CHAPTER 76 Injuries of the Upper Cervical Spine
Demographics
Traumatic injuries to the upper cervical spine are most often encountered in children and in people older than age 60 years. Fortunately, they are still rare occurrences in children. Motor vehicle accidents are the cause of pediatric cervical spine trauma in about 38% of cases.1–3 Cervical spine injuries in children account for 1% to 9% of all reported pediatric spinal trauma.4,5 Upper cervical spine injuries are responsible for the majority of these, accounting for 56% to 73% of all cervical spine injuries in children.2,6 Head injury occurs in conjunction with cervical spine injuries in up to 53% of these cases. When these two entities are concurrent, the overall mortality is very high (41%).7
Upper cervical spine injuries constitute a large proportion of cervical spine trauma in people older than age 60 years. Injuries to the C1-C2 complex account for up to 69.8% of all cervical spine trauma in those older than the age of 60.8 Odontoid fractures alone can constitute up to 57% of all cervical spine injuries in this age group. Unlike the pediatric and young adult populations, upper cervical spine trauma in the elderly often occurs from minor trauma. Falls are often the predominant cause of injury. Many explanations for this phenomenon include the presence of weakened bone at the CCJ owing to osteoporosis/osteopenia, higher stresses on the upper cervical spine owing to spondylosis of the lower cervical spine, and an increased propensity to fall from deterioration in locomotor response and balance control due to age and cervical spinal stenosis. The lower energy of the trauma is directly correlated to the lower rate of neurologic injury seen in this age group after injury as compared with the pediatric and young adult populations. However, when neurologic deficits occur, they can have devastating consequences. A 26% to 28% mortality for upper cervical level spinal cord injury has been reported for this population, with a dismal 59% survival at 2 years.9–11
In the young adult population, the majority of patients with spinal column injury are young males (up to 30% are males in their 30s).12 The most common mechanism in this age group is from vehicular accidents, followed by falls, gunshot injuries, and sports injuries. Most of the cervical spine trauma in this age group occurs in the subaxial spine and is often associated with a high-energy mechanism, severe head injury, or a focal neurologic deficit.13 Trauma to the CCJ in this population is often associated with severe neurologic injury and head trauma with relatively high rates of mortality and morbidity.
Anatomy of the Upper Cervical Spine (Craniocervical Junction)
The upper cervical spine is a complex three-unit joint that includes the bones of the occiput, atlas, and axis, their synovial articulations, and the associated ligamentous structures. The six synovial joints in this complex include the paired occipitoatlantal joints, the anterior and posterior median atlantoodontoid joints, and the paired atlantoaxial joints. These joints allow for a significant amount of motion at the CCJ. The occiput-C1 articulation supplies approximately 50% of total cervical flexion and extension, and the C1-C2 articulations supply 50% of total cervical rotation.14 Corresponding to this, the majority of the mechanical stability at the CCJ is provided by the investing ligamentous structures. An understanding of the anatomy of the CCJ is necessary to appreciate the spectrum of injuries that occur in the upper cervical spine and the strategies that have been devised to treat them. The specific articulations, ligamentous restraints, and neurovascular structures at risk for injury are addressed in a systematic fashion.
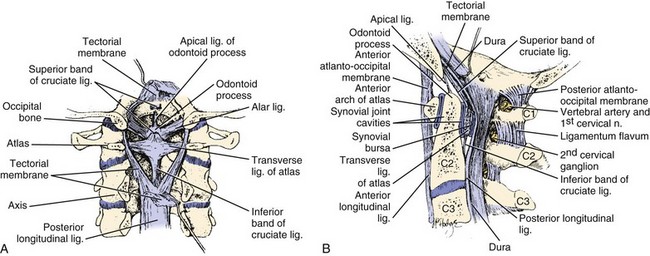
The occiput articulates with the atlas through paired occipitoatlantal joints. The occipital condyle is oval and sloped inferiorly from lateral to medial in the coronal plane, making a 25- to 28-degree angle with the midsagittal plane. The convex occipital condyles articulate with the concave superior articular facets of C1 in a “cup-and-saucer”–type fashion. In the coronal plane, the joint slopes medially toward the foramen magnum. The shape of the occipitoatlantal joint allows significant flexion and extension and some lateral bending but minimal axial rotation. Flexion is limited by the bony impingement of the anterior portion of the foramen magnum on the odontoid process, and extension is limited by the posterior arch of the atlas impinging on the posterior aspect of the skull. The anterior atlanto-odontoid joint lies between the anterior arch of the atlas and the anterior aspect of the dens. The posterior atlanto-odontoid articulation lies between the posterior aspect of the dens and the anterior portion of the transverse ligament. The paired atlantoaxial joints are situated between the inferior articular facets of the atlas and the superior articular facets of the axis. These joints are fairly shallow to allow for a significant amount of motion at the CCJ. The ligamentous restraints provide the necessary stability to prevent injury to the enclosed brainstem and spinal cord (Fig. 76–1).
The anterior longitudinal ligament attaches to the anterior body of the axis, anterior arch of the atlas, and anteroinferior edge of the foramen magnum. The cruciform ligament is composed of vertical and transverse portions. The vertical portion attaches to the anterior edge of the foramen magnum and the posterior aspect of the body of the axis. The transverse component of the cruciform ligament is commonly referred to as the transverse ligament. This important structure is made entirely of relatively nonelastic collagen fibers and extends between the osseous tubercles on the medial aspects of the lateral masses of the atlas. The tectorial membrane is the broad cephalic extension of the posterior longitudinal ligament and runs from the posterior surface of the body and dens of the axis to the anterolateral edge of the foramen magnum. This structure is a primary stabilizer of the occipitoatlantal articulation15 and helps to limit extension at this joint. The nuchal ligament extends from the posterior border of the occiput to the spinous processes of the cervical vertebrae to C7 and the intervening interspinous ligaments. The anterior occipitoatlantal membrane, part of the anterior longitudinal ligament, extends from the cephalad portion of the anterior arch of the atlas to the anterior edge of the foramen magnum. The atlanto-odontoid ligament runs from the anterior surface of the odontoid process and the caudal portion of the anterior arch of the atlas. The apical ligament of the dens lies between the vertical band of the cruciform ligament and the anterior occipitoatlantal ligament. This structure connects the apex of the dens with the anterior edge of the foramen magnum. The alar ligaments are paired structures that arise from the dorsolateral aspect of the dens and run obliquely to connect with the inferomedial aspect of the occipital condyles and the lateral masses of the atlas. These ligaments are important stabilizers of the occipitoatlantal joint and limit axial rotation and lateral bending.15 Like the transverse ligament, the alar ligaments are also made entirely of collagen fibers, and failure occurs at 10% stretch.16 These ligaments are most vulnerable in whiplash-type injuries.17 The posterior occipitoatlantal membrane attaches to the posterior margin of the foramen magnum and the posterior arch of the atlas. The posterior atlantoaxial membrane runs between the posterior arches of the atlas and the axis.
The vertebral artery and the internal carotid artery lie in close proximity to the osseous structures of the CCJ. Within the atlas and the axis the paired vertebral arteries typically lie in the foramen transversarium. At this level the paired vertebral arteries are susceptible to injury by shearing forces with rotation and flexion or extension. At the upper atlantal surface, the artery curves posteriorly into a transverse groove in the atlas behind the superior atlantal articular facet. In patients with congenital bony anomalies of the upper cervical spine, there is a higher incidence of vertebral artery anomalies.18 The artery then enters the subarachnoid space by piercing the posterior occipitoatlantal membrane and dura mater just medial to the occipital condyle. The internal carotid artery is adjacent to the anterior surface of the lateral mass of C1. This position renders it susceptible to injury by a forward thrust of the lateral mass as the head is forcefully rotated to the contralateral side.19
Clinical Evaluation
The treatment of a patient with a cervical spine injury regardless of location is initiated at the scene of the injury. Without exception, all victims of trauma are suspected to have a cervical injury until proven otherwise. Cervical spine injury has been closely linked to the presence of severe head injury (odds ratio 8.5), a high-energy mechanism (odds ratio 11.6), or a focal neurologic deficit (odds ratio 58).13 In suspected injuries of the upper cervical spine, an adequate airway and ventilation must be established because upper spinal cord injury can lead to diaphragmatic and intercostal paralysis with respiratory failure. In addition, large retropharyngeal hematomas can cause upper airway obstruction. Nasotracheal intubation or cricothyroidotomy is safest in the acute setting because it causes less cervical spine motion than direct oral intubation techniques.20,21 However, improvements in fiberoptic imaging have resulted in newer technologies such as the Glidescope. This videolaryngoscope allows oral-tracheal intubation without the need for significant neck manipulation and is technically easier than the traditional method of fiberoptic-assisted intubation. Once the patient’s airway, breathing, and circulation are stabilized, initial stabilization of the cervical spine begins with the application of a rigid cervical collar, a spine board, and sandbags.
In general, noncontiguous spinal injuries can occur in 6% of patients and these fractures can be easily missed in the presence of head injury, upper cervical injury, or cervicothoracic injury. Atlas fractures, specifically, are associated with up to a 50% incidence of concurrent cervical spine fractures.22 Facial and head injuries are also commonly seen in conjunction with fractures and ligamentous disruptions of the CCJ. Specifically, upper cervical injuries are also more frequently seen in patients with trauma to the lower third of the face.23 In addition, up to 50% of patients with cervical spine injuries, spinal cord injuries, or both have associated head trauma. Brain damage is more associated with upper cervical injuries than with injuries to the subaxial spine.24 Subarachnoid hemorrhages, subdural hemorrhages, and cerebral contusions must be diagnosed and treated expeditiously because they are the most common cause of mortality in these patients.
In addition to the spinal trauma, other injuries should be assessed because they may influence the treatment of the spinal lesion and also significantly affect the outcome of the patient. In cervical spine trauma, much attention has been paid to the evaluation of these patients for vertebral artery injury. Friedman and colleagues25 reported a 24% overall incidence of vertebral artery injury in 37 cases of nonpenetrating cervical spine trauma. Vaccaro and colleagues26 noted a 19.7% incidence of vertebral artery injury found by magnetic resonance angiography in 61 patients. In Cothren and colleagues’27 series, 18% of 69 patients with vertebral artery injury and cervical spine trauma sustained injuries to the CCJ. The incidence of vertebral artery injury increases if the fracture extends into the foramen transversarium.28 Bilateral or dominant vertebral artery injury can cause fatal ischemic damage to the brainstem and cerebellum.29 Delayed cortical blindness and recurrent quadriparesis can also occur from occult vertebral artery injury after cervical trauma.30 Despite the high incidence of vertebral artery injury with cervical trauma, as well as the potential morbidity and mortality associated with vertebral artery injury, the great majority of these injuries are clinically silent.
Neurologic evaluation of injuries to the CCJ can be difficult because there is no specific myotomal or dermatomal distribution of motor and sensory loss, and it is further confounded by the frequent coexistence of facial and head trauma. Injuries to the C1 and C2 roots generally result in sensory deficits to the occiput and posterior scalp. A complete spinal cord injury at this level can result in ventilator-dependent quadriplegia. Incomplete spinal cord injury syndromes can also occur. At the occipitocervical junction, a peculiar syndrome of incomplete paralysis can develop as a result of compression/injury of the pyramidal decussation on the anterior aspect of the brainstem where the corticospinal tracts cross from one side to the other. The tracts to the arms cross cephalad to the tracts to the legs. If the primary injury is to the upper decussation, the arms can be more affected and give the appearance of a central cord syndrome. Caudal injury will affect the legs more than the arms. It is even possible to affect crossed arm fibers and uncrossed leg fibers, the so-called cruciate paralysis as described by Bell.31 These patients can also have large variations in heart rate, blood pressure, and respiratory rate owing to injuries to the cardiovascular and respiratory centers in the brainstem.32 Dysfunction of the lower cranial nerves (CN IX, X, XI, XII) is often seen with severe injuries to the occipitoatlantal joint and the skull base.
Imaging
Plain radiography is used as the first imaging modality for the upper cervical spine. The standard series includes anteroposterior, lateral, and open-mouth views. In general, about 85% of all significant injuries to the cervical spine will be detected on the lateral view of the cervical spine. In the upper cervical spine, the lateral view and the open-mouth view are the most useful. Flexion and extension views will be inadequate to assess for ligamentous injury owing to voluntary guarding in 33% of cases.33
Computed tomography (CT) remains the most sensitive imaging modality to evaluate fractures of the upper cervical spine, subaxial spine, and cervicothoracic junction. In a prospective study of polytrauma patients, CT used as a primary screening tool had a sensitivity of 84% in detecting upper cervical injury.13 CT is also cost effective as a primary screening tool, especially in high- and moderate-risk patients.34 With the added benefit of sagittal and coronal reconstructed images, CT has immense power to demonstrate complex fracture patterns not easily seen on standard radiography and on the axial images, especially at the occipitocervical junction.35
Magnetic resonance imaging (MRI) is not as good as CT or plain radiographs in the identification and evaluation of cervical fractures. Klein and colleagues36 showed that MRI had only 11.5% sensitivity for posterior fractures and 36.7% sensitivity for anterior fractures. Katzberg and colleagues12 reported that for acute fractures MRI had a weighted average sensitivity of 43%, compared with 48% for conventional radiography. Vaccaro and colleagues37 also noted that MRI is not cost effective as a screening device in patients without a neurologic deficit.
Despite its inadequacies in evaluating bony detail, MRI is unsurpassed for the assessment of the soft tissue elements in the cervical spine. These structures include the intervertebral disc, ligamentous structures, and the spinal cord itself.12 MRI is much more sensitive and specific than plain radiographs for the evaluation of a prevertebral hematoma. MRI is also useful for the detection of spinal cord hemorrhage, which, if present, carries a poor prognosis for neurologic recovery.38 Acute hemorrhage has a low signal intensity on T2-weighted images (secondary to intracellular deoxyhemoglobin) and becomes hyperintense over the next several days after it becomes converted to extracellular methemoglobin. MRI diffusion studies allow a more accurate assessment of the degree of spinal stenosis. These diffusion studies assess the flow of cerebral spinal fluid (CSF) around the spinal cord at an area of constriction. If the degree of spinal stenosis is severe, the CSF flow is significantly compromised.39
MRI neurography provides detailed visualization of individual nerve roots as they exit the brainstem, CCJ, and subaxial cervical spine. This MRI modality can help distinguish root level injuries from more peripheral injuries and double-crush–type nerve damage.40
Bedside fluoroscopic flexion and extension views have shown some diagnostic value in clearing the cervical spine in obtunded patients. In one report it was noted that 30% of these patients could not be adequately evaluated by this technique.41 Other researchers, however, have found this helpful, using a combination of initial in-line traction followed by flexion and extension views only if the traction views are normal.42 Due to the space constraints of most intensive care units and the lack of appropriate built-in shielding for the extensive use of fluoroscopic imaging, bedside fluoroscopy is relatively impractical in most hospitals. In addition, the use of both CT and MRI may provide sufficient information to allow removal of the cervical collar in an obtunded patient without the need for manipulation of the neck.
Specific Injuries to the Upper Cervical Spine
Occipital Condyle Fractures
Most injuries to the occipital condyles are caused by high-energy trauma to the head and neck. Bell reported the first case of occipital condylar fracture in 1817. The incidence of occipital condyle fractures is reported to range from 3% to 16%.43,44
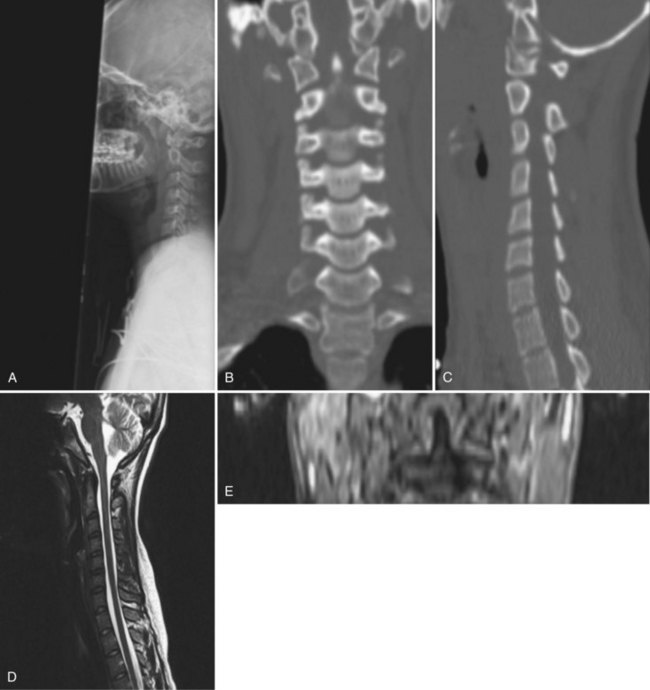
Although radiographs may show some abnormal soft tissue swelling in the presence of an occipital condyle fracture, these injuries are often extremely difficult to detect with conventional radiography (Fig. 76–2).45
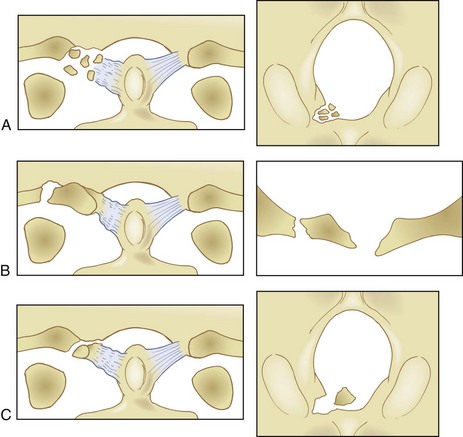
The most used classification system for occipital condyle injuries was described by Anderson and Montesano (Fig. 76–3).46 The injuries are categorized into three types according to morphology and mechanism of injury. Type I injuries are impaction fractures of the condyle from axial loading. These fractures tend to be comminuted. The tectorial membrane and the alar ligaments are usually intact. Unilateral type I lesions are stable, but bilateral lesions may be unstable. Type II injuries are part of a more extensive basioccipital fracture that involves one or both occipital condyles. The common mechanism of injury is a direct blow to the skull. The tectorial and alar ligaments are intact, and the fracture is usually stable. Type III injuries are avulsion fractures near the alar ligament insertion that result in medial displacement of the condylar fracture fragment from the inferomedial aspect of the occipital condyle into the foramen magnum. The mechanism of injury is a forced rotation of the head combined with lateral bending. Type III fractures are potentially unstable injuries owing to avulsion of the alar ligaments.
In contrast to the majority of publications, Maserati and colleagues47 reviewed 106 patients with occipital condyle fractures seen at a level one trauma center and found that only 3 required occipitocervical fusion. They suggested that each patient be evaluated looking for occipitocervical misalignment and that only those patients should be treated in a halo-vest or with a posterior fusion. The other 103 patients were successfully treated in a rigid cervical collar.47
Atlanto-Occipital Injuries
The incidence of injuries to the atlanto-occipital joint is estimated to be between 5% and 8% of fatal traffic injuries.48 These injuries account for 19% to 35% of all deaths from cervical spine trauma. More than 80% of cases of occiput-C1 dislocations were reported after 1975. Improvements in on-site resuscitation and emergency transportation have increased the number of patients who survive this catastrophic injury, which is typically the result of a motor vehicle accident. In a review of 146 traffic fatalities, Alker and colleagues49 found a 5% incidence of occipitoatlantal dislocations. Children younger than 12 years of age are uniquely predisposed to this injury because their occipitoatlantal joints are flatter and because their head weight–to–body weight ratio is significantly greater than in adults.
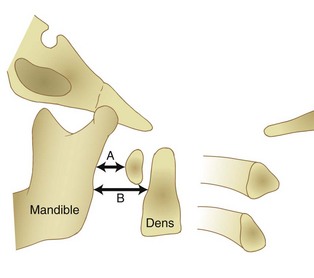
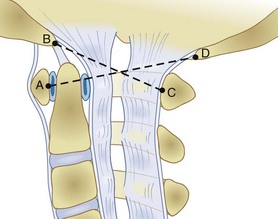
Radiographically, significant retropharyngeal soft tissue swelling at C3 will be seen (Fig. 76–4). Multiple anatomic lines mark the normal relationship of occiput to C1. A line drawn down the cranial aspect of the clivus should be tangential to the dens (Wackenheim line). Distance greater than 10 mm between the basion and the dens is considered abnormal.50 The sensitivity of this method is about 50%. An interval greater than 13 mm between the posterior mandible and the anterior atlas or 20 mm between the posterior mandible and the dens is abnormal (Fig. 76–5).51 The sensitivity of this method is 25%. Failure of a line drawn from the basion to the axis spinolaminar junction to intersect C2 or failure of a line from the opisthion to the posterior inferior corner of the body of the axis to intersect C1 is abnormal.52 The sensitivity of this method ranges from 20% to 75%. Powers’ ratio, the ratio of the distance from the basion to the posterior arch of the atlas divided by the distance from the opisthion to the anterior arch of the atlas, should be 1.0 or less in the absence of anterior occipitoatlantal dislocation (Fig. 76–6).53 Another method to diagnose occipitoatlantal subluxation or dislocation on plain radiographs was described by Harris and colleagues.54,55 They described a posterior axial line as the cranial extent of the posterior cortex of the axis body. If the distance between the basion and the posterior axial line (the basion-axial interval) is greater than 12 mm, or if the basion-dental interval is greater than 12 mm, then occipitocervical instability is present.54,55 The sensitivity of this method varies from 76% to 100%.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree