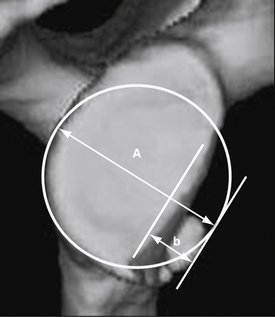
We have investigated a consecutive series of 121 glenoids in shoulders with chronic recurrent traumatic anterior instability, including 97 males and 24 females with an average age of 24 years (range, 13 to 54 years), using three-dimensional CT.11 The percentage defect of the glenoid was defined as a ratio of defect width against the diameter of the assumed circle based on the inferior portion of each glenoid (Fig. 14-1).9 The results demonstrated that 19 out of 121 glenoids (15.7%) were measured and showed more than 25% bone loss, with a mean percentage defect of 30.2% (range, 25.0% to 43.8%). Interestingly, a bone fragment was confirmed in 18 out of 19 glenoids in these shoulders (94.7%). Furthermore, in 9 glenoids (7.4%) that were measured and demonstrated more than 30% bone loss with 35.6% mean percentage defect (range, 30.6% to 43.8%), a bone fragment was confirmed in all shoulders. Therefore, it was concluded that most shoulders with a large glenoid bone defect, which corresponds to the so-called inverted pear glenoid,7 retain an associated bone fragment (Table 14-1).11
TABLE 14-1 Presence of Bone Fragment in Large Glenoid Bone Defect
| Bone Defect of the Glenoid | ||
|---|---|---|
| Parameter | 25% and more | 30% and more |
| No. of glenoids* | 19 (15.7%) | 9 (7.4%) |
| Mean percentage defect (range) | 30.2% (25.0%-43.8%) | 35.6% (30.6%-43.8%) |
| No. of attritional glenoids* | 1 (5.3%) | 0 (0%) |
| No. of glenoids with a bony fragment* | 18 (94.7%) | 9 (100%) |
* The values are given as the number of glenoids, with percentage in parenthesis.
HISTORY AND PHYSICAL EXAMINATION
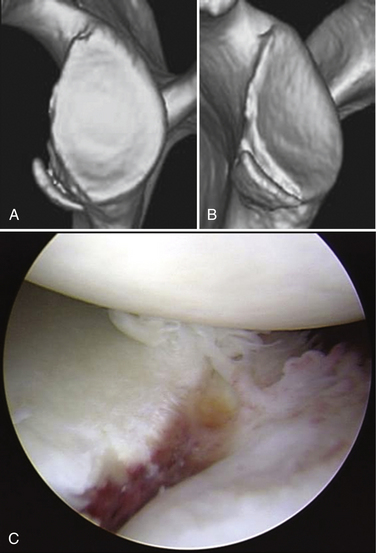
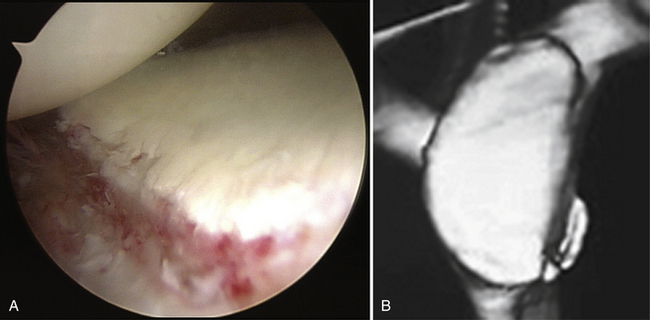
The diagnosis of recurrent traumatic anterior glenohumeral instability is usually made easily on the basis of the history of distinct dislocation or subluxation and the positive apprehension sign. However, when collision athletes are seen, care should be taken because they may not experience clear dislocation or subluxation and only complain of pain or weakness when they bring their arm to maximum external rotation in abduction. In addition, many collision athletes do have a minimally displaced bony Bankart lesion, often without a concomitant Hill-Sachs lesion, in which the arthroscopic finding demonstrates clear evidence of anteroinferior instability, but without dislocation or subluxation (Fig. 14-2).
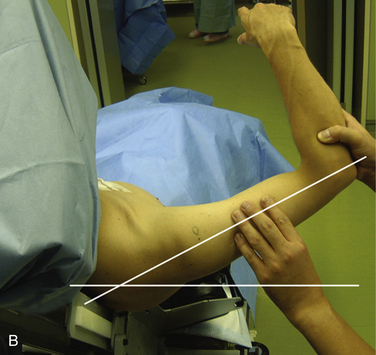
The anterior apprehension test is done with the patient in the supine position. In this test, the shoulder is moved passively into maximum external rotation with the arm at the side in 30, 60, 90, 120, and 150 degrees of abduction and maximum flexion. At the same time, the posterior apprehension test is done, with the arm at maximum internal rotation in 90 degrees of abduction. The feeling of apprehension is reported in each arm position. However, the most important and reliable physical examination can usually be done with the patient under anesthesia, comparing stability testing with the contralateral extremity (Fig. 14-3).
DIAGNOSTIC IMAGING
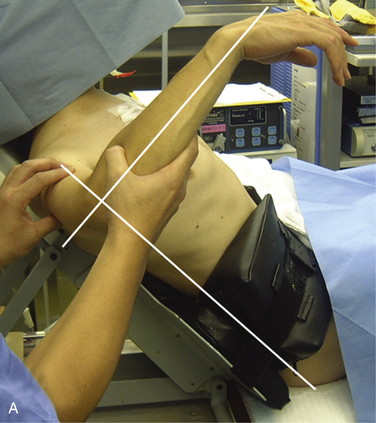
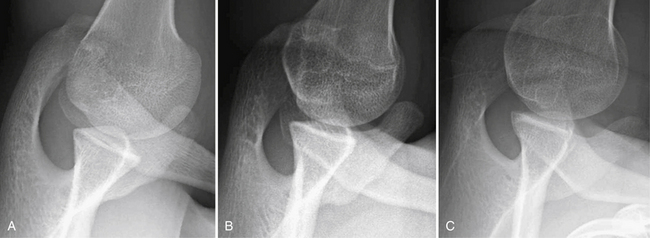
X-ray images are sometimes helpful for detecting the Hill-Sachs lesion and the anterior glenoid rim lesion,3 especially during the first patient visit. Bernageau12 has described a unique method for detecting an anterior glenoid rim lesion with the patient in the standing position. However, this technique requires fluoroscopic control to obtain optimal diagnosable images and, therefore, radiation exposure is an issue that cannot be ignored.13 Our group has developed a modified Bernageau method with the patient lying on the axilla in the most relaxed position (Fig. 14-4). In this method, clear x-ray images can be obtained more easily with a high probability of ascertaining bony pathology without using fluoroscopic imaging (Fig. 14-5).
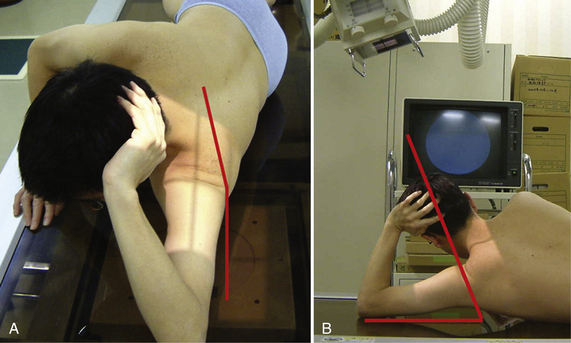
FIGURE 14-4 Modified Bernageau method. The patient lies on his or her axilla in the most relaxed position. A, In this position, the scapula needs to incline 5 degrees to the vertical line. B, Then the incident x-ray needs to be aimed craniocaudally with15 to 20 degrees of inclination to the vertical line.
Although plain magnetic resonance imaging (MRI) provides only limited information, MR arthrography is helpful when detecting a soft tissue lesion such as a Bankart lesion, capsular pathology, and/or a HAGL (humeral avulsion of the glenohumeral ligament) lesion.14 However the final diagnosis of soft tissue pathology can be made most accurately through diagnostic arthroscopy.
Three-dimensional CT is the most important imaging study for assessing glenoid morphology accurately.8 The arthroscopic glenoid view sometimes makes surgeons overestimate the bone defect because normally the cartilage damage is more extensive than the bony lesion (Fig. 14-6). Furthermore, in a shoulder with a bony Bankart lesion, detecting accurate configuration of the bony fragment is not easy because the bone fragment is covered by the surrounding soft tissue. Through preoperative three-dimensional CT, surgeons can determine whether the glenoid is attritional or if a bony Bankart lesion is present. They can also quantify bone loss with attritional glenoids and detect the size and shape of the bony fragment in shoulders with a bony Bankart lesion.8,9,11,15
Arthroscopic Treatment
If a bone fragment is present with three-dimensional CT, an arthroscopic bony Bankart repair, in which the fragment is incorporated into the Bankart repair, is indicated, regardless of the severity of bone loss.9,16,17 Therefore, most shoulders with a large glenoid bone loss can be treated arthroscopically using this technique.11 For shoulders with significant bone loss associated with the attritional glenoids in young and active patients, although the number of such patients is limited, open or arthroscopic bone grafting procedures are indicated. My preference is an arthroscopic iliac bone grafting in combination with an anterior-inferior capsulolabral repair (see later).18–20
Arthroscopic Bony Bankart Repair
Most bony Bankart lesions are displaced and represent a partly malunited chronic avulsion–type fracture, and the bony fragment is firmly connected to the adjacent labrum or soft tissue. These characteristics of chronic bony Bankart lesions make arthroscopic bony reconstruction feasible.9,16
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree