FIGURE 7-1. A: Radiograph of failed total hip arthroplasty with acetabular and femoral component templates overlaid electronically. Note that the varus deformity of the proximal femur becomes more apparent with templating. B and C: Radiographs of same hip after revision total hip arthroplasty. An extended greater trochanteric osteotomy was performed to help manage the varus femoral remodeling. The postoperative radiographs closely approximate the preoperative plan.
Priorities in Revision Total Hip Arthroplasty The surgeon must carefully consider the priorities in a revision arthroplasty, to provide the best likelihood of short- and long-term success.11–13
The first priority must be to gain secure implant fixation. For a good clinical result, the patient must gain a hip, which produces little pain; and to be painless, implants must be stable. Therefore, placing an implant, which is stable and has a high likelihood of remaining stable, must be the highest priority.14–19 Likewise, providing a hip joint that is stable and does not dislocate also is important for a satisfactory clinical result. Any procedure that compromises on the likelihood of implant or hip stability, even for some potential future benefit, may be unsuccessful (Fig. 7-2).

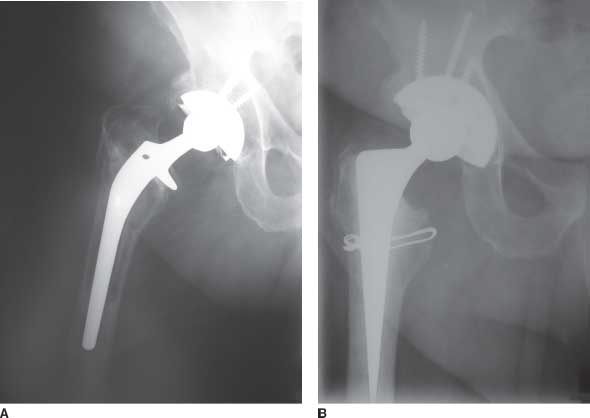
FIGURE 7-2. A: Radiograph of hip after revision of the acetabular component. The operation failed due to acetabular component loosening and hip instability. The cup chosen was too small to fill the large bone defect. B: Another revision operation was performed, which provided good component and hip stability using a larger socket. The second revision might have been avoided if a larger implant was used at the first revision.
The next priority is to choose a form of reconstruction that can be performed with sufficient technical ease and consistency to provide good clinical results and a low rate of complications.20,21 A procedure, which the surgeon can execute consistently, has practical advantages over one with theoretical benefits that is difficult to execute.
Finally, the surgeon should strive to choose surgical approaches and implants that preserve soft tissues and bone for the future.18,22–25 Particularly in younger patients, the potential for subsequent operations should be considered and the surgeon should strive to avoid burning bridges for the future (Fig. 7-3). However, the surgeon also must consider that placing too high a priority on future bone preservation at the cost of a higher risk of early re-revision due to marginal implant stability also should be avoided.26 Repetitive reoperations and repetitive failures create a vicious cycle of bone loss and soft tissue damage that may eventually lead to a serious complication or an unreconstructable hip. Effectively stopping the cycle of revisions, with one well-done operation, often is worth more extensive implant fixation, even if a little more bone is used for fixation (Figs. 7-4 and 7-5). As revision total hip arthroplasty continues to advance, more consistent, reliable, and effective methods, which also maintain or build up bone stock, will become available.
FIGURE 7-3. A: Radiograph of failed total hip arthroplasty in younger patient with femoral component loosening, large diameter femoral canal, and notable bone loss. B: Radiograph after revision using impaction bone grafting and a short cemented stem. Good bone stock reconstitution has occurred.
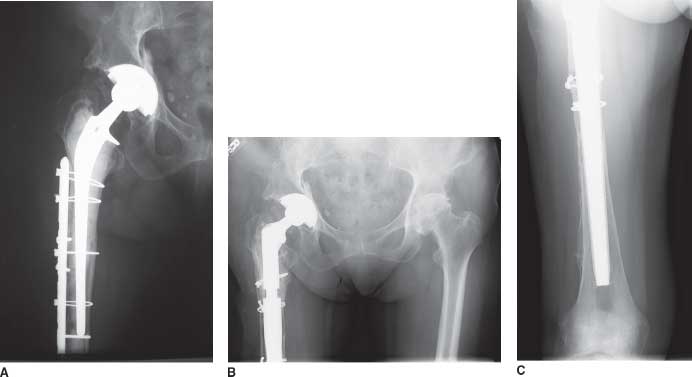
FIGURE 7-4. A: Radiograph of failed total hip arthroplasty with loose long cemented stem in older woman with previous periprosthetic fracture. B and C: Radiograph after femoral revision with long uncemented stem. A very long uncemented stem was chosen to maximize fixation, bypass stress risers from the previous operation, and minimize the chance of another reoperation for femoral side problems.
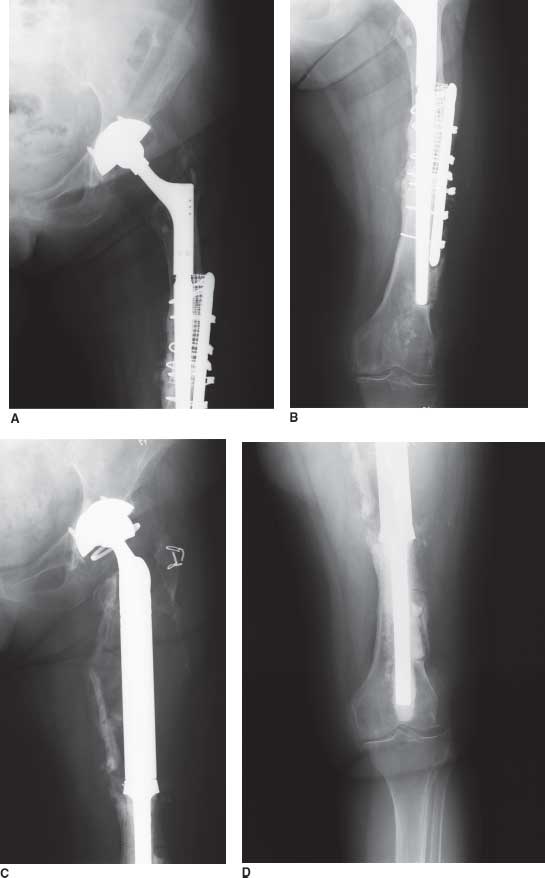
FIGURE 7-5. A and B: Radiographs of hip with loose femoral component and nonunited periprosthetic femur fracture. The patient is elderly and has failed multiple previous procedures. C and D: Hip radiographs after revision total hip arthroplasty using femoral tumor prosthesis and new constrained liner for the well-fixed shell. The procedure with the highest likelihood of immediate success was chosen in this elderly debilitated patient.
OPERATIVE EXPOSURE
A detailed outline of the critical elements involved in choosing the best operative approach for revision total hip arthroplasty is discussed in Chapter 8. The surgeon needs to consider which exposure will be best for implant removal, which will be best to facilitate the planned hip reconstruction, which will provide the best hip stability, and which will provide the best postoperative muscle function and strength.27–29
Exposure in cases of severe acetabular protrusio may be facilitated by a conventional trochanteric osteotomy or a trochanteric slide. Removal of a well-fixed stem—either cemented or uncemented—may be facilitated by extended trochanteric osteotomy. Acetabular reconstruction with either a triflange cup or antiprotrusio cage, both of which extend high into the ilium, may be facilitated by a conventional trochanteric osteotomy, which will protect the superior gluteal nerve. Insertion of an extensively porous-coated stem, particularly if there is varus remodeling of the femur, is facilitated by a lateral extended greater trochanteric osteotomy. Insertion of a long fluted tapered modular stem, which has a straight distal section, is facilitated by an anterolateral extended greater trochanteric osteotomy to provide a straight path down the bowed femur during the reaming process, thereby avoiding distal femoral perforation (Fig. 7-6). Plating of pelvic discontinuity is facilitated by direct access to the posterior column, by either a transtrochanteric approach or a posterior approach. When it is expected that soft tissue tension will be unsatisfactory at the end of the reconstruction, a trochanteric osteotomy, which allows trochanteric advancement and thereby restoration of soft tissue tension, may be considered.30 Finally, if some implants will be retained, the surgeon needs to consider which operative approach will allow him or her to work around the retained implants more satisfactorily and which exposures will best maintain hip stability. Posterior approaches pose greater risk to hip stability when a cup with little anteversion is retained, while an anterior approach may pose a greater risk of anterior instability when a cup with much anteversion is retained.
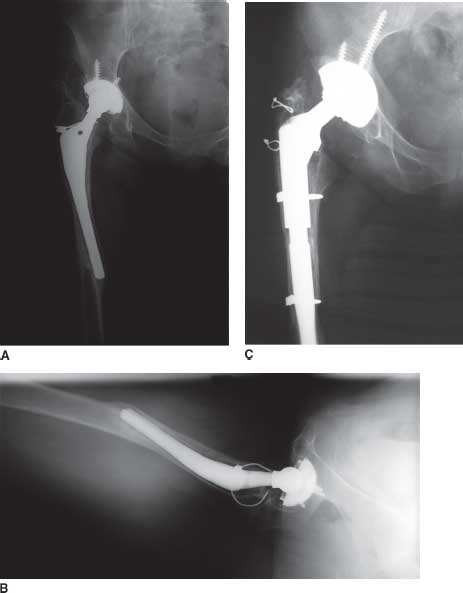
FIGURE 7-6. A and B: Radiographs of failed total hip arthroplasty with loose femoral stem and valgus remodeling of the proximal femur. Valgus remodeling is rarer than varus remodeling. C: Radiograph after revision using an extended greater trochanteric osteotomy. The extended greater trochanteric osteotomy was chosen for two reasons: (i) to simplify failed implant removal and (ii) to facilitate implantation of a longer uncemented stem.
The surgeon must balance advantages and disadvantages of each operative approach. One exposure may facilitate implant removal (e.g., extended greater trochanteric osteotomy) but also may restrict the best types of implants for reconstruction. When choosing between an anterior and a posterior approach, the surgeon also needs to balance the benefits of an anterolateral approach in minimizing posterior hip instability versus the increased risk of poor abductor function and limp associated with anterolateral approaches. Likewise, the advantages of a posterior approach in maintaining abductor strength should be weighed against the greater risk of posterior instability associated with this approach. The benefits of conventional transtrochanteric osteotomy include providing improved exposure but must be weighed against the risks of symptomatic trochanteric nonunion in a specific patient.
RETENTION VERSUS REMOVAL OF EXISTING IMPLANTS
Few decisions are more critical to revision total hip arthroplasty than choosing which implants to revise and which to retain. Implant removal is indicated in almost all cases in which a loose implant is present. Implant removal also is indicated when critical matching parts cannot be properly affixed or matched to the implant (e.g., certain femoral heads). Implant removal is indicated for marked implant malposition. In contrast, implant retention usually is indicated for well-fixed, well-positioned, well-functioning implants that allow the surgeon to perform the operation of choice despite, or because of, their presence.
As a general rule, a well-fixed, well-positioned uncemented cup may be retained, provided a new liner (if needed) of satisfactory inside cup diameter either can be snapped into the shell or cemented into the shell (Fig. 7-7). Well-fixed, well-positioned cemented cups may be retained, provided there is not notable polyethylene wear and provided an acceptable femoral head diameter can be used.
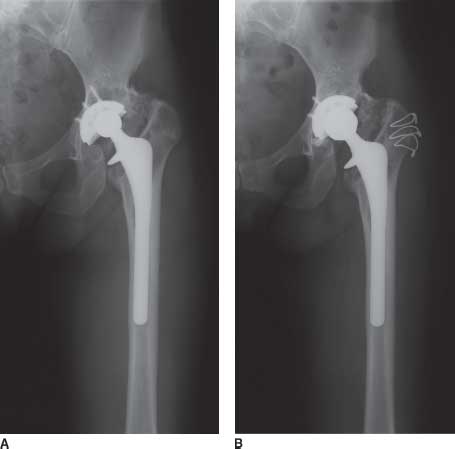
FIGURE 7-7. A: Hip radiograph of the patient with polyethylene wear and periprosthetic osteolysis. The uncemented implants are well fixed to bone. B:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree