FIGURE 32-1. The Vancouver classification of periprosthetic femur fractures is the most widely used classification system. (Adapted from Duncan CP, Masri BA. Fractures of the femur after hip replacement. Instr Course Lect 1995;44:293–304, with permission.)
Treatment Algorithm Type A(G) fractures may occur in the presence of a well-fixed implant due to trauma. If the fracture is minimally displaced, nonoperative measures are appropriate, and healing can be anticipated in approximately 12 weeks. More commonly, these fractures occur in the setting of marked osteolysis of the greater trochanter, either with or without an episode of minor trauma. When the fracture is not markedly displaced, a period of time for healing (with bony or fibrous tissue) usually is allowed before revision to manage the underlying particle-generating process that led to periprosthetic osteolysis. Markedly displaced acute greater trochanteric fractures are considered for early reoperation and fixation because nonoperative treatment is likely to lead to nonunion, an abductor limp, and possibly hip instability.23 However, gaining union of these fractures, even with operation, is difficult, and there is a risk of operative complications. Consequently the risk versus benefits of acute operative fixation of a greater trochanter should be considered carefully before a decision is made for operative intervention.
Type A(L) fractures associated with a stable implant are rare and may be treated nonoperatively. Some A(L) fractures occur in the presence of local osteolysis, which eventually will require treatment for its own sake. Type A(L) fractures associated with a loose implant usually require femoral component revision.
Vancouver type B1 fractures most commonly are treated with internal fixation and prosthesis retention.24 When internal fixation is chosen as a treatment method, it is important to ascertain with certainty that the prosthesis is well fixed.25
A high rate of union with prosthesis retention now has been achieved using two different techniques.
Vancouver type B2 fractures typically are treated with revision arthroplasty to simultaneously treat the fracture and the loose implant. Nonoperative treatment26 rarely is appropriate because of a high rate of nonunion and malunion and the prolonged immobility required. With modern implants and techniques, a single-stage procedure that includes fracture fixation and implant revision almost always is possible.27
Vancouver type B3 fractures may be treated with tumor prostheses, allograft prosthetic composites,28 or newer revision techniques using uncemented implants that gain axial and rotational stability distal to the implant.
Vancouver type C fractures usually are treated with internal fixation using a retrograde in-tramedullary device or a plate. To avoid a high stress region that is subject to fracture between the stem tip and the new fixation device, overlapping of the fixation devices with the femoral component may be considered.
TREATMENT AND RESULTS
Vancouver Type A(G) Fractures Fixation of greater trochanteric fractures may be accomplished with wires, cables, suture, a cable grip claw, or cable plate.23 Preliminary experience with hook plates appears to be favorable for these difficult problems, and this technique may become the method of choice. These fractures often are transverse, and often involve a small piece of poor quality trochanteric bone; consequently, healing can be problematic. If healing fails, problems with pain, abductor insufficiency, and limp and hip instability are frequent.
When operative treatment is selected for minimally displaced fractures associated with os-teolysis, surgery frequently is delayed to allow the fracture to gain bony or fibrous union.29 By waiting 12 weeks or more, many of these fractures become sufficiently stable to allow reconstitution of a continuous sleeve of abductor, greater trochanter, and vastus lateralis before revision surgery is undertaken to treat underlying wear and osteolysis problems (Fig. 32-2). If surgery is pursued acutely, the fracture typically is unstable and may become displaced, and fixation of the very thin osteolytic bone can be very difficult or impossible. Hsieh et al.30 reported on 21 greater trochanteric fractures associated with osteolysis that occurred a mean of 11 years after THA. Seventeen fractures were minimally displaced and 15 of the 17 treated nonoperatively with crutches, and activity restriction healed clinically and radiographically. Four of four fractures treated with internal fixation and bone grafting healed.
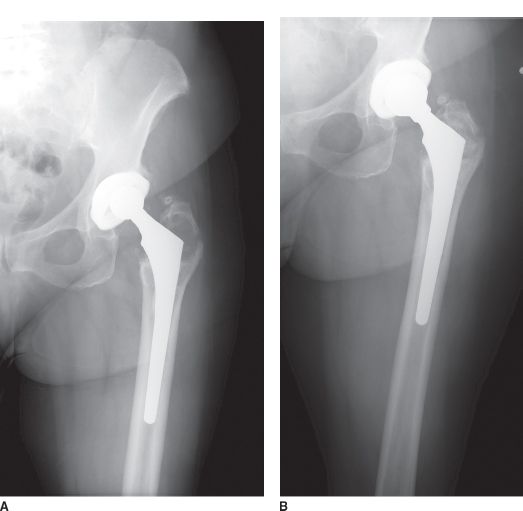
FIGURE 32-2. A: Radiograph of hip with periprosthetic fracture of greater trochanter associated with osteolysis. B: The fracture was allowed to heal with fibrous tissue, and then revision to treat the polyethylene wear and osteolysis was performed. Note the sleeve of abductors—greater trochanter—vastus lateralis has remained in continuity.
Vancouver Type A(L) Fractures A few A(L) fractures occur in the presence of a stable implant with associated periprosthetic osteolysis, and in such cases, elective surgery may be needed to manage the wear and osteolysis problems leading to fracture.
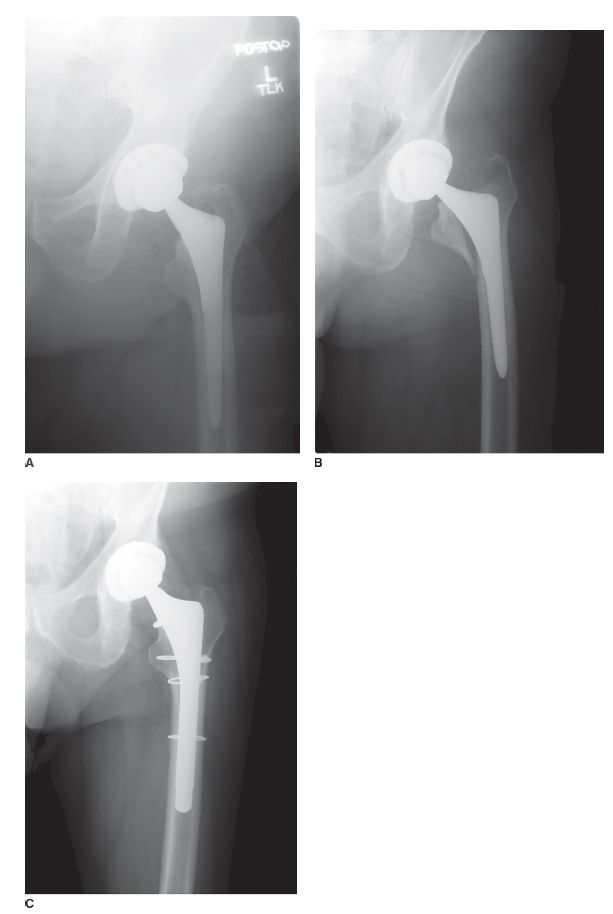
Recently an A(L) fracture pattern associated with early failure of uncemented tapered collarless implants has been identified.31,32 These fractures may occur “spontaneously” with sudden hip loading or be associated with unidentified intraoperative fractures that subsequently displace under load. The typical fracture involves a single posterior-medial bone fragment that includes the lesser trochanter and is associated with a loose implant that has subsided and rotated into a retroverted position (Fig. 32-3). In most cases, early reoperation is indicated. The implant is extracted, the fracture is reduced, and a new implant is placed. A new short or medium-length uncemented stem (extensively porous coated or fluted tapered modular) that does not rely exclusively on the fractured proximal bone for support is indicated. Preliminary results of fixation of these fractures with cerclage and insertion of a new stem have been favorable. Taunton et al.32 reported that 25 of 28 such fractures healed and had a stable implant at followup. However, three patients required further operation, two for infection, and one for hip instability.
FIGURE 32-3. A: Radiograph of hip after primary THA with uncemented tapered collarless stem. B: Hip radiograph after the patient fell, sustaining a Vancouver A(L) fracture of the proximal femur. The stem has subsided and is loose. C: Hip radiograph after re-vision of the femoral component with standard length, extensively porous coated stem.
Vancouver Type B1 Fractures Vancouver type B1 fractures most commonly are treated with internal fixation, although on rare occasions internal fixation with prosthesis revision is indicated. The two keys to obtaining satisfactory results when treating these fractures are (1) a mechanically strong construct, and (2) respecting the vascularity of the bone. Historic experience has shown that cerclage fixation alone or plate fixation with unicortical proximal screws alone, both provide insufficient fixation. Better surgical techniques and internal fixation devices33,34 have improved results of fixation of these fractures.35,36
Technique. Plates designed for combinations of cerclage cable and screw fixation provide fixation proximal and distal to the implant tip (and the fracture).37
Two main methods currently are favored to treat these fractures. The first involves fixation with an allograft strut or struts,38–42 usually in combination with a plate (Fig. 32-4). Typically, a plate is placed laterally through a vastus lateralis splitting incision, and a cortical strut graft is contoured and placed anteriorly (Fig. 32-4). The most frequent mode of failure of these constructs is failure of proximal fixation (Fig. 32-5). For this reason, the author prefers to fix the plate with both cables and screws proximal to the fracture. Proximal screws can be placed either in a unicortical mode or a bicortical mode (posterior to the prosthesis). Proximal screws (in addition to cables) add substantial strength to the construct and improve both rotational strength and resistance to bending failure. The strut graft is held in place with at least two cables distally and usually at least two cables proximally. The plate—which is usually a locking screw plate43—is fixed to bone with screws distally (Fig. 32-6). Care is taken not to devascularize the fracture site and surrounding bone. Host bone graft, if available, may be placed carefully around the fracture medially, avoiding muscle stripping.
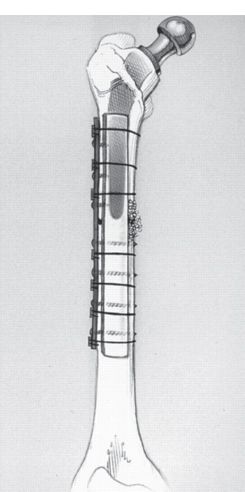
FIGURE 32-4. Diagram of Vancouver type B1 periprosthetic femur fracture treated with a lateral plate and anterior cortical strut allograft. Note that the plate is fixed proximally with both screws and cables. (Modified Haddad FS, Duncan CP, Berry DJ, et al. Periprosthetic femoral fractures around well fixed implants: use of cortical onlay allografts with or without a plate. J Bone Joint Surg 2002;84A:945–950, with permission.)
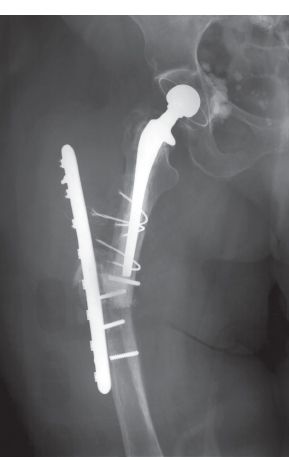
FIGURE 32-5. Hip radiograph demonstrating failed internal fixation of a periprosthetic femur fracture. A single, lateral plate with only cable fixation proximally provided less fixation than more modern methods.
FIGURE 32-6. A: Hip radiograph demonstrating Vancouver Type B1 femur fracture in elderly woman with poor bone. B: Hip radiograph after internal fixation with lateral locking plate and anterior cortical strut bone graft. C: The fracture healed uneventfully. D: Although the acetabular component demonstrated wear, it was retained because of the patient’s age and very low activity.
A second technique, which recently has been reported to provide good results, is the so-called bridge plating technique. A plate is inserted with minimally invasive methods, extraperiosteally, through small incisions proximal and distal to the fracture site. The fracture is reduced using indirect reduction methods, and then the plate is secured to the bone with screws (usually locking screws). The key to this technique is minimal disruption of the blood supply to the fracture and maintenance of the fracture hematoma, which has growth factors that promote healing. High rates of union have been reported in several series with this technique.
Results. Treatment of Vancouver B1 fractures with internal fixation was reported by Lindahl et al.44 to have a high rate of failure in the Swedish National Hip Arthroplasty Register. These poor results in part are explained because some fractures were misclassified as type B1 type fractures when in fact they were associated with loose implants. However, the results also emphasize that older methods of internal fixation, especially a single (nonlocking) plate have a high failure rate, and are unsatisfactory for these difficult problems.45,46
Modern treatment with a plate and cortical strut graft or two strut grafts in combination have had a much higher success rate. Haddad et al.,1 in a multicenter study, reported fracture healing in 39 of 40 hips treated with one of these two methods. The combination of a plate and strut graft has been shown to provide more fixation than two struts in bench testing,47,48 but strut grafts alone for fixation have produced good clinical results in several series.
Ricci et al.49 described use of a single lateral plate (usually a locking plate) in combination with indirect fracture reduction, extraperiosteal plate placement, and minimal soft tissue dissection. Fifty of 50 periprosthetic fractures healed in satisfactory alignment using this method.
Vancouver Type B2 Fractures The majority of periprosthetic fractures occur in the setting of implant loosening. Lindahl et al.,50 reporting on periprosthetic fractures in the Swedish National Hip Arthroplasty Register found 66% of fractures after primary THA and 50% of fractures after revision THA occurred in association with a loose stem.
Vancouver type B2 fractures are treated with implant revision with concomitant fracture stabilization. Modern reconstruction methods take advantage of the fracture to provide access to the failed implant, using the fracture as a window to facilitate implant removal. Most commonly, the fracture is stabilized satisfactorily with a long-stem femoral implant and cerclage fixation, but when necessary, plates or cortical strut grafts may be added for additional fracture fixation.
Improved femoral implants have greatly increased the success of one-stage revision of Vancouver B2 femur fractures.51 Almost all fractures now can be treated with a one-stage procedure at the time of the acute fracture. One-stage operation precludes the need for prolonged traction, or immobilization. Two-stage treatment, sometimes used historically, has the drawbacks of a high risk of malunion and nonunion, and ultimately producing more rather than less difficult reconstructions. Furthermore, two-stage treatment subjected patients to long periods of immobilization that are poorly tolerated and led to a high risk of morbidity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree