FIGURE 56-1. Anteroposterior (A) and lateral (B) radiographs of a distal femoral replacement knee arthroplasty. The collar on the intramedullary stem component is porous coated; extracortical bone bridges this portion of the implant and host bone.
Design of the articulating segment of a rotating hinge varies among manufacturers with corresponding differences in implant stability. A biomechanical study by Ward et al.1 of rotating hinge implants showed an association between the length and taper of the central rotational stem and stability of the implant. Prostheses with a short and/or markedly tapered central stem had greater instability. Howmedica (Stryker: Kalamazoo, MI), Techmedica (Sulzer Medica: Winterthur, Switzerland), Intermedics (Sulzer Medica: Winterthur, Switzerland), and Wright Medical/Dow Corning Wright (Arlington, TN) designs required at least 39 mm of distraction prior to dislocation, whereas the S-ROM design dislocated at only 26 mm and the Biomet implant at 33 or 44 mm depending of the thickness of the polyethylene tray used. The Link implant dislocated at 20 mm but only with failure of an antisubluxation feature. These results underscore the importance of understanding the unique characteristics of each manufacturer’s design.
INDICATIONS
In the revision TKA setting, the indication for use of a distal femoral replacement implant is extensive bone loss (Type 3 AORI bone defect2). While preliminary data show good results with large (30-mm) metal distal femoral prosthetic augmentations,3 more extensive bone loss may result from trauma (Fig. 56-2) or multiple failed arthroplasty procedures. In such cases, metal augmentation on the femoral component is inadequate and a choice must be made between implantation of a structural allograft combined with a noncondylar replacement femoral component (allograft-prosthetic composite or APC) and a distal femoral replacement implant.
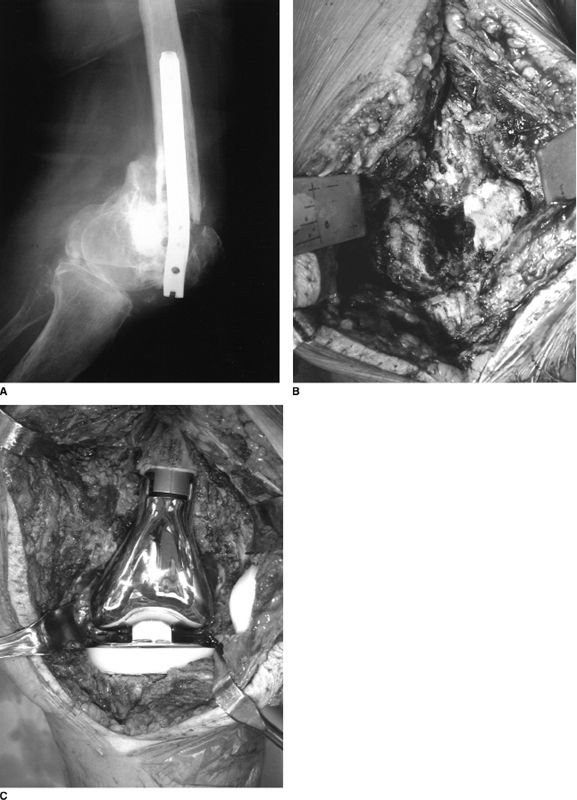
FIGURE 56-2. Elderly patient with extensive distal femoral bone loss related to four prior failed internal fixation procedures. (A) Lateral radiograph showing complex nonunion of the distal femur and prominent intra-articular hardware. (B) Intraoperative photograph showing intra-articular fracture with displacement of condyles, bone loss, and articular damage. (C) Intraoperative photograph of distal femoral replacement prosthesis.
An APC provides the theoretical advantage of bone stock restoration and some soft tissue adherence, but introduces the risk of failure of the allograft due to delayed union or nonunion, infection, or allograft fracture. A constrained articulation is still required with use of an APC as functional ligament healing to the allograft is unreliable. In a review of 12 patients treated with distal femoral allografts following periprosthetic femoral fracture after TKA, union occurred in nine of ten patients with radiographic follow-up.4 Three patients required additional surgery for complications. In a small series comparing complications and functional outcomes of irradiated APCs (11 patients) and bone ingrowth modular tumor prostheses (64 patients) for reconstruction following resection of the distal femur or proximal tibia for sarcoma, the limb salvage rate was 95% for patients with a tumor prosthesis compared with 64% for patients with an APC.5 Functional scores were also superior for the tumor implant patients. In cases of extensive distal femoral bone loss, the author favors use of a distal femoral replacement implant.
METHODS OF FIXATION
Fixation of the intramedullary stem of the femoral component of a distal femoral replacement implant can be achieved by various methods. Cement fixation is common, effective in long-term studies, and should be used in patients with poor bone quality. Press-fit stems are also available for patients with appropriate diaphyseal bone. Preliminary results with hydroxyapatite coating on the stem component are favorable6,7 as is a new method of fixation, compliant prestress fixation, which transmits dynamic physiologic stresses to the host bone resulting in bone ingrowth to the implant.8
Fixation may be augmented by extracortical bone bridging, namely bone which forms between the host bone and the implant (Fig. 56-1). Distal femoral replacement systems often have an option of a porous-coated collar on the intramedullary stem component to encourage the formation of this bone. Bone graft material is placed at the host-implant junction in the area of this porous coating prior to wound closure. Ward et al.9
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








