Jay R. Lieberman
Venous Thromboembolism Prevention
PROPHYLAXIS FOLLOWING TOTAL HIP ARTHROPLASTY
PROPHYLAXIS FOLLOWING TOTAL KNEE ARTHROPLASTY
DURATION OF THROMBOPROPHYLAXIS
Total knee and hip arthroplasty are extremely successful procedures that improve the quality of life of patients. In 2002, approximately 193,000 total hip and 43,000 revision total hip arthroplasties and 381,000 total knee and 35,000 revision total knee arthroplasties were performed.1 Despite the efficacy of these procedures, the incidence of venous thromboembolic disease (VTED) is as high as 60% following primary total hip arthroplasty and 85% following primary total knee arthroplasty without prophylaxis.2 It is essential that patients receive appropriate prophylaxis because the first manifestation of VTED may be a fatal pulmonary embolism.
Despite many well-designed clinical studies analyzing the safety and efficacy of different modalities of prophylaxis against VTED, an ideal prophylactic regimen has not been identified. The selection of a prophylaxis agent is a balance between efficacy and safety. In addition, ease of use, patient compliance, and cost also influence selection of a prophylaxis agent.
The focus of this textbook is revision total joint arthroplasty. The rate of revision surgery in North America has continued to increase, with an estimated annual rate of 8.2% for revision total knee arthroplasty and 17.5% for revision total hip arthroplasty.1 Two recent studies report pulmonary embolus rates of 0.9% to 0.93% in primary total hip patients compared to 0.79% to 0.8% in revision total hip patients within the first 3 to 6 months following surgery in patients on prophylaxis.3,4 To our knowledge, there are no reported rates of pulmonary embolism following revision total knee arthroplasty. Unfortunately, limited data are available on prophylaxis to prevent VTED after revision total hip or knee arthroplasty. There are however, many studies on different prophylaxis regimens for primary hip and knee arthroplasty. We highlight where alterations in prophylaxis are required for revision procedures. In addition, we discuss controversial areas related to prophylaxis including duration of therapy, the influence of regional anesthesia, and the impact of decreased hospital stays on the selection of prophylactic agents.
PATHOGENESIS
A total hip or knee arthroplasty is a potent stimulus for the development of VTED. Thromboembolic disease is manifested clinically as two different entities after total hip and knee arthroplasty. Proximal thrombus formation is more commonly associated with total hip than total knee arthroplasty.5 There is a strong association between proximal clot formation and symptomatic pulmonary embolism.6–8 In contrast, following total knee arthroplasty, approximately 90% of the thrombi formed occur in the calf veins and proximal (popliteal or femoral) thrombus formation occurs infrequently.2 The majority of calf thrombi are small, are clinically asymptomatic, and have low risk of associated embolization or chronic venous insufficiency. However, unsuppressed thrombi of the calf have the potential to propagate proximally, which can lead to a pulmonary embolism.6–9 In a study of 273 total hip and knee arthroplasty patients, 41 (15%) developed asymptomatic distal deep vein thrombi.8 Using serial duplex ultrasonography, 7 (17%) of these 41 patients had evidence of proximal propagation by postoperative day 14. Furthermore, in another study assessing the natural history of thromboembolic disease after total hip arthroplasty, 4 of 23 patients (17%) with an untreated calf vein thrombosis developed a symptomatic pulmonary embolism.10
The formation of thrombi is associated with Virchow’s triad of venous stasis, hypercoagulability, and endothelial injury that occurs during the perioperative phase.11 Venous stasis may occur secondary to the positioning of the limb during surgery, localized postoperative swelling, and decreased activity level following the operation.12–14 A significant reduction in the venous capacitance and outflow of both legs has been demonstrated during hip arthroplasty and may last as long as 6 weeks postoperatively.15 This may be exacerbated during dislocation of the hip and femoral prosthesis insertion by occluding the femoral vein.12,16,17 Total knee arthroplasty is usually performed with a tourniquet on the thigh and with the knee in a flexed and subluxated position. Venous outflow has been shown to be reduced for several days after total knee arthroplasty in the operated limb.18
Tissue thromboplastin and other clotting factors are released during the course of the surgical procedure and can aggregate in regions of venous stasis. The production of multiple markers of thrombin generation (prothrombin F1.2, thrombin-antithrombin complex, fibrinopeptide A, and d-dimer) was analyzed at various time points during a total hip arthroplasty to define the period of thrombogenic stimulus.19 These markers did not increase with preparation of the acetabulum or osteotomy of the femoral neck but rose significantly during reaming of the femoral canal and insertion of the femoral component. The levels of fibrinopeptide A and D-dimer were greater after insertion of a cemented femoral component compared to a noncemented component. It is theorized that manipulation of the femoral canal leads to release of thromboplastin in the bone marrow or fat, which causes a thrombogenic stimulus. In a similar study with knee arthroplasty, significant increases in thrombotic markers were noted following tourniquet deflation.20 However, manipulation of the femoral canal during total knee arthroplasty is probably the thrombogenic stimulus rather than the tourniquet itself.21 Recently, with the advent of computer navigation systems, intramedullary guide rods are not required during preparation of the femoral canal, and this may potentially reduce the formation of clots associated with this procedure. Further study of the factors that promote thrombogenesis during total knee arthroplasty is necessary.
Injury to the endothelium may occur during positioning and manipulation of the extremity as well as from thermal injury from bone cement.12,16,22 Endothelial damage initiates the activation of tissue factor and other clotting factors (Fig. 2-1).23,24 Blood loss during surgery can result in a reduction of antithrombin III (AT III) and inhibition of the endogenous fibrinolytic system, which further leads to a hypercoagulable state and promotes thrombus propagation.16,25–28
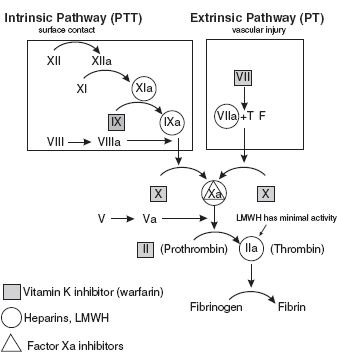
FIGURE 2-1. Coagulation cascade indicating sites of inhibition by various chemoprophylactic agents.
EPIDEMIOLOGY
Patients who undergo total joint arthroplasty are at particularly high risk for the development of VTED independent of risk factors that already have been identified (Table 2.1).7,30,31 Prior to routine prophylaxis, deep vein thrombosis (DVT) developed in 45% to 85% of total hip and knee arthroplasty patients. Proximal clots developed in 18% to 36% of total hip patients and in 5% to 22% of total knee patients.2 Fatal pulmonary embolism rates were reported to be between 0.5% and 2.0% in total hip patients.6,7,25,26,28,30,32–34 Fatal pulmonary embolism from total knee replacement ranges from 0.1% to 1.7%.35–37
TABLE 2.1 Risk Factors for Venous Thromboembolic Disease
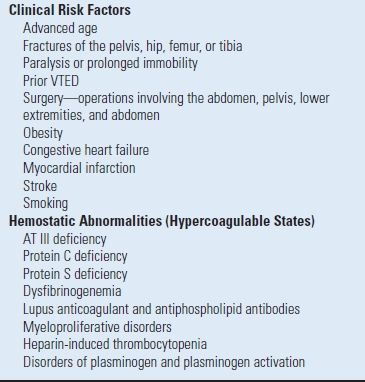
Adapted from Anderson FA, Jr, Spencer FA. Risk factors for venous thromboembolism. Circulation 2003;107(23 Suppl 1):I9–I16, with permission.
VTED after total joint arthroplasty adds a considerable burden to health care cost and a significant morbidity to the patient.38,39 In one study reviewing 11,607 total hip replacements, the most common cause of readmission to the hospital following total hip arthroplasty was thromboembolic disease.40 Of the 208 readmissions within a month of surgery, 26% were due to a DVT or pulmonary embolism. Additionally, since the duration of hospital stays following total joint arthroplasty has decreased, the occurrence of DVT after discharge has increased. In a review of 19,586 hip and 24,059 knee arthroplasty patients from 1991 to 1993, the incidence of symptomatic DVT was 2.8% (566 patients) for total hip and 2.1% (508 patients) for total knee arthroplasty patients.41 The diagnosis of thromboembolism was made after discharge in 76% of the total hip patients compared to 47% of total knee arthroplasty cases. The median time of diagnosis of VTED was at 17 days after total hip arthroplasty and 7 days after total knee replacement.
Finally, in high-risk patients, symptomatic clots can develop despite adequate prophylaxis. Factor V Leiden mutation, activated protein C resistance, antiphospholipid antibody syndrome, Protein C and S deficiency, or impairment of the fibrinolytic system can potentially increase the risk of the development of VTED.42–44 Slightly higher rates of symptomatic DVT were noted in patients with factor V Leiden mutation, prothrombin mutations, and genetic abnormalities related to AT III.42–47 However, none of the authors recommended routine preoperative screening for gene mutations because the overall rate of thrombophilic disorders is low and the risk of symptomatic DVT is not markedly increased in these patients.
PROPHYLAXIS FOLLOWING TOTAL HIP ARTHROPLASTY
A variety of pharmacologic and mechanical agents have been used to decrease the risk of venous thromboembolism after total hip arthroplasty. The pharmacologic approaches have included standard heparin, low molecular weight heparin (LMWH), warfarin, fondaparinux, and aspirin. Mechanical approaches include sequential intermittent pneumatic compression boots (PCBs), intermittent plantar compression, compression stockings, and early mobilization.
The selection of a prophylactic agent is one of the few areas of orthopaedic surgery where there is evidence-based medicine to help make clinical decisions. Although randomized controlled trials are the gold standard to assess the efficacy of a drug, it must be noted that most of the VTED studies use asymptomatic DVT detected by venogram as a surrogate outcome measure. There is some concern about the clinical relevance of these clots especially when there is no difference is noted with respect to proximal clot formation and symptomatic PE rates with various agents. Again, the selection of a prophylaxis agent is a balance between safety and efficacy.
It has been assumed that patients undergoing revision total hip arthroplasty are at a higher risk for developing DVT than are those undergoing primary hip arthroplasty due to longer operative time, increased endothelial damage, increased blood loss, and more comorbid conditions due to increased age at time of operation.48 However, a revision total hip arthroplasty encompasses a wide range of procedures, from a relatively simple liner exchange to a complex acetabular reconstruction for pelvic discontinuity. Intuitively, the risk of DVT may rise with increasing complexity of surgery, but there is no clinical study to support this hypothesis.
There are very limited data with regard to DVT following revision total hip arthroplasty. We are unaware of any large randomized clinical trials comparing different prophylactic regimens following revision total hip arthroplasty. Phillips et al.4 had a rate of symptomatic pulmonary embolus of 0.9% (537 of 58,521) for primary total hip arthroplasty and 0.8% (104 of 12,956) for revision total hip arthroplasty. Twenty six percent of the pulmonary emboli that occurred after primary total hip arthroplasty developed within the first 2 weeks compared to 38% after revision surgery. The type of prophylaxis was not reported.
PHARMACOLOGIC METHODS
Heparin Heparin is a collection of glycosaminoglycans of varying lengths and molecular weights from 5,000 to 30,000 Da. The major anticoagulant effect of heparin is accounted for by a unique pentasaccharide that binds with high affinity to AT III (Fig. 2-2). The interaction of heparin with AT III produces a conformational change in AT III which accelerates its ability to inactivate thrombin, factor IX, and factor Xa. In order to inhibit thrombus formation, heparin binds to AT III and thrombin to form a ternary complex. Heparin molecules that contain less than an 18-saccharide chain are unable to form this ternary complex.49–51
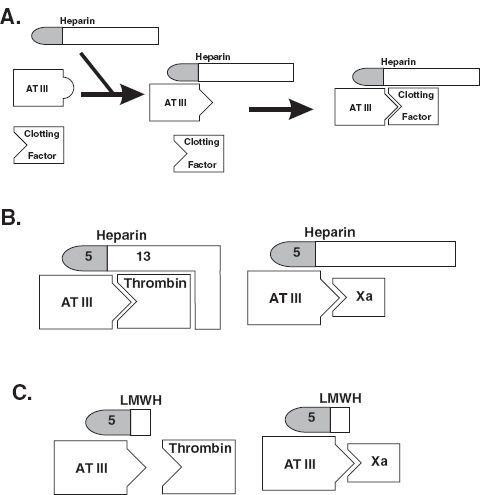
FIGURE 2-2. A: Binding of the heparin pentasaccharide to AT III accelerates binding of this complex to a clotting factor. B: Binding of heparin forms the AT III-heparin thrombin ternary complex and requires a 13-chain oligosaccharide sequence. No ternary complex is formed with the binding of factor Xa. C: LMWHs do not contain the 13-chain sequence and are unable to form an AT III-LMWH-thrombin ternary complex, but are able to bind preferentially to factor Xa.
Standard low-dose heparin (5,000 units administered subcutaneously twice daily) is not currently recommended in the prevention of DVT after total hip arthroplasty due to ineffectiveness.17,52,53 However, adjusted-dose heparin has been shown to be effective in limiting clot formation after total hip arthroplasty.32,53,54 Heparin is administered and adjusted to achieve an activated partial thromboplastin time (aPTT) of 1 to 5 seconds more than the hospital upper normal limit. However, due to multiple subcutaneous injections and frequent monitoring of the aPTT, adjusted-dose heparin has not become a popular thromboprophylactic modality.
Low Molecular Weight Heparin The LMWHs are derived from unfractionated heparin by chemical or enzymatic depolymerization yielding fragments relatively homogeneous in size, with molecular weights between 1,000 and 10,000 Da and a polysaccharide length <18. A minimum heparin chain length of 18 saccharides is required to simultaneously bind AT III and thrombin thus LMWHs are able to selectively inhibit factor Xa but not thrombin (Fig. 2-2).49–51 Pharmacologically, LMWH is substantially different from unfractionated heparin because it binds less to plasma proteins and endothelial cells, resulting in a more predictable dose profile, increased bioavailability and longer half-life among patients of differing weight.55 These biologic properties allow a fixed dose of LMWH to be used without the need for laboratory monitoring. Prophylactic doses of LMWHs do not increase the PTT or the rate of bleeding,51 but they can occasionally cause heparin-induced thrombocytopenia.56,57 The LMWHs are metabolized in the kidney and therefore should be used with caution in patients with renal insufficiency. Additionally, the use of LMWHs has been associated with the formation of spinal hematomas when used with epidural anesthesia.58 Specific guidelines have been developed to reduce the risk of bleeding with regional anesthesia and the use of LMWH prophylaxis (Table 2.2). Currently both enoxaparin and dalteparin are FDA approved for total hip arthroplasty.
TABLE 2.2 Regional Anesthetic Management of Patients on Anticoagulants
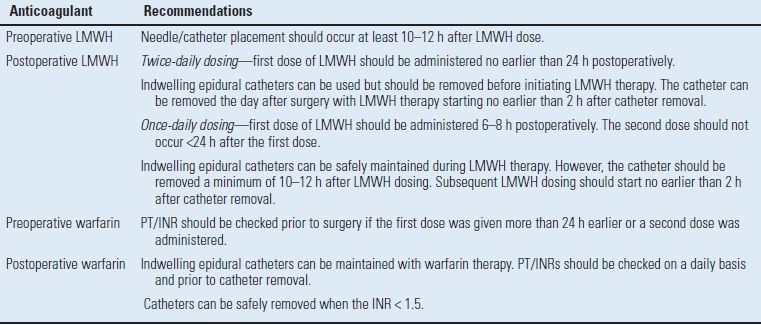
Adapted from Horlocker TT, Wedel DJ, Benzon H, et al. Regional anesthesia in the anticoagulated patient: defining the risks. Reg Anesth Pain Med 2004;29(2 Suppl):1–12.
A number of studies have shown that LMWHs reduce the risk of proximal and distal DVT by at least 70% compared to placebo.30,59–62 In two meta-analyses, LMWHs have been demonstrated to prevent VTED after total hip arthroplasty more effectively than unfractionated heparin with no difference in major hemorrhage.61,63 Additionally, LMWHs have been compared to warfarin in a number of multicenter randomized clinical trials64–68 (Table 2.3), which demonstrated that different LMWHs were more efficacious than warfarin (7% to 15% vs. 11% to 26%) in limiting proximal clot formation but were associated with higher bleeding rates (1.2% to 5.5% vs. 1.0 to 4.0%).
TABLE 2.3 Randomized Clinical Trials of Warfarin Versus LMWH After Total Hip Arthroplasty
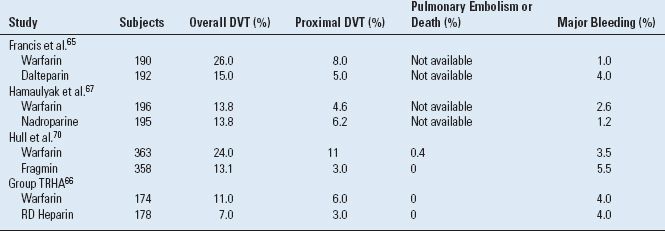
Adapted from Lieberman JR, Hsu WK. Prevention of venous thromboembolic disease after total hip and knee arthroplasty. J Bone Joint Surg Am 2005;87(9):2097–2112, with permission.
Hull et al.70 performed a multicenter randomized trial comparing dalteparin to warfarin, which included two LMWH treatment arms to assess if timing of prophylaxis affected safety and efficacy. Patients were randomized into three groups: a warfarin group who received 10 mg starting the evening of surgery followed by daily dosing to maintain an INR between 2.0 and 3.0, a preoperative dalteparin group who were administered a half-dose of dalteparin (2,500 IU) 2 hours prior to surgery followed by a second half-dose 4 hours after surgery (preoperative dalteparin), and a postoperative dalteparin group receiving a half-dose 4 hours after surgery. The dalteparin patients then received the standard (5,000 IU) dose beginning on postoperative day 1 and continuing prophylaxis for 5 weeks. The overall DVT rate was higher in the warfarin group (81 of 338, 24%) compared to both the preoperative dalteparin group (36 of 337, 10.7%, p < 0.01 vs. warfarin) and the postoperative dalteparin group (44 of 336, 13.1%, p < 0.001 vs. warfarin). The rate of proximal clot formation was 0.8% (3 of 364, p = 0.04 vs. warfarin) in the preoperative dalteparin group, 0.8% (3 of 358, p = 0.02 vs. warfarin) in the postoperative dalteparin group, and 4.4% (15 of 338) in the warfarin group. Symptomatic thrombi were less frequent in the preoperative dalteparin group (5 of 337, 1.5%, p = 0.02) and postoperative dalteparin group (10 of 336, 3.0%) compared to the warfarin group (15 of 338, 4.4%, p = 0.2). Overall bleeding episodes were similar among groups, but increased major bleeding at the surgical site was seen in the preoperative dalteparin group (p = 0.01). The results of this study suggest that a LMWH regimen in which prophylaxis is started either prior to or soon after the procedure results in a significant reduction in both total and proximal DVT formation. However, the higher bleeding risk associated with a preoperative dose of the LMWH is too high for this regimen to be accepted by most North American surgeons. The question is whether or not starting a half-dose of LMWH in the early postoperative period will increase the overall efficacy of the drug without increasing bleeding risk compared to an LMWH regimen started 18 to 24 hours after the surgical procedure.
Colwell et al.64 conducted another large multicenter randomized clinical trial evaluating the efficacy of enoxaparin and warfarin in preventing symptomatic DVT and pulmonary embolism after THA. Three thousand and eleven patients were randomly assigned to receive either enoxaparin twice daily beginning the morning after the surgical procedure or warfarin the night of the total hip arthroplasty with prophylaxis continuing for an average of 7 days. An analysis of inhospital DVT formation revealed a higher rate of symptomatic thromboembolic events in patients who received warfarin prophylaxis (17 of 1,495 patients, 1.1%) compared to enoxaparin (4 of 1,516 patients, 0.4%, p < 0.01). After hospital discharge, there was no difference in the symptomatic VTE rates between the warfarin (29 patients, 2.6%) and the LMWH (51 patients, 3.4%, P = NS) groups after 3 months. Major bleeding episodes were significantly more frequent in the enoxaparin group (18 of 1,516 patients, 1.2%), than in the warfarin group (8 of 1,495 patients, 0.8%, p < 0.05). The results of this study demonstrated that enoxaparin provides more effective symptomatic VTE prophylaxis than warfarin while the drugs were used in the hospital, but VTED rates were similar after hospital discharge. The LMWH was associated with higher bleeding rates.
The two LMWHs that are available in the United States have different dosing regimes. It is recommended that the initial dose of enoxaparin be administered 12 to 24 hours after the end of the surgical procedure to decrease the risk of bleeding. In contrast, a half-dose of dalteparin is administered 4 hours after the surgical procedure followed by a full dose on postoperative day 1. However, there have been no randomized trials comparing the efficacy of different LMWHs. Overall, the LMWHs are safe and effective agents in limiting the incidence of thromboembolic disease following total hip arthroplasty.
Warfarin Warfarin has been used for the past three decades and is the most commonly used single agent for prophylaxis following hip surgery.26,40,71–73 Warfarin produces its anticoagulant effect by interfering with the vitamin K–dependent clotting factors. Specifically, it blocks Vitamin K reductase, which limits carboxylation of glutamate and thereby inactivates clotting factors II, VII, IX, and X. Warfarin has several advantages including oral administration, cost, and ease of administration after hospital discharge.74 However, there are several drawbacks including frequent monitoring of the International Normalized Ratio (INR) and multiple drug interactions. Warfarin has a delayed onset of action for several days, which may reduce bleeding but leaves the patient relatively unprotected from thrombus formation during this period. Warfarin is effective in decreasing the prevalence of thrombosis by up to 60% for distal DVT and 70% for proximal thrombi when compared to no prophylaxis.30 Additionally, warfarin has been associated with a 1% to 5% rate of a major postoperative bleeding event.74–77
Warfarin prophylaxis is started with either a 5- or 10-mg dose the evening before surgery or a 10-mg dose the evening after surgery. If warfarin is started the evening prior to surgery, an INR may be obtained the morning of the surgery if spinal anesthesia is going to be used. Measurement of daily INR values determines subsequent evening doses of warfarin. Therapeutic INR levels of prophylaxis are between 1.8 and 2.5 with a target of 2.0. A dosing nomogram was shown to be able to simplify the management of warfarin prophylaxis.78 Some surgeons are reluctant to attain the target INR recommended for DVT prophylaxis in order reduce bleeding or postoperative monitoring, but this places patients at increased risk for DVT formation.79
At UCLA, we have had an extensive experience using warfarin prophylaxis for the past three decades.71,76 Lieberman et al.76 analyzed 1,099 patients after primary or revision total hip arthroplasty between 1987 and 1993.76 Twelve patients (1.1%) had a symptomatic pulmonary embolus with one fatality (0.1%). The incidence of a major bleeding event was 2.9% (32 patients) with a significantly increased risk of a postoperative hematoma development if the prothrombin time was >17 seconds. Patients with a history of symptomatic thromboembolic disease had a significantly increased risk of symptomatic pulmonary embolus (p = 0.001). The average duration of therapy was 15 days with no difference in symptomatic events with either 14 or 21 days of prophylaxis. This study also included 419 revision total hip arthroplasties (333 patients). The rate of symptomatic pulmonary embolism after revision total hip arthroplasty was 0.4% (2 of 418) compared with 1.5% (10 of 681) in primary hip arthroplasty (p = NS).
A meta-analysis of 52 randomized, controlled trials from 1966 to 1998 evaluated 10,929 total hip arthroplasty patients.80 Warfarin had the lowest rate of proximal DVT (6.3%), as well as the lowest rate of symptomatic pulmonary embolism (0.16%) but the second highest rate of distal thrombus formation (17.1%). There was no increase in the risk of major bleeding episodes postoperatively in patients taking warfarin compared to placebo.80 Warfarin has been shown to be more effective for prophylaxis against proximal deep vein thrombus than distal thrombus in several studies comparing warfarin with mechanical prophylaxis.81,82
Warfarin remains a safe and effective agent for prophylaxis following hip arthroplasty. Although it appears to be not quite as effective as the LMWHs in preventing VTED, there is a decreased risk of bleeding complications compared with LMWHs. Large randomized clinical trials are needed to fully compare warfarin with other treatment modalities such as mechanical devices and fondaparinux.
Aspirin Aspirin irreversibly inhibits cyclooxygenase and decreases localized platelet aggregation by blocking the production of thromboxane A2. Historically, aspirin has been an attractive prophylactic agent because it is an oral drug, is inexpensive, requires no monitoring, and can also reduce the risk of heterotopic ossification.83 Aspirin does lower the risk of thrombosis, and is associated with a slightly lower bleeding complication rate following total hip arthroplasty, but it is not as effective as either LMWHs or warfarin in preventing DVT.2,80
The Pulmonary Embolism Prevention Trial was a randomized controlled trial that included 4,088 patients undergoing elective total hip or knee arthroplasty to assess the efficacy of aspirin in VTED.84 The patients were randomized to 5 weeks of 160 mg aspirin (n = 2,047) started 1 day preoperatively or placebo (n = 2,041). There was no statistical difference in the incidence of symptomatic pulmonary embolus or DVT between the aspirin group (23 of 2,047, 1.1%) and the placebo group (28 of 2,041, 1.3%). There were eight pulmonary emboli in each group (0.4%, NS), with one death in the aspirin group and two in the placebo group. In addition, 16 patients required evacuation of a hematoma in the aspirin group (0.8%), versus 8 in the placebo group (0.4%); however, this difference was not statistically significant (p = 0.1). However, the value of this study is limited because there were numerous protocol violations in both groups of patients (32% of the patients received aspirin or another NSAID during the study period, and 35% received LMWH).
In a meta-analysis comparing multiple prophylaxis regimes, eight studies were included that used aspirin following total hip arthroplasty.80 Use of aspirin was associated with an incidence of proximal thrombus formation of 11.4% which was less than that of placebo (25.8%, p < 0.05). However, the distal DVT rate (19.7% vs. 22.4%), pulmonary embolism rate (1.3% vs. 1.5%), and symptomatic pulmonary embolus rates (0.32% vs. 0%) were not different between aspirin and placebo. The risk of a major bleeding event was 0.73% compared to 1.67% for warfarin and 2.22% for a LMWH. However, all of the studies included in the meta-analysis were single-center studies and only 687 patients were analyzed. Furthermore, the aspirin dose varied from 300 to 1,800 mg and two of the studies evaluated patients who were also treated with hypotensive epidural anesthesia, which impacts deep venous thrombosis rates. Although aspirin does appear to lower the risk of VTED following total hip arthroplasty, it is not as effective as either warfarin or LMWHs.
Fondaparinux The synthetic pentasaccharide fondaparinux selectively inhibits factor Xa, with no direct inhibition of thrombin.85–87 The antithrombotic activity of fondaparinux is due to AT III–mediated selective inhibition of factor Xa. Fondaparinux selectively binds to AT III, causing an irreversible conformational change at the binding site for factor Xa. Fondaparinux does not affect platelet activity or enhance fibrinolytic activity; however, moderate thrombocytopenia (50,000 to 100,000 platelets/mL) has been seen in up to 2.9% of patients.88 Since fondaparinux is metabolized in the kidney and excreted in the urine, renal impairment (creatinine clearance of <30 mL/min) is a contraindication for its use. A routine measurement of hematocrit, platelet count, and creatine levels is recommended prior to discharge for patients receiving fondaparinux. Fondaparinux has recently received Food and Drug Administration (FDA) approval for prophylaxis for total hip and knee arthroplasty and hip fracture patients.
Turpie et al.88 performed a randomized, double-blind multicenter trial comparing fondaparinux to enoxaparin in 2,275 consecutive patients undergoing elective total hip arthroplasty. Patients received fondaparinux 6 hours following the surgery, and enoxaparin 12 hours following the surgery. Patients in both groups received DVT prophylaxis for an average of 7 days (range 4 to 11 days for fondaparinux and range 5 to 11 days for enoxaparin). There was no significant difference in overall DVT formation between the fondaparinux (44 of 784, 5.6%) or enoxaparin (65 of 796, 8.2%, p = 0.099) groups. In addition, there was no difference in either the proximal clot rates for fondaparinux (14 of 186, 1.7%) versus enoxaparin (10 of 830, 1.2%, p = 0.42) or symptomatic pulmonary embolism rates (0.4%, vs. 0.1%, respectively). Major bleeding episodes were also similar in both groups (fondaparinux 20 of 1,128, 1.8% and enoxaparin 11 of 1,129, 0.09%, p = 0.11). Lassen et al.89 followed 2,309 patients randomized to either 2.5 mg of fondaparinux 6 hours postoperatively or 40 mg enoxaparin preoperatively. The overall rate of VTE was significantly decreased (47 of 908, 4%) in patients assigned to fondaparinux compared to enoxaparin (85 of 919, 9%, p < 0.0001). The rate of proximal DVT was lower with fondaparinux (1%) compared with enoxaparin (2%, p = 0.002). Major bleeding episodes were similar in both groups (4% vs. 3%, p = 0.11).
Fondaparinux appears to be as safe and effective as the LMWHs in providing prophylaxis following total hip replacement. However, more studies will need to be performed as fondaparinux becomes more widely used. There is a multicenter study under way to assess the safety and efficacy of fondaparinux when administered 18 hours after the end of the procedure.
MECHANICAL METHODS
PCBs and venous plantar compression devices (VPCs) both have been used to prevent DVT after total hip arthroplasty. The advantages of these devices are that there is no laboratory monitoring and no potential for bleeding and they are well tolerated and inexpensive. The major disadvantages are that patients do not receive prophylaxis when the devices are removed, prophylaxis cannot be continued beyond hospital discharge, and patient compliance is not consistent.90,91
Pneumatic Compression Boots PCBs reduce the venous stasis in the lower extremity by increasing the velocity of venous blood flow and enhancing local endogenous fibrinolytic activity.92,93 This secondary effect is caused by the release of endothelium-derived relaxing factor, which inhibits platelet aggregation and release of urokinase and/or tissue-plasminogen activator from the venous endothelium.94,95
A number of randomized trials have demonstrated that PCBs can limit distal thrombus formation but may not be as efficacious in reducing proximal clot rates in total hip arthroplasty patients.81,82,96–99 However, the true efficacy of PCBs is difficult to ascertain as many of these studies lack the statistical power necessary to draw adequate conclusions.73 In addition, there is concern that these devices may not provide adequate protection against proximal clot formation. Paiement et al.82 compared PCBs (66 patients) and warfarin (72 patients) after total hip replacement. The overall DVT rate was the same 17% (p > 0.05) in both groups; however, the location of the thrombi was different. PCBs offered better protection for calf thrombi, while warfarin offered better protection against proximal clots. Similarly, in a randomized study of 201 patients, the overall DVT rate was similar (31% vs. 27%, p > 0.05) for patients using warfarin compared to PCBs, but proximal thrombosis occurred in 12% of the PCBs versus 3% of the warfarin group (p = 0.01).97 In contrast, calf thrombus occurred in 12% of the PCB group versus 21% of the warfarin group (p = 0.02). Further study of PCBs is necessary before they can be recommended as a sole means of thromboembolic prophylaxis after total hip arthroplasty.
Venous Plantar Compression VPC mimics the hemodynamic effects that occur during normal walking. There is a large plantar venous system composed of one to four veins that is rapidly emptied with compression of the plantar arch during weight bearing. VPCs are usually better tolerated than the intermittent pneumatic devices that are applied to the whole leg.100
When compared to no prophylaxis or standard heparin, VPC has been demonstrated to decrease overall thrombosis rates with no adverse reactions.100,101 Two recent small randomized trials comparing VPCs to LMWHs have demonstrated the efficacy of these devices in preventing both proximal and distal thrombus formation.102,103 Warwick et al.103 performed a prospective comparison of a foot pump and enoxaparin on 274 total hip patients. DVT was detected by venography in 18% (24 of 136) of patients using VPCs and 13% (18 of 138) of patients taking enoxaparin. No statistical difference was found in the incidence of calf (5% vs. 4%) or proximal (13% vs. 9%) DVT in patients using foot pumps or enoxaparin respectively. In another study comparing VPC with a LMWH (fraxiparin), 3 of 100 patients in the foot-pump group developed a DVT compared with 6 of 100 patients in the fraxiparin group.102 All three thrombi in the foot-pump group were distal compared to four distal (p = 0.11) and two proximal clots (p < 0.05) in the fraxiparin group. Although the data appear promising, as of yet, VPC cannot be recommended as the sole means of prophylaxis until larger randomized prospective trials are performed comparing this mechanical device to other forms of chemical prophylaxis.
Compression stockings alone do not reduce the risk of thromboembolism acceptably and should not be considered as the sole prophylaxis option for patients who have had a hip arthroplasty.30,60,104,105 The role of compression stockings in combination with other modalities has not been completely investigated, although two recent studies found that the combination of compression stockings with venous foot pumps actually reduces the venous velocity.106,107 The use of compression stockings with PCBs did not have an additive effect on peak velocity of venous blood flow as measured in the superficial femoral vein.108 Further study on combination therapy is warranted.
PROPHYLAXIS FOLLOWING TOTAL KNEE ARTHROPLASTY
Total knee arthroplasty is associated with deep vein thrombus formation even more frequently than total hip arthroplasty2,30,66,81,109,110; however, the rates of symptomatic pulmonary embolism are greater in total hip arthroplasty.2 There are two special considerations when comparing hip arthroplasty to knee arthroplasty that deserve mention. The first is that the envelope of skin around the knee is less forgiving than the hip and does not tolerate hematoma formation as well. Therefore, surgeons are concerned about using prophylactic agents associated with higher bleeding rates. Secondly, the formation of a calf thrombus is more common than that of a proximal thrombus, and although most calf clots resolve, they can still propagate into the thigh. However, propagation of a proximal clot is more common. Again, the selection of a prophylaxis regimen is a balance between efficacy and safety.
Very limited data are available regarding the incidence of DVT following revision total knee arthroplasty.111 Because procedures are often longer with larger blood loss on older patients, it is assumed that patients undergoing revision total knee arthroplasty are at a higher risk for developing DVT than are those undergoing primary knee arthroplasty. Various trials have included small numbers of revision patients, but we are unaware of any study in the literature that compares different prophylactic regimes following revision total knee arthroplasty. As with revision total hip arthroplasty, the complexity of the revision total knee arthroplasty would influence management of prophylaxis. We currently recommend 2 weeks of prophylaxis after revision total knee arthroplasty, but a longer duration may be appropriate in cases with greater blood loss, those requiring extensive soft tissue dissection, and in patients with limited postoperative mobility. Further studies are needed to determine if these patients are at an increased risk of VTED.
PHARMACOLOGIC METHODS
Low Molecular Weight Heparin The LMWHs have been demonstrated in multiple clinical trials to provide effective and safe prophylaxis after total knee arthroplasty. There have been five randomized multicenter clinical trials comparing the efficacy of adjusted-dose warfarin prophylaxis and different LMWHs as prophylactic agents (Table 2.4).66–68,112–114 Pooling the data of all five randomized trials yields a distal DVT rate of 48% versus 33% for warfarin and LMWH, respectively. The respective rates of proximal DVT were 10.4% and 7.1%.2 LMWH appears to be more effective in limiting asymptomatic DVT, but rates of clinically significant bleeding were generally higher than with warfarin (2.8% vs. 1.2%).
TABLE 2.4 Randomized Clinical Trials of Warfarin Versus LMWH After Total Knee Arthroplasty
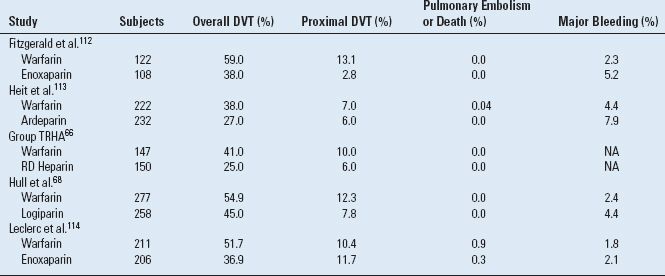
Adapted from Lieberman JR, Hsu WK. Prevention of venous thromboembolic disease after total hip and knee arthroplasty. J Bone Joint Surg Am 2005;87:2097–2112, with permission.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








