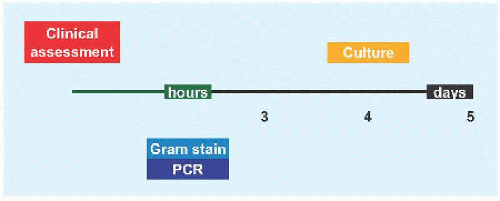
Musculoskeletal infections risk life, deformity, and disability. Infections and their treatment are evolving. Pyarthritis due to Hæmophilus influenzæ has declined due to vaccination. Antibiotic resistance is rising, for example, methicillin-resistant Staphylococcus aureus (MRSA) is the causative pathogen in up to 1/3 of cases, is more invasive, and leads to more complications. Diagnosis is improving with new modalities, for example, polymerase chain reaction. Duration of intravenous administration of antibiotics and total duration of therapy have been shortened significantly.
Osteomyelitis is twice as frequent as pyarthritis. This increased rate may be due to MRI detection of bone infection before radiographic change. Musculoskeletal infections show no gender predilection. Presentation skews to the middle of the first decade (6.6 years).
SELECT ORGANISMS
Bacteria may be distinguished morphologically as coccus (Greek κοκκοζ: “grain, seed”), rod or bacillus (Latin baculus = Greek βακτηρíα: “staff, cane”), vibrio (comma shaped), spirilla (spiral), and spirochete (tightly coiled). The organisms may occur in pairs (diplococcus), for example, Neisseria; in chains, for example, Streptococcus; in bunches, for example, Staphylococcus (Greek σταψvλη: “grape”); in filaments, for example, Actinobacter; and in complex structures resembling fungi, for example, Nocardia.
Gram-positive bacteria are characterized by a thick cell wall containing many layers of peptidoglycan and teichoic acids, which retain crystal violet in the Gram stain technique (Danish scientist Hans Christian Gram, 1853-1938). Gram-positive cocci are the most common pathogens in musculoskeletal infections. By contrast, Gram-negative bacteria have a relatively thin cell wall consisting of a peptidoglycan layer surrounded by a second lipid membrane containing lipopolysaccharides, the endotoxin responsible for much of their toxicity. Acid-fast bacteria, like Mycobacterium, are resistant to decolorization by acids during staining procedures (e.g., Gram stain), on account of the high lipid content of its wall (mycolic acid), which also contributes to virulence and resistance. L-form bacteria are strains of bacteria that lack cell walls. The main pathogenic bacteria in this class is Mycoplasma.
Certain genera of Gram-positive bacteria, such as Clostridium tetani (puncture wounds), form resistant endospores that may lie dormant for millions of years. Aerobic organisms use oxygen as the electron acceptor, while anaerobic organisms use other inorganic compounds (e.g., nitrate, sulfate, carbon dioxide) as electron acceptors, in a redox reaction that releases energy to synthesize ATP and drive metabolism.
Type of pathogen depends upon several factors:
Age. While Staphylococcus aureus is most common overall, Gram-negative bacteria and in particular Kingella kingæ account for more than half of infections in children under 4.
Vaccination history. Vaccination against Hæmophilus influenzæ B in the last decade of the 20th century has essentially eliminated pyarthritis due to this organism compared with a prevaccination rate of 1/3 of pyarthritis.
Host environment. Because of its ability to rapidly develop a biofilm, Staphylococcus epidermidis is of particular concern to patients with implants.
Socioeconomics. Haæmophilus influenzæ remains relevant in developing countries lacking vaccination programs.
Geography. Tuberculous spondylitis, rare in North American children, remains a significant burden in Africa.
Staphylococcus Aureus
New strains of this Gram-positive bacterium may be methicillin (MRSA) or vancomycin resistant. MRSA secretion of the necrotizing toxin Panton-Valentine leukocidin results in more invasive infection, longer hospitalization, more surgery, and higher complication rates.
Staphylococcus Epidermidis
This Gram-positive bacterium is responsible for nosocomial infection. It is a threat to patients who are immune compromised. The ability to form biofilms on implants is a major virulence factor. It is a frequent contaminant in laboratory analysis.
Kingella Kingæ
Infections by this Gram-negative coccobacillus are rising, in particular in infants. Presentation is benign, including fever in less than 1/5 of children and a normal C-reactive protein (CRP) in more than 1/3.
Propionibacterium Acnes
This ærotolerant anaerobic Gram-positive bacterium is a commensal colonist of the sebaceous glands of the skin around puberty. The indolent nature of this organism explains the delayed presentation of postoperative infection (including revision), in particular in spine surgery, where it requires implant removal for eradication.
Pseudomonas æruginosa
Opportunistic Gram-negative rod that rarely causes disease in the healthy, except when a physical barrier is breached, such as after a puncture wound to the sole of the foot in a shoe. It also is found in the setting of immune compromise, such as in the gastrointestinal tract of a child with leukæmia and the lungs in cystic fibrosis.
Salmonella
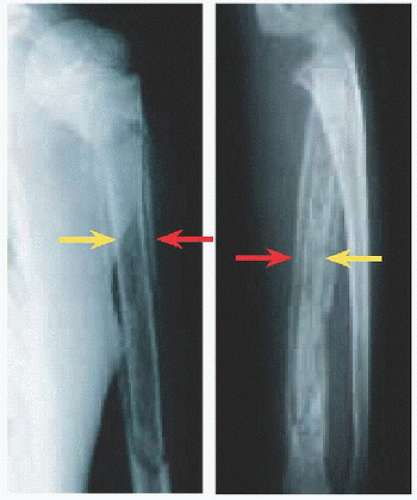
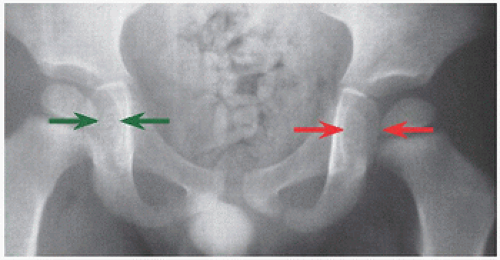
This Gram-negative enterobacterium is of particular concern in children with sickle cell disease. Capillary occlusion secondary to sickling may infarct the gut, permitting Salmonella invasion. Reticuloendothelial dysfunction and expanded marrow with sluggish flow leads to osteonecrosis with Salmonella infection. The infection is distinguished by diaphysial involvement [A], multiple sites, and a high rate of complications due to vasculopathy and immune compromise.
Borrelia Burgdorferi
This spirochete causes Lyme disease (Old Lyme, Connecticut, USA), a zoonosis transmitted from rodents by the Ixodes tick. Lyme disease is characterized by a delayed, warm though not itchy, target rash, termed erythema chronicum migrans, and pyarthritis. The disease also may affect the heart and central nervous system. Be alert to travel and exposure history: due to the relative indolence of pyarthritis, delay in diagnosis is typical.
EVALUATION
Physical Examination
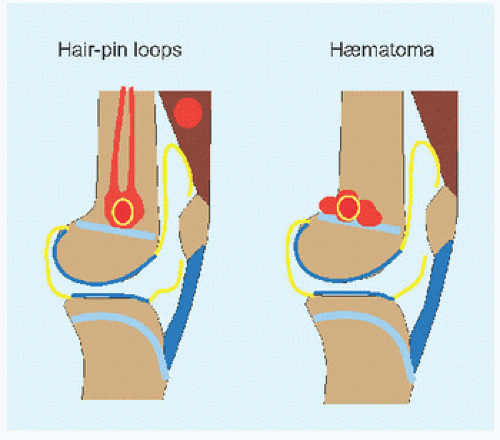
Take the temperature. Perform a screening examination first. Is the child in distress? This suggests an overwhelmed host worthy of expeditious attention. It argues against more benign confounding conditions such as transient synovitis. Similarly, lack of movement of, or bearing weight on, a limb, known as “pseudoparalysis,” is a sign of such extreme pain that the child will not use the affected part. Even if the examiner tries, the child will splint to present joint rigidity. In children, infected joints do not move; by contrast, only half of adjacent joints show reduction of motion in osteomyelitis. Look for inflammatory signs in the soft tissues, including swelling, redness, and warmth [A]. In order to relax these inflamed soft tissues, joints are flexed and at the hip rotated lateralward [A]. Percuss the bone to determine tenderness: this transmits force effectively to the bone while manipulating surrounding soft tissues less than palpation. Check the skin for stigmata that may predispose to infection, such as a pock or a laceration.
Imaging
Röntgenogrammes Signs of infection include the following:
Soft tissue swelling. This includes alteration of cutaneous contour, distortion of intermuscular planes, and contrasting densities.
Joint diastasis. At the hip, measure the distance between proximal femoral epiphysis and medial wall of acetabulum [B]. An effusion may be sufficiently large to dislocate a joint.
Periosteal elevation. This represents repair of osseous destruction.
Bone loss. A reduction of bone density of >30% is necessary before there are radiographic changes.
Röntgenogrammes are significant only if positive; negative images are inconclusive.
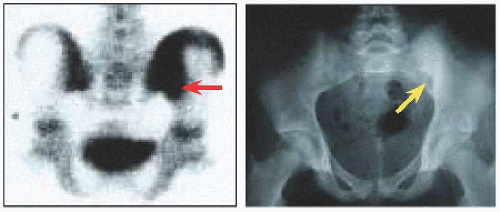
Scintigraphy This is indicated for clinical suspicion of osteomyelitis with normal röntgenogrammes. Technetium (99mTc) medronic acid is taken up preferentially by bone, concentrating (hot) where bone is inflamed. The immediate or flow phase (seconds after injection) assesses bone perfusion. The second or blood pool phase (minutes) is a measure of surrounding vascularity, as capillary dilatation slows the flow of blood. The third or delayed phase (hours) is a reflection of bone turnover. Reduced uptake (“cold” scan) is concerning for infarction and osteonecrosis, which limit antibiotic access. The scintigramme is unaffected by bone or joint aspiration.
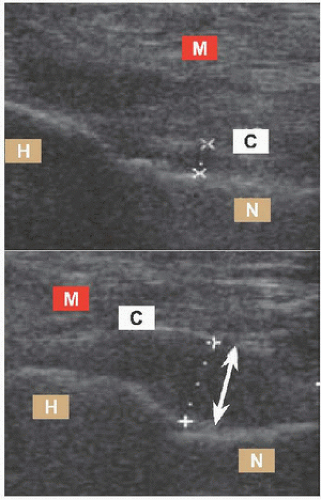
Ultrasound This is indicated for evaluation of the joint (in particular axial), such as effusion [D], and soft tissue, such as abscess. It is noninvasive, nonradiating, dynamic, portable, versatile, and cheap. However, it is user dependent, both for technique and for interpretation. Both quantitative and qualitative assessment of joint effusion is possible. At the hip, >2 mm elevation of the capsule off the neck of femur at the anterior joint recess defines distension. Echogenicity of the fluid suggests pus. Synovial membrane hypertrophy distinguishes transient synovitis (absent) from infection or other inflammatory process (present). Joint aspiration may be facilitated by ultrasonogramme, which confirms articular location of the needle. False negatives may occur early in disease, before sufficient fluid has accumulated to be detectable.
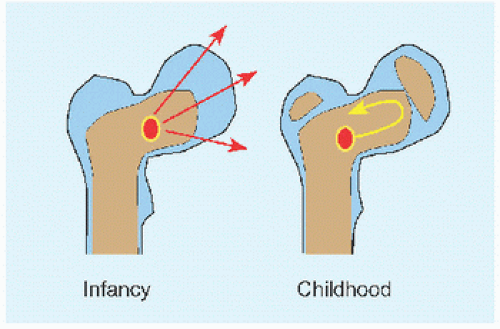
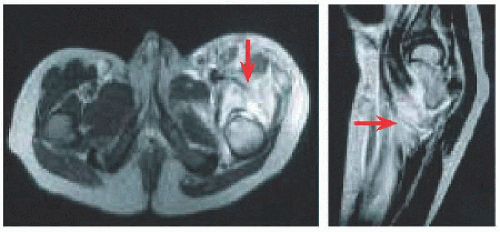
MRI This shows soft tissue best [E]. It also shows bone and its reaction. The modality allows for early identification with high sensitivity, before röntgenogrammes change, and provides anatomic detail for surgical planning. Gadolinium enhancement enables identification of infection of nonossified cartilage, including the epiphysis. This is a tissue target for MRSA and Kingella kingæ. Thus, treatment may be instituted earlier to mitigate damage from these pathogens.
Exercise sobriety and correlate MRI findings with the entire evaluation of the child. Because it reveals everything in such detail, it may raise alarm and promote zealous intervention. Remember that it requires sedation for the young child who will not lie still.
CT/PET This may be superior to MRI in monitoring response to treatment for osteomyelitis and in distinguishing ongoing infection from repair. However, the radiation dose limits the use of this modality.
Laboratory Studies
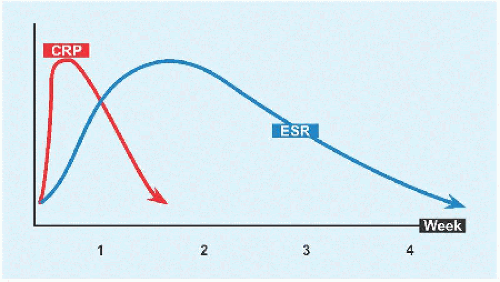
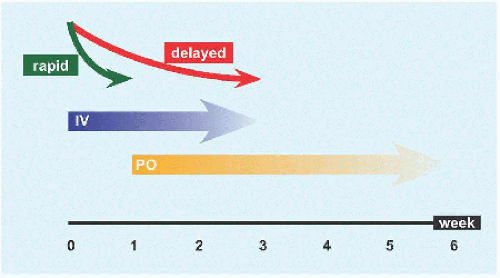
Blood Only half of children will have an elevated white blood cell count (WBC) > 12,000/mm3 at presentation. Most patients will have erythrocyte sedimentation rate (ESR) > 20 mm/h and C-reactive protein (CRP) > 20 mg/L; in combination, these markers approach 100% sensitivity for infection. Isolated musculoskeletal infection is characterized by a range of CRP 20 to 90 mg/L; CRP > 90 mg/L suggests disseminated infection. With successful treatment, ESR rises by 3 to 4 days and normalizes by 4 to 6 weeks, while CRP rises by 1 to 2 days and normalizes within 2 weeks [F]. ESR is useful for long-term follow-up and CRP for the acute treatment period.
Bone and joint This may be fluid from arthrocentesis or blood from bone or surgical specimen. The emergency setting, where the child may be sedated and before antibiotics are administered, is an opportunity to obtain fluid directly from the site of infection, rather than peripherally from a vein. If an appendicular joint is swollen, stick a needle in it. Decompression in this case may be therapeutic, by decreasing bacterial load, in addition to diagnostic. Infected metaphysial bone is soft. Insert a needle while aspirating in the event that there is a periosteal abscess. Once bone is encountered, advance the needle while rotating through a small arc to burrow into the bone, from where a blood specimen may be aspirated. At operation, physical deep and superficial tissue is preferable to swabs.
Gram stain may show bacteria. WBC > 50,000/mm3 with predominance of polymorphonuclear leukocytes in joint fluid is consistent with infection, although there may be overlap with juvenile idiopathic arthritis.
Culture Only half of blood, joint, and bone specimens will yield an organism. The rate is reduced by antibiotics, of which administration should be delayed in the stable child until all specimens are obtained. For Kingella kingæ, nasopharyngeal cultures (due to colonization) are significantly more positive than joint fluid.
Polymerase chain reaction Heat-stable polymerase selectively amplifies, using complementary primers, a specific region, or target of DNA after melting the double helix into independent strands. It provides results within 3 hours. It identifies fastidious organisms difficult to grow in culture, such as Kingella kingæ. It accelerates identification of virulent pathogens, such as MRSA, allowing earlier treatment to limit their morbidity. Early identification also promises more targeted antibiotic regimens, reducing iatrogenic bacterial resistance.
Due to diagnostic dilemma, burden of disease, and gravity of negative outcomes, diagnostic criteria have been developed for pyarthritis of the hip [G]. Added to this has been repeat presentation, suggesting deterioration during a period of observation. Remember that these are guidelines and not rules.



 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access