Steven J. MacDonald
Indications for Revision Total Hip Arthroplasty
INTRODUCTION
In the year 2000, of the 183,000 total hip replacements performed in the United States, 31,000 (~17%) were revision procedures.1 With an ageing population and a widening of the indications, the incidence of revision total hip arthroplasty (THA) will continue to have a major impact on patients and the adult reconstructive surgeon. Revision total hip replacements are amongst the most challenging of procedures and have a varied complexity and outcome. A thorough understanding of the indications for the procedure assists in preoperative planning (Chapter 6) and intraoperative decision making.
The most common diagnoses leading to revision THA include aseptic loosening, bearing surface wear, osteolysis, implant fracture, hip instability, infection, periprosthetic fractures, heterotopic ossification (HO), and leg length discrepancy.
The most common mechanisms of THA failure, and the reasons for revision, may be changing over time. Homesley et al.2 reported their institution’s experience over a 10-year period. In 1990, the indications for revision total were aseptic loosening (49.4%), infection (17.9%), hemiarthroplasty failure (16.7%), periprosthetic fracture (9.3%), instability (6.2%), leg length discrepancy (0.6%), and no cases of polyethylene wear. By 2000, the indications had changed to aseptic loosening (52.4%), infection (10.7%), instability (10.7%), periprosthetic fracture (7.5%), hemiarthroplasty failure (7.0%), polyethylene wear (6.9%), and leg length discrepancy (4.8%). Of particular note is the increasing indication of polyethylene wear which had not been a concern in the earlier series.
The main indications for revision THA are hip pain or dysfunction, progressive bone loss, and infection. Hip pain and/or dysfunction leading to revision THA may be caused by mechanical implant failure (loosening, wear, implant fracture), recurrent hip dislocation, or periprosthetic fracture. Progressive local bone loss, most commonly due to osteolysis, around the implant also may be an indication for revision, even in the absence of pain. A final indication for revision (in one or two stages) is infection, which usually causes local hip pain but may also cause systemic sepsis.
Aseptic Loosening Aseptic loosening is the most common diagnosis leading to revision THA. The Swedish hip registry in 2002 reported 60% of revisions were for aseptic loosening.3 Loosening may affect the acetabular component, the femoral component, or both. For cemented implants, aseptic loosening of the acetabular component is thought to predominantly be caused by periprosthetic wear debris that infiltrates the bone-cement interface and causes linear osteolysis and implant loosening. In some cases, however, mechanical detachment of the cement mantle from the bone or the implant from the cement may occur as the initiating factor.
For cemented femoral components, failure may occur due to loosening of the implant at the prosthesis-cement interface (so-called “debonding” of the implant) or at the bone-cement interface. More detailed information on this topic is provided in Chapter 4 entitled “Mechanisms of Failure.”
In uncemented acetabular and femoral components, loosening most commonly occurs when bone fails to grow into or onto the acetabular component. Failure of previously well-fixed implants may occur when a large amount of bone loss occurs in association with osteolysis, thereby destabilizing the implant.
Revision surgery in cases of aseptic implant loosening may be indicated for two reasons. The most common reason is pain (and/or dysfunction) associated with the loosening process. Many patients experience pain due to motion between the implant and the bone. Pain commonly occurs with the initiation of weight bearing, may be somewhat better after a few steps have been taken, and then typically worsens again as the patient walks further. This pattern of pain has been called triphasic. Pain typically is most severe in the groin or buttock when acetabular component loosening occurs and typically is most severe in the thigh when femoral component loosening occurs. Patients with loosening often also have a limp (antalgic gait), although a limp can also be caused by other factors such as muscle weakness.
Revision hip replacement also may be indicated when the loosening process leads to change in implant position causing poor biomechanics of the hip and associated hip dysfunction (e.g., femoral component subsidence leading to ineffective abductor function).
Finally, revision hip surgery for aseptic loosening may be indicated when it causes marked bone loss. Substantial bone loss due to mechanical abrasion of bone by loose implants or by particle debris access to interfaces in association with loose implants can leave the patient at risk for periprosthetic fracture or lead to circumstances in which revision surgery will be more difficult in the future. In such circumstances, revision may be indicated to stop the cycle of progressive bone loss.
Acetabular Revision. Acetabular revision most commonly is indicated for aseptic loosening or bearing surface wear. Other indications for acetabular revision include hip instability due to suboptimal cup position and infection.
Radiographic criteria for cemented cup loosening include migration or a complete radiolucent line at the bone-cement interface. Criteria for uncemented acetabular component loosening include migration, implant position change, broken fixation screws, and a complete radiolucent line of >1 mm at the implant-bone interface. A subtle—but not perfectly specific—finding often associated with early loosening of an uncemented cup is development of a radiolucent line in zone three of the implant-bone interface in combination with increasingly sclerotic bone in zone one.
Revision of the acetabular component, with retention of a functional femoral component—so-called isolated acetabular component revision—carries some unique risks. Exposure is more difficult. Especially if the femoral component is nonmodular, appropriate soft tissue balancing can be hard to achieve, and consequently, instability risk may be higher. Moskal et al.4 reported their experience in 32 hips with an average follow up of 8.1 years. They reported excellent stem survival with only 1 failure, but a 19% failure rate of the revised acetabulum. Jamali et al.5 also reported on their experience with isolated acetabular revision in 95 patients. They reported a reoperation rate for the femoral component of 8% at an average of 130 months, while the acetabular component had a 10-year survival of 90.5%. The major problems were an 8% dislocation rate and a 13% incidence of nerve palsy. They found that the dislocation risk in patients with a monoblock component was reduced with the use of a greater trochanteric osteotomy to adjust soft tissue tension.
Femoral Component Revision. Femoral revision is most commonly indicated for aseptic loosening. Other less common indications include osteolysis, hip instability, implant fracture, periprosthetic femur fracture, and infection. Criteria for definite loosening of cemented and uncemented components have been outlined, although they are not universally agreed upon. Cemented stems can be considered definitely loose if there has been migration of the component, fracture of the cement mantle, or a broken femoral component. Stems with a continuous radiolucent line at the bone-cement interface are considered probably loose, and those with a radiolucent line at 50% to 99% of the bone-cement interface are possibly loose.6 Uncemented femoral components can be considered osteointegrated if there is endosteal new bone, with no associated sclerotic lines in the region of the porous surface. If there is a failure of bone ingrowth, then reactive sclerotic lines are present in the area of porous coating. The component is considered to have fibrous fixation if these lines are parallel and nonprogressive and there is no migration of the component. The presence of subsidence, angulation, or shed particles from the porous coating suggests that the component is unstable.7
At the time of femoral component revision, optimal management of the stable acetabular component must be addressed. A well-fixed modular uncemented component provides the opportunity to perform a liner exchange and bone grafting of acetabular defects, when necessary. Beaule et al.8 reported their results with this technique and found the survival rate of the acetabular component to be 98.7% at 5 years and 93.5% at 10 years after the femoral revision. No hip showed recurrence or expansion of pre-revision periacetabular osteolysis. They concluded from their study that revision of a stable cementless acetabular component, solely on the basis of its duration in vivo, or the presence of periacetabular osteolysis, does not appear to be warranted.
Loose femoral stems articulating with well-fixed cemented acetabular components are a more difficult management issue. Two studies that have looked at this issue have found satisfactory results but have differed in their recommendations for predicting which cups will tend to fail. A large series from the Mayo Clinic9 showed the rate of survival of retained acetabular components was 96.9% at 5 years, 89.3% at 10 years, and 78.7% at 15 years following the femoral revision. The best predictive factors for acetabular component survival were increasing patient age and a shorter duration of implantation (<7.5 years) prior to the revision. The authors’ indication for retaining the polyethylene cup included implants that showed no evidence of loosening or wear. In a different paper, Berger et al.10 used the radiological assessment of Ranawat et al.11 to determine the grade of acetabular component. They found that retention of well-fixed cemented acetabular components was associated with good clinical results but reported a 15% rate of loosening at 5 to 13 years of follow-up. They found all acetabular components with a grade of A, B, C, or D at the time of revision continued to function satisfactorily at last follow-up. In contrast to the Mayo Clinic study, they found that components that loosened had been in vivo for a relatively shorter, as opposed to longer, duration before the femoral revision compared with the components that did not loosen.
Osteolysis Osteolysis is thought to be predominantly due to an inflammatory response to foreign material released from arthroplasty articulations. This tends to be a silent disease with symptoms often appearing only when substantial osteolysis is present. The ability of plain radiographs to demonstrate the extent of osteolysis is poor for the acetabulum, but better for the femur. A recent study of pelvic osteolysis showed the presence of significant defects in 48% of asymptomatic hip arthroplasties.12 The frequency of revision for the related problems of bearing surface wear and osteolysis is increasing rapidly. Different fixation methods, components, and articulating surfaces have been used over the last four decades, but osteolysis continues to be one of the greatest challenges to long-term arthroplasty survival.
Revision surgery for implant wear and osteolysis may be indicated for several distinctly different reasons. Bearing surface wear may cause hip synovitis. This process is typically manifested by pain in the groin which may be due to a joint effusion, synovitis within the joint, or synovitis along the iliopsoas tendon sheath. Pain in some cases may alone be an indication for revision surgery. Severe bearing surface wear may lead to polyethylene wear through to metal with mechanical symptoms in the hip, which also may be an indication for surgery. Finally, and most commonly, marked bearing surface wear leads to periprosthetic bone loss. Indications for further surgery in the presence of bearing surface wear and periprosthetic bone loss are among the most difficult to define in revision hip surgery. Most agree that severe bone loss that leads to potential periprosthetic fracture is an indication to consider operative treatment. More commonly, osteolysis is identified before it is likely to lead to fracture. Osteolysis is understood to be a progressive disease. Most surgeons tend to operate earlier when periprosthetic bone loss is substantial at the time of diagnosis, occurs in younger patients, or occurs in patients with implants that are known to be associated with the high likelihood of substantial periprosthetic bone loss. If the osteolysis is diagnosed early, the surgeon may elect to discuss the problem with the patient, observe the process on a regular basis, and operate either when substantial bone loss has occurred and/or when bone loss is found to have progressed. CT scans and MRI scans with metal artifact suppression are now available that can more clearly define the amount of bone loss that has occurred. An important principle is that operative treatment is indicated to prevent bone loss from occurring, which would otherwise reduce the likelihood of a good outcome of revision surgery. Another general tenant of treatment is that the older and sicker the patient, the more reluctant the surgeon should be to operate for bone loss alone.
Acetabulum.
UNCEMENTED CUPS. The osteolysis pattern in uncemented cups differs from cemented components. In uncemented cups, osteolysis tends to be more ballooning in nature and can occur around screws, screw holes, dome holes and the edge of the component. Despite the presence of marked osteolysis, component stability may be maintained through sufficient bone ingrowth.
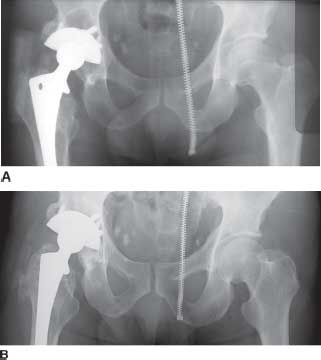
A challenging problem continues to be the role of revision surgery in asymptomatic patients with well-fixed acetabular components who demonstrate evidence of significant wear and/or osteolysis on radiographs (Fig. 6-1). It is often difficult for the patient to understand the need for further hip surgery and its associated risks when the hip is still functioning well. Early surgical intervention when the component is still well fixed preserves bone stock and is technically less challenging than when significant bone loss has occurred that may require extensive reconstruction. These advantages must be balanced against the surgical risks. Dislocation rates of up to 25% were reported both for isolated head and polyethylene liner exchange in early series.13 As surgeons have gained experience with isolated head and liner exchange and optimize intraoperative factors such as soft tissue tension and femoral head diameter, the dislocation rate appears to be falling. Surgical approach also may be an important factor; the dislocation rate was much lower with the use of a direct lateral approach in a recent report.14
FIGURE 6-1. A: 47-year-old asymptomatic patient 5 years following primary THA for posttraumatic osteoarthritis demonstrating significant acetabular osteolytic defect. B: Patient 3 years following polyethylene exchange and lesional bone grafting.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree