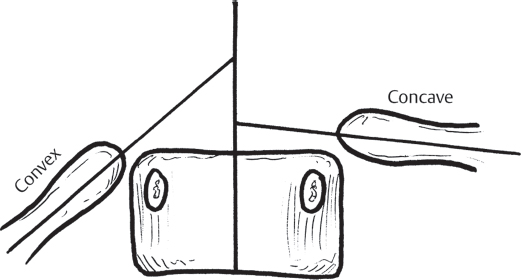
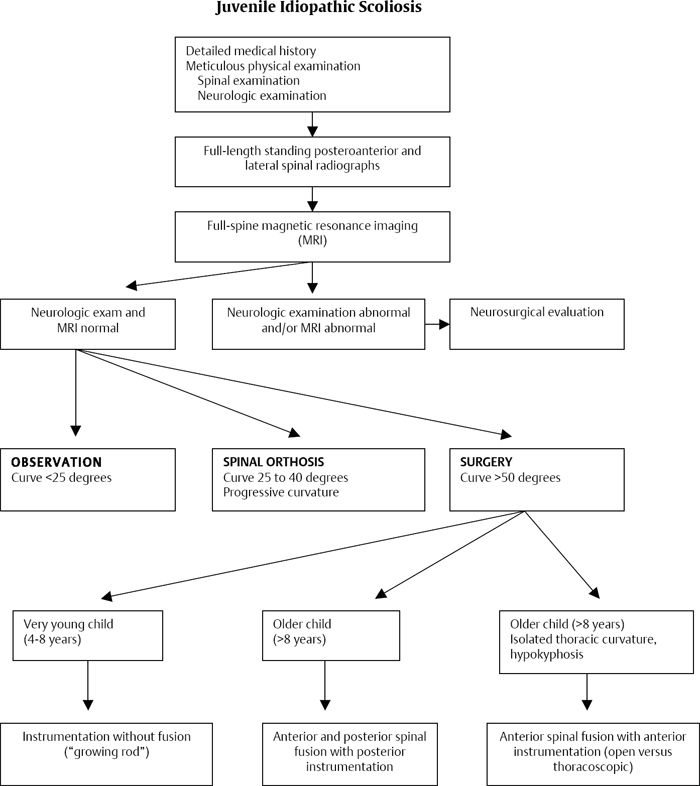
37 Infantile idiopathic scoliosis is a coronal plane deformity of the spine exceeding 10 degrees diagnosed prior to the age of 3 years. Weinstein prefers the classification of early-onset idiopathic scoliosis. Infantile scoliosis differs from adolescent scoliosis in that males are more commonly affected than females and the curve patterns are levoconvex (apex toward the left) in 75% of reported cases. The etiology is unknown, but the main theories include intrauterine molding and postnatal pressure. A segmental radiological study of the spine and rib cage in children with progressive infantile scoliosis determined that the thorax is narrower and the upper chest is funnel-shaped. These findings suggest vertebral rotation is predictive of progressive deformity. By definition, idiopathic infantile scoliosis excludes: 1. Congenital deformities, such as hemivertebrae and spinal dysrhaphism 2. Neuromuscular conditions, such as cerebral palsy, spina bifida, muscular dystrophy, and spinal muscular atrophy 3. Trauma 4. Infection 5. Neoplasm, especially neurofibromatosis and spinal cord tumors (primitive neuroectodermal tumor of infancy) 6. Metabolic bone disease (osteomalacia) 7. Connective tissue diseases (osteogenesis imperfecta, Marfan and EhlersDanlos syndromes) The history should determine whether the spinal deformity was present at birth or developed prior to age 3. A history of associated cardiac, genitourinary, or pulmonary problems should be obtained. There is also an association of inguinal hernias with infantile scoliosis. The physical examination should document neurocutaneous lesions, hairy patches, or nevi. The curve pattern should be determined, since the majority of infantile idiopathic scoliosis apices are levoconvex. The sagittal alignment should be documented along with the coronal deformity. Shoulder height asymmetry and pelvic obliquity should be evaluated. There should be evaluation for any chest wall deformity, including pectus carinatum, pectus excavatum, and thoracic insufficiency syndrome. Chest wall mobility should be assessed. Leg-length discrepancy should be assessed as well as range of motion in the spine and extremities. A complete and thorough neurologic examination should be performed, including motor, sensory, and deep tendon reflexes. Babinski and abdominal reflexes should be documented. Imaging should begin with routine radiographs. The radiograph should document coronal and sagittal plane deformity, associated congenital deformities, and the rib-vertebral angle difference (Fig. 37.1). Any congenital deformity should be further evaluated with computed tomography (CT). CT should be used sparingly because of the radiation exposure with this study. If there are congenital deformities documented, then magnetic resonance imaging (MRI) needs to be obtained to exclude an associated spinal cord abnormality; ~ 30 percent of children with congenital scoliosis have associated intraspinal abnormalities, including tethered spinal cord, syringomyelia, lipoma, and diastematomyelia. Other imaging studies can include ultrasound in the neonate to assess any spinal dysraphism. If associated intraspinal abnormalities are documented, then further diagnostic evaluation, including renal ultrasound and echocardiogram, is recommended to exclude congenital cardiac and renal defects. Laboratory studies with serum chemistry may be obtained to exclude metabolic bone disease and infection. Electrodiagnostic studies may be considered to rule out neuromuscular scoliosis. Fig. 37.1 The rib-vertebral angle difference is calculated by subtracting the convex value from the concave value at the apical vertebra of a thoracic curve. The first stage of treatment in the child with infantile scoliosis is to exclude an associated anomaly, such as cardiac anomalies, genitourinary anomalies, or pulmonary insufficiency. Careful evaluation for inguinal hernia also must be done. As long as there is no sagittal plane deformity and no congenital deformities, infantile scoliosis should be observed for progressive deformity. A rib-vertebral angle difference exceeding 20 degrees has a prognostic significance for progressive scoliosis. Spinal orthotic management should be considered for documented progressive deformity that exceeds 25 degrees, especially if the rib-vertebral angle difference exceeds 20 degrees; however, limited success with orthotic management is reported. Cast immobilization may also be considered for a progressive deformity. Serial cast correction can be successful in infants with idiopathic curves less than 60 degrees if started before 20 months of age. Surgical intervention for infantile scoliosis should be considered only for the child with progressive deformity despite cast and/or orthotic management. Surgical intervention with combined anterior and posterior convex epiphysiodesis does not prevent progressive deformity in infantile scoliosis. Submuscular or subcutaneous distraction rods have been shown to be effective in initial correction and subsequent maintenance of correction of the spinal deformity during growth. This can be combined with apical epiphysiodesis for treatment of the more severe deformity. Complications associated with growing rod treatment are frequent and can be reduced by use of dual rods, submuscular placement, limiting the number of lengthening procedures, and delaying initial implantation of the growing rods if possible. Spinal growth over the instrumented spine averages 1 cm per year of serial distractions. Newer instrumentation may produce better correction of the deformities. Preliminary results using the vertical expandable prosthetic titanium rib (VEPTR) in large-magnitude curves appear promising. Infantile scoliosis without associated congenital deformity carries a much better prognosis than adolescent scoliosis does. The majority of patients improve either without treatment or with casting/orthotic management and do not require surgical intervention. Children with sagittal plane deformities of the spine usually have an unrecognized congenital deformity and are much more likely to have progressive deformity. The main complication associated with infantile scoliosis is the unrecognized congenital deformity, neuromuscular pathology, or metabolic abnormality accounting for the spinal deformity. Operative treatment using spinal instrumentation without arthrodesis can be complicated by spontaneous arthrodesis and failure of trunk growth. Instrumentation problems are common, resulting in unplanned surgical procedures; surgical complications are directly proportional to the number of surgical procedures performed. Abel MF. Infantile idiopathic scoliosis. J Neurosurg Spine 2009;11(1):1–2, discussion 2 PubMed The importance of this reference is the documentation of limited success using orthotic management for infantile scoliosis. Bess S, Akbarnia BA, Thompson GH, et al. Complications of growing-rod treatment for early-onset scoliosis: analysis of one hundred and forty patients. J Bone Joint Surg Am 2010;92(15): 2533–2543 PubMed This reference reviewed multicenter experience using growing rods in early-onset scoliosis in 140 patients. Complications and treatment recommendations are discussed. Blakemore LC, Scoles PV, Poe-Kochert C, Thompson GH. Submuscular Isola rod with or without limited apical fusion in the management of severe spinal deformities in young children: preliminary report. Spine 2001;26(18):2044–2048 PubMed This reference reviewed 29 patients with progressive early-onset scoliosis. These patients underwent a submuscular Isola rod. Eleven patients also had apical anterior arthrodesis. Mean deformity improved from 66 degrees to 38 degrees with this treatment program. Campbell RM Jr, Smith MD, Mayes TC, et al. The characteristics of thoracic insufficiency syndrome associated with fused ribs and congenital scoliosis. J Bone Joint Surg Am 2003;85-A (3): 399–408 PubMed This article defines thoracic insufficiency syndrome with respiratory insufficiency, loss of chest wall mobility, worsening of deformity (based on three-dimensional imaging), and decline in predicted vital capacity. Treatment is discussed with expansion thoracoplasty. Diedrich O, von Strempel A, Schloz M, Schmitt O, Kraft CN. Long-term observation and management of resolving infantile idiopathic scoliosis: a 25-year follow-up. J Bone Joint Surg Br 2002;84(7):1030–1035 PubMed This article describes 42 patients with infantile idiopathic scoliosis, 34 patients followed for over 25 years. Twenty of the patients were treated with casting and 14 were treated with therapy. No progressive deformity was noted with this treatment regimen. There was no significant difference in the two treatment groups. The rib vertebral angle difference exceeding 20 degrees was prognostic for progressive deformity. Grivas TB, Burwell GR, Vasiliadis ES, Webb JK. A segmental radiological study of the spine and rib—cage in children with progressive infantile idiopathic scoliosis. Scoliosis 2006;1:17 PubMed This article describes a radiological study of the spine and rib-cage in children with progressive infantile scoliosis. Pathological findings are reviewed and predictive of progressive deformity. James JIP. Two curve patterns in idiopathic structural scoliosis. J Bone Joint Surg Br 1951;33-B (3): 399–406 PubMed This article describes the possible etiology of infantile scoliosis and describes similarity to other positioning abnormalities at birth. Lonstein JE, Bradford BS, Winter RB, Ogilvie JW. Moe’s Textbook of Scoliosis and Other Spinal Deformities. Philadelphia, Pennsylvania: WB Saunders Co; 1995 This text provides an excellent review of treatment alternatives in infantile scoliosis. Marks DS, Iqbal MJ, Thompson AG, Piggott H. Convex spinal epiphysiodesis in the management of progressive infantile idiopathic scoliosis. Spine 1996;21(16):1884–1888 PubMed This study evaluated 22 patients with a 10-year follow-up after combined anterior and posterior convex epiphysiodesis. This treatment alone does not prevent progressive deformity in idiopathic infantile scoliosis. Mineiro J, Weinstein SL. Subcutaneous rodding for progressive spinal curvatures: early results. J Pediatr Orthop 2002;22(3):290–295 PubMed This study reviewed 11 patients who failed nonoperative management for early-onset scoliosis. The patients underwent consecutive distraction of subcutaneous rods. Two patients also had anterior apical arthrodesis. One patient had no change in the deformity, with all other patients demonstrating improvement in the deformity and documented spinal growth with a mean of 2 centimeters over the course of treatment. Prahinski JR, Polly DW Jr, McHale KA, Ellenbogen RG. Occult intraspinal anomalies in congenital scoliosis. J Pediatr Orthop 2000;20(1):59–63 PubMed This reference describes 31 patients with congenital scoliosis evaluated with MRI. Nine of the patients had documented intraspinal abnormalities, consistent with a 30% positive findings on MRI study. Sanders JO, D’Astous J, Fitzgerald M, Khoury JG, Kishan S, Sturm PF. Derotational casting for progressive infantile scoliosis. J Pediatr Orthop 2009;29(6):581–587 PubMed This reference describes the method of serial casting in infantile scoliosis and the successful management in children with curves less than 60 degrees and started prior to 20 months of age. Schulz JF, Smith J, Cahill PJ, Fine A, Samdani AF. The role of the vertical expandable titanium rib in the treatment of infantile idiopathic scoliosis: early results from a single institution. J Pediatr Orthop 2010;30(7):659–663 PubMed This reference reviews the preliminary results using the VEPTR in large-magnitude infantile scoliosis deformity. Suh SW, Sarwark JF, Vora A, Huang BK. Evaluating congenital spine deformities for intraspinal anomalies with magnetic resonance imaging. J Pediatr Orthop 2001;21(4):525–531 PubMed This reference evaluated 41 patients with congenital scoliosis. Thirty-seven patients had failure of formation, 19 patients had failure of segmentation, and 4 patients had mixed deformities. Thirteen intraspinal abnormalities were diagnosed based on MRI study. Weinstein SL. The Pediatric Spine: Principles and Practice. New York, NY: Raven Press; 1994 This is an excellent overview of all pediatric spine conditions and management.
Infantile Scoliosis
![]() Workup
Workup
![]() Spinal Imaging
Spinal Imaging
![]() Special Diagnostic Testing
Special Diagnostic Testing
![]() Treatment
Treatment
![]() Outcome
Outcome
![]() Complications
Complications
Suggested Readings
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






