Wayne G. Paprosky
Karl Dermingian
Brett Levine
Extensively Porous-Coated Stems
HISTORY OF EXTENSIVELY COATED IMPLANTS
THEORY OF EXTENSIVELY COATED IMPLANTS
POSSIBLE PITFALLS OF EXTENSIVELY COATED STEMS
INTRODUCTION
Total hip arthroplasty has revolutionized the treatment of hip arthritis and is now a predictable surgical technique to relieve pain and improve function. Despite the excellent short-term and long-term clinical results of total hip replacement, revision hip surgery continues to represent approximately 17% of all hip surgeries performed in the United States.1,2 Similar trends for revision hip surgery are seen through-out Europe.3 The incidence of revision hip surgery may increase in the future as the surgical indications broaden, patient longevity increases, and longer follow-up of early-generation implants becomes available.
HISTORY OF EXTENSIVELY COATED IMPLANTS
The proximal and distal bone encountered in a primary hip arthroplasty is generally intact and supportive. The cancellous bed in the metaphyseal portion of the femur allows interdigitation of bone cement into the bony interstices. This cement mantle subsequently provides excellent torsional and axial stability to the implant. Excellent long-term clinical results have been demonstrated with the use of a Charnley-type implant inserted with cement during primary total hip arthroplasty. However, the results of cemented femoral revision have been disappointing. Pellicci et al.4 reported a failure rate of 29% at a mean follow-up of 8.1 years with cemented femoral revision. In this series, the presence of a progressive radiolucency at the bonecement interface was highly predictive of failure. The high rate of failure in cemented femoral revision may be due to the lack of remaining cancellous bone in the metaphyseal and isthmic portions of the femur. Dohmae et al.5 demonstrated that the shear strength at the bonecement interface decreases to 20.6% and 6.8% after the first and second revision, respectively. Katz et al. reviewed the minimum 10-year clinical results of 79 revision hips treated with second-generation cement technique. While the clinical results did appear to improve compared with historical controls, the rate for aseptic femoral revision remained 9.5% while the rate of radiographic femoral failure was 26.1%.
Proximally porous-coated implants have shown similarly poor clinical results when used in revision surgery. This type of implant relies upon the metaphysis and medial calcar to provide axial and rotation stability. However, in the revision situation, the proximal bone is frequently deficient. Berry et al. reviewed the results of 375 femoral revisions, at a mean follow-up of 4.7 years, treated with one of six femoral component designs. The 8-year Kaplan-Meier survival rate was 58% using aseptic femoral revision as the end point, while the survival rate was 45% using aseptic or radiographic loosening as the end point. They concluded, “The damaged, weakened bone often present in the proximal femur during revision probably does not provide an optimal environment for sturdy initial or long-term biologic fixation of these devices that rely on the proximal femoral bone for fixation.”6 Several other authors have demonstrated similarly poor results using a proximally porous-coated stem during femoral revision with failure rates of 10% to 20%.7–9
In 1977, Engh began utilizing a modified Austin Moore straight-stemmed, porouscoated femoral component. The prosthesis was made of cast cobalt-chromium and had a powder-made, sintered, beaded surface of the same material with an initial pore size of 100 mm. In 1980, the pore size was increased to a mean of 250 mm based upon animal research.10 This prosthesis was initially used in younger patients due to the perceived benefit of biologic fixation. In 1982, the first 100 cases were presented to the Food and Drug Administration, and the implant was approved for use without cement in primary hip arthroplasty. In the same year, many stem sizes were made available with porous coating of the proximal 80% of the stem. In 1983, the AML (Anatomic Medullary Locking) stem was made available in distal stem diameters ranging from 9.0 to 21.5 mm, in 1.5-mm increments. The increased use of the AML stem led to the recognition of proximal/distal-sizing mismatch in the femur. This prompted the development of a second stem with reduced medial to lateral dimension (modified medial aspect). This series of changes allowed for improved canal filling both proximally and distally. Modular head and neck segments were then added to the system to further refine the prosthesis, allowing for independent leg-length and offset adjustment. The increased experience of the extensively coated stem in revision surgery along with the early clinical success led to the recognition of the fact that, in the presence of significant damage to the proximal femur, fixation of the stem could be reliably achieved at a more distal level. Longer extensively coated stems were then made available in 205- and 250-mm lengths. Further refinements led to the addition of calcar replacement prostheses.
THEORY OF EXTENSIVELY COATED IMPLANTS
In order to obtain a well-functioning femoral revision, it is imperative that the surgeon obtain an initially stable interface between the prosthesis and the host bone. This can be a challenging task since the femoral bone stock is often deficient, the remaining bone is sclerotic, and the surrounding soft tissue envelope is compromised. Options for femoral reconstruction include stem fixation on the remaining deficient proximal femur, reconstruction of the femoral defect (bone packing, cortical struts, allograft prosthetic composite) or by bypassing the deficient portion of the femur. Extensively coated stems rely upon a “scratch fit” between the cylindrical prosthesis and the remaining host bone in the isthmus. Since the isthmic portion of the femur is generally less deficient than the proximal segment, distal fixation can be reliably obtained during most femoral reconstructions.
Advantages of the cylindrical design of an extensively coated stem include the ability of the surgeon to seat the prosthesis at varying depths depending upon the depth of reaming. Because the proximal bone is not utilized in the fixation of the implant, the stem may be “potted” in patients with severe proximal bone loss. The current recommendation is to underream the femoral canal by 0.5 mm in order to obtain appropriate initial stability. Animal studies have shown that micromotion >150 mm can inhibit bone ingrowth into a cobalt-chromium substrate.11 Clinical results demonstrate that a 4- to 5-cm isthmic segment is all that is required to obtain adequate initial fixation.12
The radiographic characteristics of an extensively coated stem are predictive of implant longevity. Engh et al. observed the changes that occur between 1 and 3 years postoperatively and have described three basic radiographic patterns.13 Extensively coated stems are classified as bone ingrown, stable fibrous fixation, or unstable fixation.
The bone ingrowth pattern is characterized by the absence of migration of the implant, absence of radiolucent line around the porous portion of the stem, absence of endosteal hypertrophy at the distal limit of the porous coating, and no pedestal formation. Proximal bone resorption “stress shielding” is seen with extensively coated components since most ingrowth occurs distally on the stem, and as a result, the proximal femoral bone is not loaded.
The second radiographic pattern of fixation is fibrous ingrowth. The component demonstrates no subsidence; yet a parallel reactive line adjacent can be seen adjacent to the porous coating. The char-acteristic feature of this line is that it parallels the contours of the implant, is separated from it by a narrow width (usually 1.0 to 1.5 mm), is not divergent, and does not progress with time. A small distal pedestal and mild proximal bone resorption may be present.
The final radiographic pattern of an unstable implant is characterized by progressive implant migration, rotary instability, and tilting of the component into varus. Progressive, divergent, sclerotic lines are seen, and the proximal bone demonstrates hypertrophy. An endosteal pedestal is frequently present at the tip of the stem. With these radiographic characteristics, the implant is grossly unstable and clinically symptomatic.
INDICATIONS
The most frequent indications for femoral revision include aseptic loosening, recurrent instability from a malpositioned component, component fracture, delayed infection, and the need for improved acetabular exposure. Relative indications for femoral component removal include progressive distal femoral osteolysis or during acetabular revision when a femoral component with a poor track record had previously been placed. The choice of implant used during the femoral reconstruction will be based largely upon the amount of femoral bone loss encountered at the time of revision surgery. Depending upon the clinical scenario, an extended trochanteric osteotomy may be required to facilitate component removal, remove distal cement, or avoid eccentric remaining in a varus remodeled femur.
The senior author has previously described a femoral classification system that can assist the surgeon with preoperative planning for femoral revisions and can predict the extent of bone loss. This clas-sification places the remaining femoral bone stock into one of four defect types. Type I defects have minimal damage to the proximal metaphysis and can be treated like a primary hip. Type II defects demonstrate mild metadiaphyseal bone damage with an intact diaphysis. Type III defects have significant metadiaphyseal damage with Type IIIA allowing >4 cm and Type IIIB allowing <4 cm of “scratch fit” at the isthmus. Type IV defects are characterized by extensive metadiaphyseal damage with thin cortices and a widened femoral canal.
The majority of femoral revisions demonstrate moderate proximal bone deficiency with an intact isthmus (Type II or IIIa defects). These defects can be adequately reconstructed with an extensively coated implant. The length of the implant is predicated upon the extent of bone loss. Because stable fixation can be obtained with 4 to 5 cm of “scratch fit,” most Type II defects can be reconstructed with a 6-in stem, while most Type IIIa and IIIb defects require either an 8- or 10-in stem (Fig. 25-1A,B).
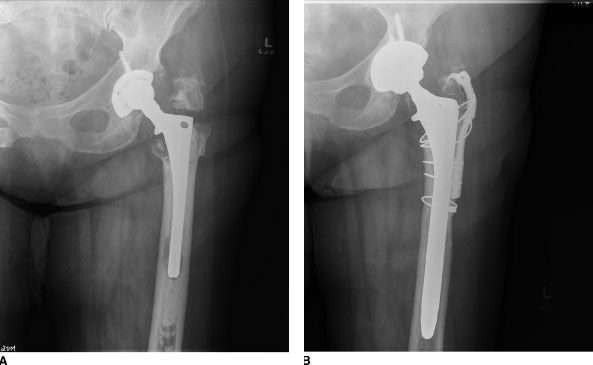
FIGURE 25-1. Seventy-six-year old patient with aseptic loosening of her femoral implant. A: Preoperative radiograph demonstrating proximal bone loss. The femur has >3 cm of isthmus remaining (Type IIIa femoral defect). B: Femoral reconstruction with an 8-in extensively coated femoral implant.
CONTRAINDICATIONS
The use of an extensively coated stem is a relative contraindication in patients with capacious femoral canals that do not allow initial stability. The authors reviewed 51 patients with either a 10- or 9-in cal-car fully porous-coated stem, at an average 6 years postoperatively. The mechanical failure rate among the 9- and 10-in fully porous-coated stems was 0% in Type III B defects with femoral canals <19 mm (15 patients), 18% in Type IIIB defects with femoral canals >19 mm (2 of 11 patients), and 37.5% in Type IV defects (3 of 8 patients). We hypothesize that the lack of isthmic bone and the often ectatic femoral canals do not allow intimate apposition of the implant against the bone. Therefore, the surface area for bone ingrowth is de-creased, and component micromotion can occur.14 The senior author now believes that an exten-sively coated stem is relatively contraindicated in Type IV femoral defects and in Type IIIB patients with femoral canals >19 mm.15 Additional contraindications to the use of an extensively coated stem are in patients who require a bowed 8- or 10-in stem with associated severe femoral torsional remodeling. Femoral remodeling in varus and retroversion is frequently observed at the time of revision, especially in loose cemented implants. The anterior femoral bow will dictate the amount of anteversion that can be obtained with the use of a bowed femoral stem. Because of the remodeling in retroversion, the stem frequently cannot be placed in an anatomic position. Component malposition with decreased femoral anteversion may result in re-current posterior instability.
SURGICAL TECHNIQUE
Exposure Similar to other surgical procedures, adequate preoperative planning is essential for a successful surgical outcome. Standard anteroposterior (AP) and lateral radiographs of the hip including all of the prosthesis and cement along with an AP pelvis are necessary. If the femoral component ap-pears to be well fixed, a large distal cement mantle is present, or if there is significant femoral varus remodeling, an extended trochanteric osteotomy should be anticipated. It is imperative that an oscillating saw, pencil-tip burr, several wide osteotomes, trephines, Gigli saw, metal-cutting burr, and cerclage wires be available in the operative suite.
The surgical approach in the revision setting may be directed by previous surgical incisions. In general, a posterior lateral approach is used to facilitate visualization of both the femur and the acetabulum. This approach will also allow extension both proximally and distally if needed. Once the femoral component is exposed, the stability of the implant is assessed. If the stem is grossly loose and the greater trochanter is not preventing extrication, the component is removed. However, if the trochanter is preventing component removal or if the stem is well fixed, an in situ extended trochanteric osteotomy is performed.
Bone Preparation It is imperative that the surgeon be able to concentrically ream the remaining diaphyseal bone. If the femur has undergone varus remodeling, an extended trochanteric osteotomy is required in order to avoid perforation of the lateral cortex. The femoral canal is sequentially reamed with straight reamers until cortical resistance is encountered. The femoral canal is underreamed by 0.5 mm in rela-tion to the actual implant. Underreaming of the canal allows axial and rotation stability once the slightly larger implant is inserted. Throughout the reaming, the surgeon should be aware of the depth and the approximate location of the new stem. A minimum of 5 cm of diaphyseal bone, “scratch fit,” is required when utilizing a fully porous-coated stem. Alternative methods of reconstruction should be considered if this is not feasible. Once significant endosteal resistance is encountered with the reamers, a femoral trial can be placed. The hip can then be reduced and examined for stability. Provided the hip is stable, the amount of required femoral anteversion is marked. If an 8- or 10-in bowed stem is utilized, the bow of the femur and the prosthesis will control the ultimate amount of femoral anteversion. If the hip is not stable in this configuration, alternative methods of reconstruction such as a modular stem should be considered. When using an 8- or a 10-in bowed stem, the femur is reamed with flexible reamers. The bow of a curved stem generally requires reaming line-to-line in order to safely insert the prosthesis. The surgeon must be cognizant while reaming to avoid anterior femoral perforation due to the anterior femoral bow along with the often hypertrophied posterior cortical bone.
Prosthesis Implantation The placement of a fully porous-coated stem in the revision situation is similar to that used during primary arthroplasty. A hole gauge should be used to verify that the manufacturing process has resulted in the appropriate distal femoral diameter (e.g., a 18-mm component should be able to pass through the 18.25-mm hole and not the 18.00-mm hole). The implant dimension should be compared to the last femoral reamer and should ideally be oversized by 0.5 mm. If the femoral component is relatively oversized, the femoral canal can be reamed an additional 0.5 mm to avoid femoral fracture during insertion. A series of gentle blows are used to seat the implant. The stem should advance with each strike of the mallet. Care must be taken to maintain the appropriate anteversion of the stem during the insertion.
A prophylactic cerclage cable can be placed distal to the osteotomy site prior to insertion of the implant to avoid inadvertent fracture due to the relatively high hoop stresses at the level of the osteotomy.
RESULTS
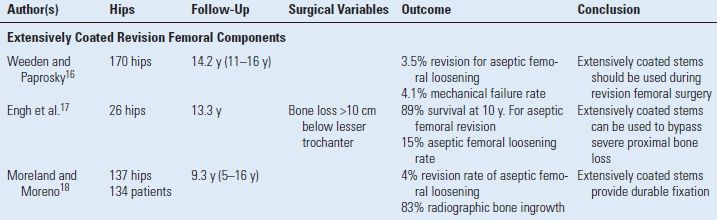
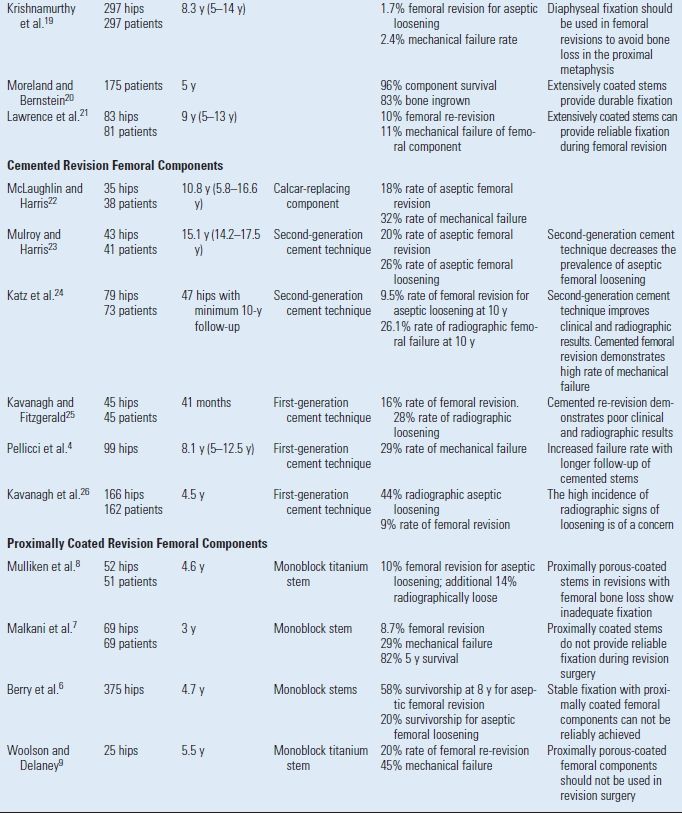
Femoral revision with the use of extensively coated stems has demonstrated excellent clinical and radiographic results (Table 25-1).
The senior author reviewed 297 hips with a mean follow-up of 8.3 years (range, 5 to 14 years) in patients who underwent revision total hip arthroplasty using the extensively coated AML (DePuy, Warsaw, IN) prosthesis. All patients were evaluated radiographically and clinically at a minimum of 60 months.
TABLE 25.1 Outcome of Femoral Revision
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








