I. Talus Fractures and Dislocations
A. Anatomy
1. Parts—The talus comprises three distinct parts: the head, which articulates with the navicular; the neck, which is nonarticular; and the body, which has articulations with the tibia above and the calcaneus below. Approximately 50% of the talus is covered by articular cartilage. The talus has no muscular or tendinous attachments. The talar dome is wider anteriorly. The posterior process of the talus contains the medial and the lateral tubercles, between which the flexor hallucis longus courses. The lateral tubercle is larger and may exist as a separate ossicle (the os trigonum), attached only by ligamentous structures.
2. Blood supply—The talus receives its blood supply from two main sources: extraosseous and intraosseous (Fig. 14-1).
• Extraosseous supply
(a) Posterior tibial artery
• Artery of the tarsal canal—The artery of the tarsal canal gives off a deltoid branch, which passes through the deltoid ligament and supplies the medial body of the talus.
• Calcaneal branches
(b) Anterior tibial artery (dorsalis pedis artery)
• Medial tarsal branches
• Anterolateral malleolar artery—The anterolateral malleolar artery contributes to the artery of the tarsal sinus.
(c) Peroneal artery—The peroneal artery contributes to the artery of the tarsal sinus.
• Intraosseous supply
(a) Talar head
• Superomedial half—The superomedial half is supplied by branches from the anterior tibial artery (dorsalis pedis artery).
• Inferolateral half—The inferolateral half is supplied by the arteries of the tarsal sling (artery of the tarsal canal and artery of the tarsal sinus).
(b) Talar body—The main blood supply is the anastomosis between the artery of the tarsal canal and the artery of the tarsal sinus.
B. Injury Types
1. Talar head fractures—Talar head fractures account for 5% to 10% of all talus fractures.
• Mechanism of injury
(a) Axial loading with the ankle in plantar flexion or compression of the head of the talus against the distal tibia with the ankle in dorsiflexion
(b) Shear fracture of the navicular as it medially dislocates over the talar head during an inversion injury
• Associated injuries—Metatarsal fractures are common associated injuries; midfoot instability is common.
• Treatment
(a) Nondisplaced fractures—Most fractures are nondisplaced because of the strong capsular and ligamentous attachments. Treatment involves a short leg cast and nonweightbearing for 4 to 8 weeks
(b) Displaced fractures—No good evidence exists to guide treatment in regards to fragment excision versus open reduction and internal fixation. If the fragment is large enough, standard practice is to internally fix it and excise small fragments.
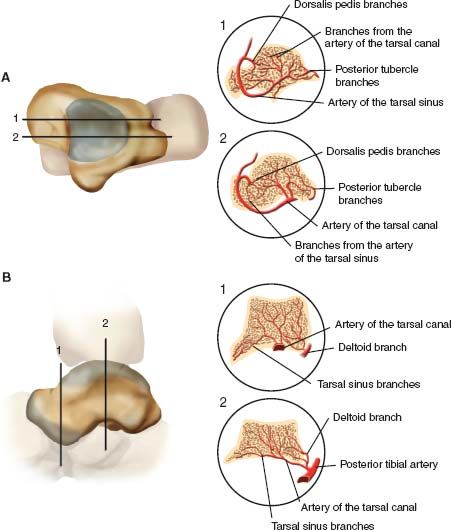
FIGURE 14-1 A. Sagittal sections through the talus in planes 1 and 2. Note that the body of the talus is supplied mainly by branches from the artery of the tarsal canal and the posterior tubercle branches (2), whereas the head of the talus is supplied by branches from the dorsalis pedis and the tarsal sinus arteries (1). B. In the coronal plane, the lateral two-thirds of the talar body is supplied by branches from the artery of the tarsal canal and the medial one-third by the branches entering through the deltoid ligament insertion.
• Complications—Complications include arthritis due to malalignment, osteonecrosis (approximately 10% of cases), and osteochondral fractures.
2. Talar neck fractures—Talar neck fractures are also called aviator’s astragalus.
• Overview—Talar neck fractures are high-energy injuries usually occurring as a result of hyperdorsiflexion in which the talus impinges on the distal tibia. Approximately 15% to 20% of these injuries are open fractures. They are frequently associated with malleolar fractures (25% of cases); injury to the medial malleolus is more common. There is a high risk of soft-tissue injuries and compartment syndrome.
• Classification—According to the Hawkins classification (Fig. 14-2), talar neck fractures are classified into four types.
(a) Type 1 is nondisplaced.
(b) Type 2 involves a displaced talar neck fracture and subluxation or dislocation of the subtalar joint.
(c) Type 3 involves a displaced talar neck fracture and dislocation of both the ankle and subtalar joints.
(d) Type 4 involves a displaced talar neck fracture and dislocation of the ankle and subtalar joints with a talonavicular dislocation.
• Radiography—A foot and ankle series is obtained. The talar neck profile is best seen on the Canale view (maximum plantar flexion with 15° of pronation with the beam directed 75° cephalad from the horizontal).
• Treatment—Treatment is determined by the Hawkins type. The goal of treatment is anatomic reduction; historically, early reduction of displaced fractures was thought to reduce the risk of osteonecrosis. Recently, a study has shown that approximately 60% of orthopedic traumatologists find it acceptable to operate after 8 hours, and 46% find it acceptable to operate after 24 hours.
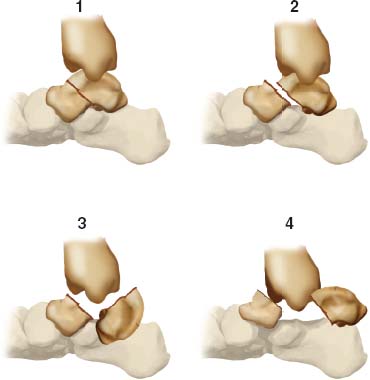
FIGURE 14-2 Hawkins (and Canale) classification of talar neck fractures. (1) Nondisplaced; (2) with subtalar subluxation or dislocation; (3) with talar body dislocation; and (4) with talar body and head dislocation.
(a) Hawkins Type 1—Type 1 injuries are treated with 4 to 6 weeks of non weightbearing in a short leg cast, followed by 1 to 2 months in a walking cast. If joint stiffness or late fracture displacement is a concern, percutaneous fixation may be contemplated.
(b) Hawkins Type 2—Type 2 injuries constitute an orthopaedic emergency. Immediate manipulation of the fragments with traction and plantar flexion to realign the talar head fragment with the talar body is recommended. If the reduction is anatomic (reported to occur in approximately 50% of cases), the injury may be treated in the same manner as a Hawkins Type I injury. Residual deformity must be corrected to accept no more than 5 mm of displacement, with angulation of 5° or less. One study by Sangeorzan (1992) showed that as little as 2 mm of displacement of the talar neck significantly affects articular pressures. Most agree that Type II fractures should undergo internal fixation to avoid late displacement. Open reduction may be carried out through an anterolateral (least vascular risk) or anteromedial arthrotomy, or through a posterolateral approach. Fixation is usually via screws placed across the talar neck. The surgical approach is determined by the location of the fracture fragments, open wounds, contused skin, and adjacent fractures. The anteromedial approach is the most frequently used, but carries the greatest risk of injury to the artery to the tarsal canal. Sometimes, both the anteromedial and anterolateral approaches are necessary to allow for cross screw fixation. The posteromedial approach should be avoided because of the high incidence of painful sequelae. Intraoperative radiographs are necessary to ensure proper bony reduction and avoid malalignment (especially a varus deformity of the talar neck). Posterior-to-anterior–directed screws demonstrate the largest strength of fixation compared with K-wires or anterior-to-posterior directed screws.
(c) Hawkins Type 3—Treatment of Type 3 injuries is similar to that of Type 2 injuries. However, soft-tissue problems are more frequent, and results are generally poorer. Manipulation less frequently results in an acceptable reduction, and therefore ORIF is more commonly required. Sometimes skeletal traction through the calcaneus is necessary to gain reduction of the talar body fragment. If the talar body is extruded, primary Blair fusion may be performed, as replacement of the talus leads to a notoriously high rate of infection. The deltoid branch of the posterior tibial artery may be the only remaining blood supply to the talus. Attention must be directed toward minimizing soft-tissue stripping of the deltoid ligament. The talus may spin on the deltoid ligament and must be derotated to maintain the blood supply.
(d) Hawkins Type 4—Type 4 is a rare injury. Treatment principles follow those outlined for a Type 2 injury.
• Complications—Patients report a high rate of dissatisfaction as a result of the numerous sequelae.
(a) Skin necrosis and infection—The dorsal skin envelope is particularly at risk for necrosis and infection. A delay in fracture reduction if it is tenting the skin increases the risk of ischemia. Osteomyelitis is common in open injuries and requires excision of infected bone and subsequent arthrodesis.
(b) Delayed union or nonunion
• Delayed union—Delayed union occurs in approximately 10% of cases and is defined as failure to heal after 6 months. It occurs secondary to the tenuous blood supply of the talus with slow revascularization. Weightbearing should be limited until bridging callus is seen.
• Nonunion—Frank nonunion is rare. The incidence of both nonunion and delayed union is reduced with immediate internal fixation. Fractures that have failed to unite 1 year after the injury should be treated with ORIF and bone grafting.
(c) Malunion—Varus malunion is the most common malunion and commonly results from closed manipulation without internal fixation. This deformity ultimately leads to degenerative arthritis of the subtalar joint and occurs most commonly with a Type 2 injury (up to 50% of cases). Clinically, patients present with decreased subtalar motion and stand on the lateral border of the foot. Identifying malalignment using proper X-ray studies after manipulation or ORIF helps reduce the risk of varus malunion. Using only a medial approach may increase the risk of a varus malunion due to limitations of fracture reduction visualization.
(d) Posttraumatic arthritis—Posttraumatic arthritis occurs at the subtalar joint (50% of cases), tibiotalar joint (33% of cases), or both joints (25% of cases). It results from articular damage at the time of injury, osteonecrosis with late segmental collapse, malunion, or prolonged immobilization leading to fibrosis. Local injections may be necessary to identify specific joint involvement. Conservative treatment is frequently effective, but if it is unsuccessful, arthrodesis may be the only alternative.
(e) Osteonecrosis—The incidence is related to injury type (Table 14-1). “Hawkins sign” (Fig. 14-3), if present, is seen on plain X-ray films at 6 to 8 weeks, and signifies revascularization and atrophic changes in the body of the talus. Hawkins sign appears as a subchondral luceny in the dome of the talus on the anteroposterior view. Its presence signifies that osteonecrosis will not occur; its absence does not indicate that osteonecrosis will definitely occur. MRI or nuclear medicine studies are sometimes helpful in determining this in equivocal cases. In cases of osteonecrosis, an increase in the radiographic density of the talar body is not seen for 3 months or more. If osteonecrosis is present, weightbearing is controversial. Bony union of the fracture does not appear to be delayed by osteonecrosis. Weightbearing, however, should be delayed until union of the talar neck fracture. In cases with documented osteonecrosis, some injuries heal well as long as late segmental collapse is avoided. Offloading in a patellar tendon-bearing brace should be maintained until revascularization of the talus occurs (up to 36 months by creeping substitution). A late segmental collapse is a difficult problem from a management standpoint; tibiocalcaneal fusion, Blair fusion, and modified Blair fusion (maintaining the head and neck of the talus) are treatment options.

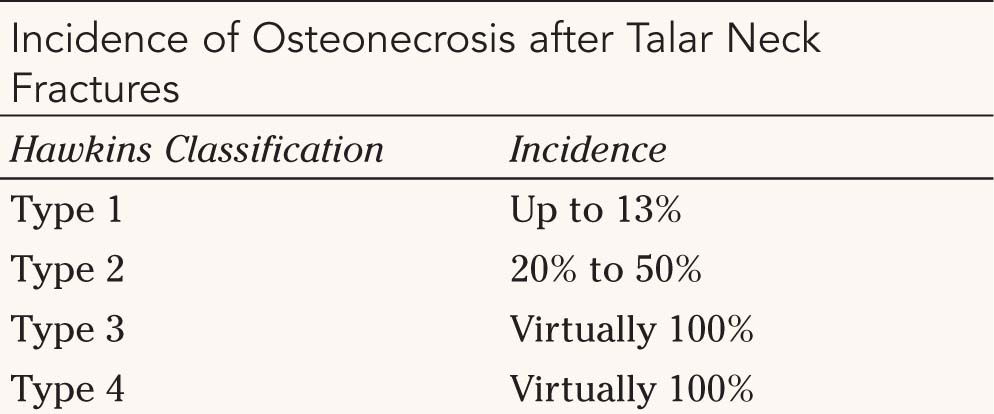


FIGURE 14-3 Hawkins sign. Note the atrophy in the subchondral area of the talus, which suggests vascularity. (This is a good prognostic sign for viability of the talus.) (Reprinted with permission from Mann RA, Coughlin MJ, Surgery of the foot and ankle, ed 6, St. Louis, 1993, Mosby).
• Posterolateral approach—Damage to the sural nerve is most likely.
• Anteromedial approach—Damage to the saphenous nerve is most likely
• Anterolateral approach—Damage to the dorsal intermediate cutaneous branch of the superficial peroneal nerve is most likely.
3. Talar body fractures—Talar body fractures include fractures involving the superior articular surface or the trochlear region. These fractures can occur in any plane and have a much poorer prognosis than talar neck fractures. The classification (Fig. 14-4) is based on the plane of the fracture and fracture fragment displacement. Treatment involves surgery in all but those with minimal displacement. The medial surgical approach with a malleolar osteotomy gives wide exposure for fixation. The lateral approach carries less risk of vascular compromise. Fracture fixation may be achieved with cancellous screws, K-wires, or Herbert screws. The overall incidence of osteonecrosis is approximately 50% and in general is not related to fracture type for talar body fractures. (The incidence of osteonecrosis is related to fracture type for talar neck fractures.) The treatment of osteonecrosis after a talar body fracture is similar to that for osteonecrosis after a talar neck fracture.
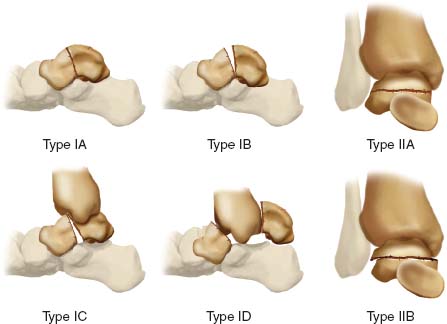
FIGURE 14-4 Fractures of the talar body.
• Lateral process fractures (Snowboarder’s fracture)—The mechanism of injury is dorsiflexion, inversion, external rotation, and axial loading. The lateral process of the talus contains the attachments for the cervical, bifurcate, anterior talofibular, and lateral talocalcaneal ligaments.
(a) Examination—The physical findings mimic those of a lateral ankle sprain. A history of an inversion injury is characteristic. A high index of suspicion is needed to make the diagnosis. Radiographs often demonstrate subtle or no obvious findings. Evaluation with computed tomography (CT) is often helpful.
(b) Radiography
• Plain films—AP view of the ankle and view with the leg internally rotated 20° are the views that best visualize the lateral process in order to look for a fracture.
• CT—Coronal slices
(c) Treatment—Treatment depends on the size of the fragment, displacement, and comminution.
• Nondisplaced fractures—Nondisplaced fractures may be treated in a short leg cast (nonweightbearing) for 4 weeks, followed by weightbearing in a short leg cast for two more weeks.
• Displaced fractures without comminution—Displaced fractures without comminution are amenable to ORIF with small fragment fixation or a Herbert screw.
• Comminuted fractures—Comminuted fractures are best addressed with excision and early subtalar motion with no weightbearing.
(d) Complications—A delay in diagnosis causes the greatest problems. Healed displaced fragments can give rise to subtalar arthritis. If excision does not provide relief, subtalar arthrodesis is the treatment of choice.
• Posterior process fractures (Shepherd’s fractures)
(a) Diagnosis—There may be a history of trauma or pain of insidious onset. The pain may be vague and nonspecific and may localize to the posterior ankle. The pain is usually aggravated by forced equinus of the ankle. Hallux motion may reproduce the painful symptoms as the flexor hallucis longus courses adjacent to the tubercles then through a groove under the sustentaculum tali.
(b) Mechanism of injury—Two mechanisms of injury have been proposed: hyperdorsiflexion and/or inversion, leading to tightening of the posterior talofibular ligament with avulsion of the lateral tubercle, and forced plantar flexion, causing compression of the lateral tubercle between the tibia and the calcaneus.
(c) Stress fractures—Stress fractures leading to failure of the lateral ossicle to unite may occur as a result of repetitive activity.
(d) Radiography—The lateral ankle view provides the best delineation of the fracture. It is difficult to distinguish between an acute fracture of the trigonal process (roughened edges) and discontinuity of the os trigonum (smooth edges). A bone scan can be helpful.
(e) Treatment—Treatment involves a non-weightbearing cast for 4 weeks, followed by a walking cast for 2 weeks. Persistent pain is treated with further casting. Symptoms lasting over 6 months indicate nonunion. A bone scan may be useful for documenting localized metabolic activity. Excision through a posterolateral approach (between the flexor hallucis longus and the peroneals) is recommended for cases of nonunion. Athroscopic excision has also been described.
5. Osteochondral defects of the talus—These are intra-articular fractures of the talar dome articular surface. Impaction injuries may leave the overlying cartilage intact while shear injuries may cause a flap tear of the cartilage. Osteochondral defects of the talus occur in 6.5% of all ankle sprains. After trauma, 55% of the lesions involve the medial portion of the talus, and 45% involve the lateral talus.
• Mechanism
Lateral—dorsiflexion and inversion of the ankle cause impaction and anterolateral shear.
Medial—Plantar flexion and inversion cause the superomedial ridge of the talus to rub on the tibial plafond, resulting in a medial lesion.
• Diagnosis—Symptoms mimic those of an ankle sprain; this injury may have the sensation of a foreign body.
• Radiography—A lateral lesion is usually flatter and more wafer-like as opposed to a medial lesion, which is deep and cup-shaped. CT can help delineate the depth and size of the lesion, but MRI is more accurate in determining the overlying cartilage separation and dissociation of the fragment from its subchondral bed. MRI can also identify associated soft-tissue injuries.
• Classifications
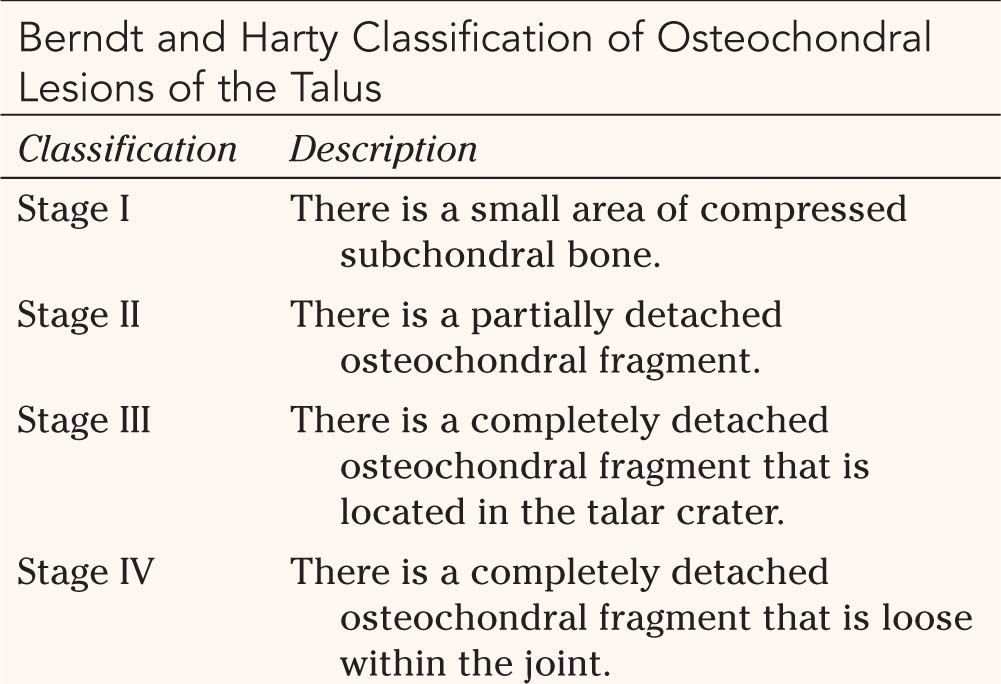
(a) Berndt and Harty classification—The Berndt and Harty classification (Table 14-2) is the original and most widely used classification.
(b) Ferkel CT classification
(c) Anderson MR classification
• Treatment (based on the Berndt and Harty classification)
(a) Stage I and II lesions and medial Stage III lesions—Stage I and II lesions and medial Stage III lesions are treated by cast immobilization for 6 to 12 weeks. If symptoms persist over 4 to 6 months, injuries are treated surgically as described next.
(b) Stage IV and lateral Stage III lesions—Stage IV lesions and lateral Stage III lesions are treated surgically. Smaller lesions are treated by surgical excision and drilling of the base of the lesion. This can be done either open or arthroscopically. Larger lesions involving over one-third of the articular surface are treated with operative reduction and fixation of the fragment. The use of bone graft is controversial. Medial or lateral arthrotomies are usually satisfactory, but large posteromedial lesions may require a malleolar osteotomy. Nonweightbearing with aggressive range-of-motion exercises is continued for 8 to 12 weeks.


• Chronic lesions—Chronic lesions should be suspected in patients with persistent symptoms after appropriate conservative treatment for an ankle sprain. Symptoms are usually activity-related and include pain, locking, and swelling. These lesions may not be visible on plain X-ray films, and a bone scan, an MRI, or both modalities may be helpful. MRI can assess stability by demonstrating the presence or absence of a fibrous attachment or fluid in the base of the fragment and in the fragment bed. The treatment for unstable chronic lesions is similar to that for acute lateral Stage III and Stage IV lesions. Ankle stiffness and arthritis are common with chronic lesions.
6. Dislocations involving the talus—Talar dislocations are high-energy injuries; 10% to 15% of these injuries are open.
• Subtalar dislocation—These are relatively rare injuries accounting for about 1% of all injuries to the foot. Subtalar dislocations occur with dislocation of both the subtalar and talonavicular joint. They are usually high-energy injuries, but may occur after small injuries. It is important to distinguish subtalar dislocations based on energy (high or low) and direction of dislocation in terms of treatment and prognosis.
• Anatomic classification:
(a) Medial subtalar dislocations occur with forceful inversion of the foot while in plantar flexion. These are the most common, and 40% have an open injury.
(b) Lateral subtalar dislocations occur with forceful eversion of the foot while in plantar flexion. These are usually higher energy with higher incidence of open injuries with over half being open.
(c) Posterior dislocations may occur with hyper plantar flexion
(d) Anterior dislocations are very rare and may result from a traction injury.
• Radiographs—Plain radiographs including three views of the foot and ankle are required for full evaluation. After reduction, plain films should be repeated to look for concentric reduction of the subtalar and talonavicular joint. Broden’s views can demonstrate reduction at the subtalar joint. Postoperative plain films and CT scans can further assess for associated impaction fractures or osteochondral fractures that may occur at the talonavicular or subtalar joint or evaluation of incarcerated fragments.
(a) Documentation of a complete neurovascular exam is crucial both pre- and postreduction.
(b) Reduction consists of knee flexion, traction/countertraction at the foot, recreation of the injury force, and direct pressure to the talar head as the calcaneus is gently manipulated back into position. This should be done in a timely fashion to reduce tenting of the skin and possible skin necrosis.
(c) Open injuries
• Irrigation and debridment
• Since lateral dislocations are higher-energy injuries, many require secondary grafting or flap procedures.
(d) Irreducible joints—If the joint cannot be reduced closed, then open reduction must be performed through an anteromedial or anterolateral approach to the talus
• Medial dislocations
• Buttonholing of the talar head through the extensor retinaculum
• Entrapment of the extensor digitorum brevis
• Entrapment of the lateral branch of the deep peroneal nerve
• Impaction of the navicular onto the talar head
• Lateral dislocations
• Impaction of the navicular onto the talar head
• Entrapment of the talar head by the posterior tibial tendon or flexor digitorum longus
(e) Postreduction
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






