CHAPTER 4 Implant Choices: The Biomechanics of Anchors and Sutures
HISTORY
Before the development of suture anchors, the attachment of ligament or tendon to bone was accomplished by first creating a bone tunnel and then passing sutures through the bone tunnel. Awls or drills were used to create the bone tunnels. Suture was passed through the tunnels and then tied over the bone bridge. This technique worked relatively well for open procedures, but could not be used for arthroscopic repairs.1 As surgeons attempted to do more through less invasive surgeries, the first-generation suture anchor was introduced by Mitek, called the G1 anchor.2 This anchor gave the surgeon the ability to attach a suture to bone without having to create a bone tunnel.
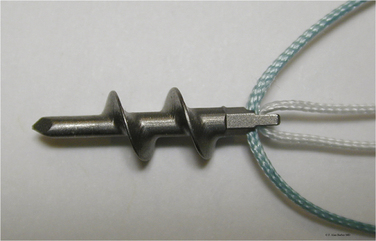
The first screw-in suture anchor was developed about the same time as the G1, called the Statak anchor. This anchor was designed by Marlowe Goble and had a suture secured in the center of a screw anchor.1 Since the introduction of these original suture anchor designs, dozens of different screw-in and non–screw-in anchors have been developed. All these anchors are designed to achieve the goal of attaching a suture to bone.
SUTURE ANCHORS
There are many suture anchors on the market today. In general, they can be classified as screw-in or and non–screw-in anchors. To assist with the selection of the proper anchor, it is important to understand the basic biology of tissue healing. The three main phases of tissue healing have been summarized by Barber and Boothby1 and progress from inflammation through repair and finally tissue remodeling. Initially, inflammatory cells fill the gaps between the tendon and the bone. The inflammatory cells gradually become organized and are then invaded by a vascular supply, which aids in the removal of debris and the formation of collagen-forming cells. These cells act to close the tissue gap. This entire process takes at least 12 weeks, but is likely to vary according to the specific tissue in question, as well as the patient’s preinjury metabolic status and inherent vascularity.3 A surgeon must select an anchor that will hold the tissue in close enough proximity to the bone so that gapping does not occur before the final phases of tissue healing can occur.
A good suture anchor has several characteristics, which have been outlined by Barber and colleagues.1,4,5 The suture anchor should do the following: (1) fix the suture to bone; (2) not pull out of the bone with stress; (3) be easy to place surgically; (4) allow for arthroscopic knot tying; (5) have the capacity to hold multiple sutures; and (6) not cause long-term morbidity. Some of the specific anchor qualities that should be considered include the size and shape of the anchors, type and location of the eyelet in the anchor, anchor material, method of insertion, and method of failure (Box 4-1).3 Barber and associates have carried out a number of studies on the fixation strength of various suture anchors and their modes of failure and have recently published updates with information on the latest designs.6,7
Anchor Size
Suture anchors come in many different sizes. Both the diameter of the outside of the anchor and the core of the anchor should be considered.1,5 Historically, larger screw-in anchors with deep threads were the anchor of choice in humeral heads that were osteoporotic. However, newer non–screw-in anchors with smaller diameters may show comparable strength,3 although anchor performance is affected by the quality of the bone, which can be a significant concern, especially in older patients. For rotator cuff repairs, the larger suture anchors are advantageous because they can hold more sutures than smaller anchors. Very large suture anchors (6.5 mm and larger) cause crowding and limit the placement of all the anchors in ideal locations. Therefore, with the improved strength of smaller diameter anchors, these extremely large anchors are often not practical.4
When placing sutures into the dense bone of the glenoid for labral repairs, smaller anchors may have an advantage because they are less likely to cause significant damage to the articular cartilage.1 The limitation is that they are often not able to accommodate as many sutures per anchor.
Anchor Type
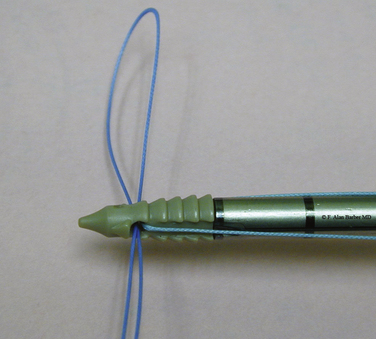
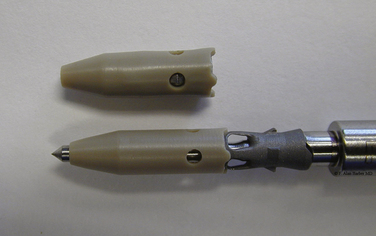
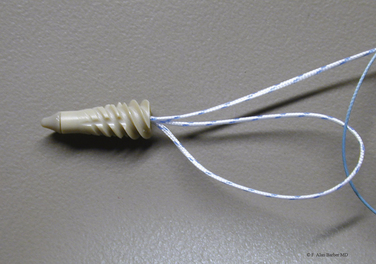
Anchors come in several different shapes. In general, they can be divided between screw-in and non–screw-in designs (Figs. 4-1 and 4-2). As described by Barber,4 non–screw-in anchors are those that toggle, push in, or change their morphology after being pushed into the bone (Fig. 4-3).
Another variation is an anchor that works more like a tack. These have a bar or disk attached, which holds the tendon on the bone. There are several disadvantages of these designs. They often create a larger hole in the tendon and are usually very difficult to remove once they are placed in the bone.1 They do, however, eliminate the need to pass sutures through the tissue or tie any knots.4
Screw anchors are a good anchor choice for the osteoporotic bone of the humeral head and tuberosity. The screw in anchors typically have high load to failure strength. However, Pedowitz18 has demonstrated that even screw-in anchors can have significant translation in the humeral head after cyclical loading, particularly when load is applied oblique to the angle of anchor insertion, which is the physiologic direction of loading with a rotator cuff repair. Many of the suture anchors, both screw-in and non–screw-in, now allow easy movement of the suture through the eyelet so that sliding knots can be used. Many anchors have eyelets large enough to allow multiple sutures to pass and some allow the surgeon to change out the suture if they desire.4
Anchor Eyelets
The shape of an anchor’s eyelet is another important consideration. The eyelet can be a potential site of anchor failure.4,9 The rotation of the eyelet in relationship to the line of force has been shown to affect suture fretting and load to failure force.10,11 This may be more pronounced with metal suture anchors because the eyelets might have sharp edges that can contribute to suture failure if the alignment of the suture and the eyelet is not correct.3
Many anchors now have two or more sutures loaded into them. To accommodate multiple sutures, different eyelet designs have been used. These designs include a long vertically oriented eyelet, a wide horizontally orientated eyelet, or a distal cross bar.4 The horizontal eyelets make it easier to tie sliding knots with both sutures. Some designs have been introduced that have eyelets made from a braided flexible suture. To avoid the problem of having multiple sutures binding up inside the eyelet, some anchors have two independent suture channels, which can be at different angles to each other or on different sides of the eyelet column.
Anchor Material
Metal and biodegradable anchors are used frequently. Recently, there has been a trend toward the development of more biodegradable anchors. The benefits of metal anchors have been summarized by Barber and Boothby.1 These anchors provide good strength and are relatively easy to insert, and can easily be evaluated with x-ray.
Modern biodegradable anchors have pull-out strengths similar to those of metal anchors and are just as easy to insert.12–14 As noted, the eyelets of biodegradable suture anchors may be associated with less damage to the suture, regardless of whether the suture is damaged.15 Barber and Boothby have noted other benefits associated with biodegradable anchors.1 They are easier to revise, can be used in pediatric patients, eventually resorb, and produce less artifact with magnetic resonance imaging (MRI). Overall, newer biodegradable anchors are becoming easier to use and provide excellent pull-out strength.16
Most of the bioabsorbable anchors are made out of polyglyconate (PGA) or poly-L-lactic acid (PLLA).1 Some are hybrid and are composed of PGA and PLLA. Each polymer behaves in a unique fashion. PGA has been linked to complications, including restricted shoulder motion and a hyperinflammatory response.1 PLLA can take up to 4 years to resorb completely and the problems reported with these implants have been primarily mechanical. A recent study of the use of PLLA anchors in labral repairs has demonstrated postoperative enlargement of drill holes that were filled with these anchors and a correlation with less favorable results in function and stability.17 However, another study, which followed patients for 7 to 8, has years noted that the drill holes used for the placement of PLLA anchors healed in most patients.18
Recently, nonbioabsorbable and nonmetallic materials have been introduced in suture anchors. Polyetheretherketone (PEEK) is a chemically resistant crystalline thermoplastic that maintains its integrity in a wide pH range. It withstands high temperatures and can be found in automotive, aerospace, and industrial applications. As a suture anchor, it creates a nonabsorbable, strong, radiolucent anchor that may be drilled out during revision surgery. However, radiolucent anchors (absorbable or nonabsorbable) may be difficult to localize if they become dislodged at some point after surgery; this is important, because these anchors can cause significant injury to articular cartilage and other periarticular tissues (Figs. 4-4 and 4-5).
It is important for the bioabsorbable implants to retain their strength during the critical phases of tissue healing. Clinically, they appear to do this.18 Once healing has occurred, other factors, including bone-implant reactions and the potential for loose body formation caused by implant breakage, become more important.8
Anchor Placement
In the past, surgeons were satisfied if they could get the tendon near the bone attachment site without a lot of tension. Recent appreciation and understanding of margin convergence and the interval slide technique have made it easier for surgeons to reattach the rotator cuff to the footprint on the greater tuberosity.4
Barber has outlined the different options for the placement of anchors to achieve attachment over the footprint.4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree